Inspired by a passion for improving lives through oral health, Glidewell Clinical Education provides contemporary, continuing education for dental professionals. Read our chief publication, Chairside® magazine, for cutting-edge clinical techniques and industry news, or take a free online CE course to expand your skillset. Listen to our “Chairside Live: Dental Insights” podcast or check out our library of over 10,000 education videos.
Dental Education
-
 Online CE CourseIntroduction to Digital Dentistry for the Dental Auxiliary
Online CE CourseIntroduction to Digital Dentistry for the Dental Auxiliary -
 Online CE CourseIntroduction to Dental Sleep Medicine
Online CE CourseIntroduction to Dental Sleep Medicine -
.png/_jcr_content/renditions/thumb-png-mobile-full.png) Online CE CourseImplant Treatment Planning: The Contributing Factors
Online CE CourseImplant Treatment Planning: The Contributing Factors -
 Online CE Course4 Ways to Provisionalize Dental Implants
Online CE Course4 Ways to Provisionalize Dental Implants -
 Online CE Course10 Things I Learned the Hard Way
Online CE Course10 Things I Learned the Hard Way -
 Online CE CourseGuided Bone Regeneration: 8 Steps to Successful Ridge Augmentation
Online CE CourseGuided Bone Regeneration: 8 Steps to Successful Ridge Augmentation -
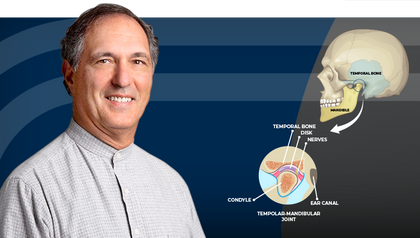 Online CE CourseTemporomandibular Disorders and the Human Jaw
Online CE CourseTemporomandibular Disorders and the Human Jaw -
 Online CE CourseRestoration of Implant Overdentures
Online CE CourseRestoration of Implant Overdentures -
 Online CE Course11 Steps to Increase Practice Production Right Away – Part 2
Online CE Course11 Steps to Increase Practice Production Right Away – Part 2 -
 Online CE CourseUsing Laboratory-Fabricated Provisionals
Online CE CourseUsing Laboratory-Fabricated Provisionals
-
 Online CE CourseNext-Level Chairside Esthetics: Customizing Restorations with Stain, Glaze, and Finishing TechniquesIn this course, Dr. Justin Chi demonstrates how to elevate chairside restorations using advanced staining, glazing, and finishing techniques for monolithic restorations.
Online CE CourseNext-Level Chairside Esthetics: Customizing Restorations with Stain, Glaze, and Finishing TechniquesIn this course, Dr. Justin Chi demonstrates how to elevate chairside restorations using advanced staining, glazing, and finishing techniques for monolithic restorations. -
 Online CE CourseEsthetic Veneer Preparations: From No Prep to Full PrepIn this course, Dr. Danielle Brown provides a practical overview of veneer preparation techniques from no-prep, minimal-prep and traditional-prep veneers with step-by-step protocols.
Online CE CourseEsthetic Veneer Preparations: From No Prep to Full PrepIn this course, Dr. Danielle Brown provides a practical overview of veneer preparation techniques from no-prep, minimal-prep and traditional-prep veneers with step-by-step protocols. -
 Online CE CourseBonding and Temporizing Protocols: Tips for VeneersIn this course Dr. Danielle Brown offers practical guidance on veneer temporization and bonding techniques to improve patient comfort and clinical outcomes.
Online CE CourseBonding and Temporizing Protocols: Tips for VeneersIn this course Dr. Danielle Brown offers practical guidance on veneer temporization and bonding techniques to improve patient comfort and clinical outcomes.
The best educational resource in the dental industry