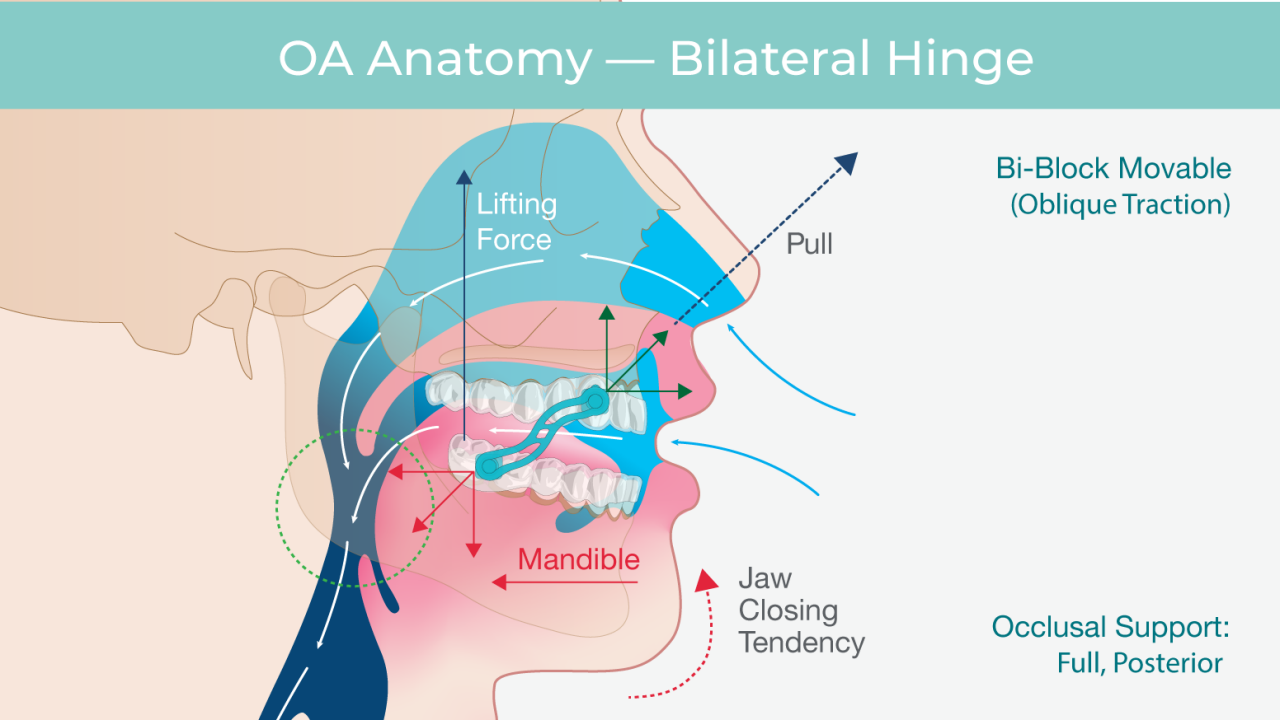
It is impossible to discuss sleep apnea solutions without describing the physical condition that we know as obstructive sleep apnea. As a person falls asleep, the tissues of the upper airway begin to lose their tone. As they relax, the cross-sectional area of the airway begins to collapse. As each breath draws air through this narrow airway, the tissues vibrate and make the snoring sound. As the tissues further relax, the airway can collapse completely, obstructing airflow.
OSA sufferers experience repeated drops in oxygen saturation, which affects the heart and vascular system. During these periods of low oxygen, heart rate increases with a corresponding increase in blood pressure. The body responds by secretion of hormones related to stress and increasing the production of compounds that produce inflammation.
The physiologic response to the stress associated with OSA is to awaken to a lