Related Dental Sleep Medicine Articles
- “Dental Sleep Medicine: Should You Become a Medicare DME Supplier?” by Randy and Kyle Curran, Pristine Medical Billing
- “What Is Obstructive Sleep Apnea?” by Randy Clare, Glidewell
800-854-7256 USA
Follow these pointers to secure reimbursement for sleep apnea therapy.
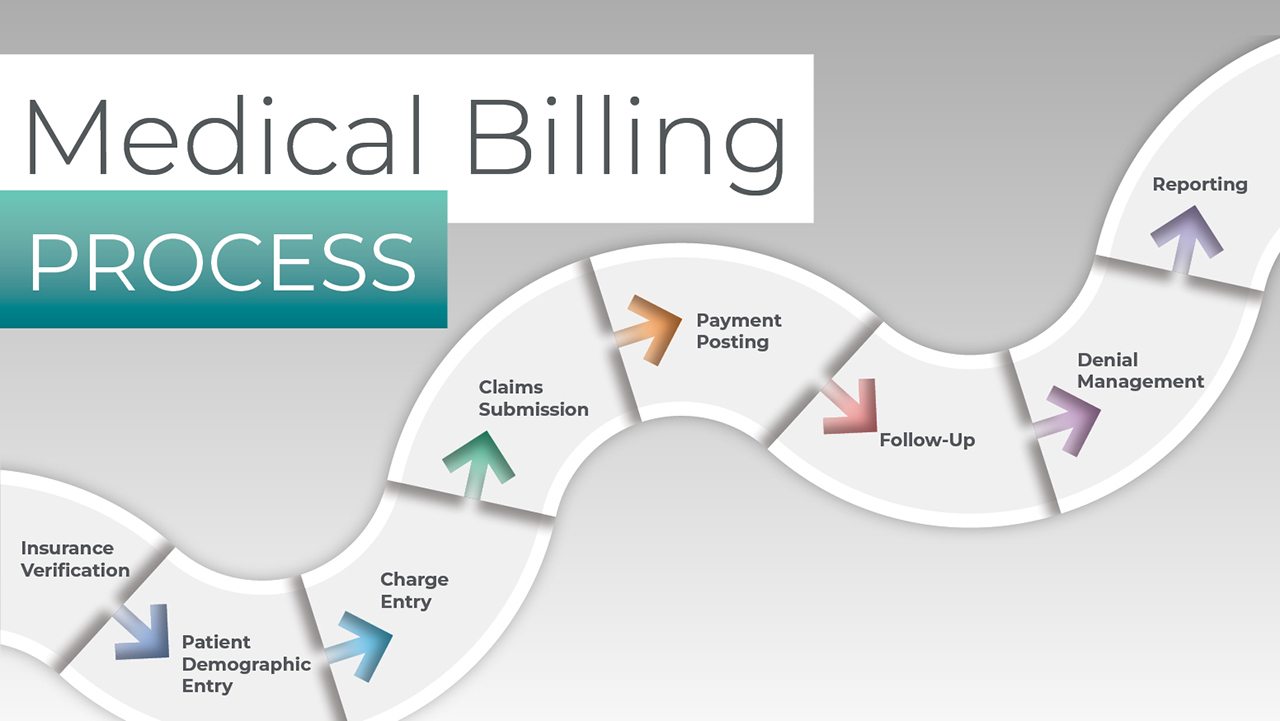
Dentists often ask if medical insurance can be billed for dental treatments that address conditions that affect the patient’s general health. The short answer is yes, but consider the following:
Medical insurance can cover treatment in the dental office. Reimbursed therapies include implants that are a medical necessity, trauma cases, temporomandibular disorder (TMD) treatments, oral appliance therapy for sleep apnea treatments, biopsies, and imaging related to these procedures. Sleep apnea therapy is the most consistently reimbursed medical treatment provided by dentists.
There are very specific methods and best practices that every dental office needs to follow when billing medical insurance. Randy Curran from Pristine Medical Billing took the time to answer a selection of questions that often come up when discussing medical billing for dental sleep medicine.
Why are sleep apnea treatments more consistently paid than implant or TMD treatments?
Randy Curran: As opposed to implants, there is no debate whether sleep apnea is a medical or dental condition. There is also rarely an exclusion to a sleep appliance with an insurance plan, but some insurance plans do exclude the TMD appliance. Also, sleep apnea treatments can usually be covered at the in-network level, even if the dental practice is out of the insurance network. Using the lower in-network deductible results in a better payment from the insurance carrier in addition to the deductible being satisfied many times by the sleep test prior to treatment.
What are some of the biggest hurdles to implementing sleep services for patients?
RC: There are a few barriers to overcome, but today it is easier than ever with new telemedicine guidelines and easier access to sleep physicians. The first barrier is the practice itself. Often, practices will start a sleep program without the correct guidance and also leave their staff responsible to implement a new program without adding any extra payroll hours. Many times, we see practices’ newly added sleep services fail simply because the staff doesn’t have enough time to run the everyday aspects of the practice and also implement a new program that is completely foreign to them.
Another way the practice will sabotage itself is by setting expectations too high for reimbursement from the medical insurance carrier. These practices think that they need to make $3,500 or more per treatment, and that will price many patients out of the treatment as the average insurance pays around $2,100. This leaves the patient with a bill of at least $1,400, depending on their deductible. Most successful practices can flourish with a per-treatment profit of around $2,500, which will help a lot more patients afford the treatment.
Do I need to find medical doctors in my area to refer patients to me before I start a dental sleep medicine program?
RC: While that would be ideal, it’s not usually realistic. Most of the successful practices that we work with started by treating their own patients for the first year and grew the program organically. Then, by year two, and after many effective treatments, they would go out and start trying to build relationships with local M.D.s. Many were also sending letters throughout the first year to the patient’s medical doctors to keep them in the loop of the therapy. This policy gains the trust of the medical community. In summary, start small and understand that it is a gradual process that may take at least a couple of years to build up.
If I start screening my own patients, what is the best way to help them get tested for sleep apnea?
RC: This will depend upon your state and the patient’s insurance. Many states do not have any restrictions on dental practices ordering or sending patients home with a sleep-testing device. So, one option may be to purchase a sleep-testing device and use it as a cash pay model, then have the study interpreted by a sleep physician. This is good, as the patient can take it home directly from the practice.
Another option would be to use a national home sleep testing company that can connect the patient to a sleep physician via telemedicine and then ship the sleep testing device directly to the patient after the telemedicine consultation. This option is also good, as some insurance carriers do require a face-to-face visit with a physician. It may also be beneficial if the sleep study can be billed to the insurance carrier, as sometimes the patient can be tested at little to no out-of-pocket cost.
Do insurance carriers accept home sleep testing results when approving the pre-authorization for oral appliance therapy?
RC: Yes, insurance carriers have approved these tests for many years now, and they will qualify the patient for treatment. This is the case even with Medicare, if the test is given by a Medicare-approved testing provider (this does not include a dentist enrolled with Medicare) and there is a face-to-face visit with a physician prior to the test.
How recent should a sleep study be to qualify a patient for therapy?
RC: Most private insurance carriers want to see the test be no older than two years, though sometimes we can stretch that to three years with an appeal. Medicare tests need to be performed within the past year.
What other documents are needed to qualify a patient for sleep apnea treatment with an oral appliance?
RC: Most carriers at minimum want to see the qualifying sleep test; an Rx, LOMN (letter of medical necessity) or recommendation on the sleep test from an M.D. for oral appliance therapy; and a document showing a dental exam was completed and the patient is a good candidate for the treatment. Additionally, if the patient has mild sleep apnea, documentation may include an Epworth Sleepiness Scale score at 11 or higher showing daytime fatigue or associated comorbidities. If the patient has severe sleep apnea, documentation may include a trial and proof of CPAP or BiPAP failure. There are a couple of carriers that will also require a face-to-face consultation with a medical doctor or sleep physician.

Insurance providers may require specific documentation for qualifying a patient for sleep apnea treatment with an oral appliance.
How long does a pre-authorization take, and will the medical insurance disclose how much it will pay for the treatment after it approves the treatment?
RC: It will typically take about two or three weeks for the pre-authorization approval. Most patients need a pre-authorization or a gap approval to help reduce their cost. A gap approval is when the insurance has a gap in coverage with a deficiency of in-network providers and allows the patient to see an out-of-network provider while using the better in-network benefits (lower deductible and cost share). This is allowed if there aren’t any in-network dental sleep medicine providers within a 30-mile radius of the patient’s home. The insurance will not tell you how much they will pay unless you have a contract with the carrier. They might send over a single case agreement that will show this, but this isn’t very often. In order to accurately quote patients their out-of-pocket cost, the practice must be contracted or hire a third-party billing service that has the data from the insurance carrier’s past payments under the plan.
How long do medical insurance claims take to pay out?
RC: Many claims should pay within six to eight weeks once you are in the insurance system. The first couple of payments from a carrier may take 12–14 weeks, as the carrier needs to put the practice into the system using the W-9 form prior to claim adjudication. The key for faster payments is to send the claims electronically through a robust clearinghouse and to call on the claims weekly to ensure no further clinical records are needed to process the claim. Many medical providers use poor-performing clearinghouses, which greatly affects the timing of the claim payments.
Should I become an in-network provider with medical insurance carriers or stay out of the network?
RC: This depends on your area of practice. If there is an in-network dental sleep medicine provider within 20–30 miles of your practice, it would probably be best to become an in-network provider, as the insurance carrier is going to try to drive the patient to the other provider during the pre-authorization process. It will also be very difficult to obtain a gap approval to use the patient’s lower in-network deductible.
If there are no in-network competitors nearby, then the practice can stay out of the insurance network and obtain gap approvals to get the best of both worlds.
What is the average in-network rate to treat sleep apnea with an oral appliance?
RC: This ranges between $1,700 and $2,500 depending on the carrier and region. Some states are even lower with Blue Cross Blue Shield plans. There are other non-covered cash pay items that practices can add to the treatment to increase the total reimbursement of the treatment for some of the lower paying contracts.
If I stay out of the insurance network, will the insurance company send the payment to me or the patient?
RC: Most carriers will send the check to the provider, regardless of whether they are in or out of the network. The exception would be some of the Blue Cross Blue Shield plans in certain states and maybe some smaller local carriers like Medical Mutual of Ohio.
Should I become a Medicare DME provider for dental sleep medicine services?
RC: This depends on your patient demographics and if you are going to market yourself to the medical community down the road. Many providers enroll as a Medicare nonparticipating DME provider and charge the patient a fee up front, and the patient will be reimbursed directly from Medicare. The Medicare allowable ranges from $1,100 to $1,950 depending on the state. Some Medicare patients have a supplemental insurance that will at times pay the entire charge amount. These checks will go to the patients, so the practice must have a good collection protocol to ensure the patient pays all of the payments from both Medicare and the supplemental.
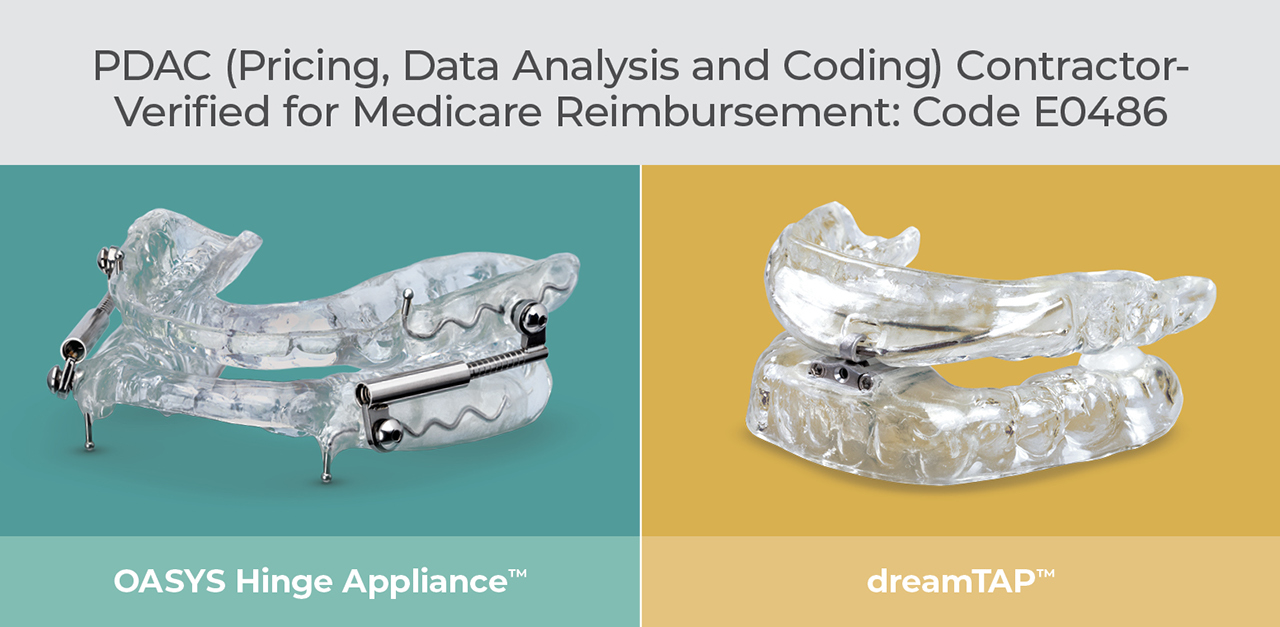
Both the OASYS Hinge Appliance™ and dreamTAP™ appliance are eligible for Medicare reimbursement under code E0486.
What is your advice for dentists interested in implementing dental sleep medicine into their practices?
RC: Make sure you partner with trusted companies. Give your staff plenty of time to start and run the program. Select a go-getter as the leader of the program. Set realistic financial goals to ensure patients can afford the treatment; $2,500 seems to be the sweet spot in most areas. Think of patient care first and understand it’s a volume game in the end. Don’t expect medical insurance to be the magic wand; rather, think of it as a way to supplement the cost to the patient. Last, but not least, be very patient with the process as it can take years to get to the goals most practices want to reach.
To discover the simple, three-step process to screen and treat patients for snoring and sleep apnea, visit glidewell.com/pmad.
Related Dental Sleep Medicine Articles
OASYS Hinge Appliance is a trademark of Dream Systems LLC. dreamTAP is a trademark of Airway Management Inc.
Send blog-related questions and suggestions to hello@glidewell.com.


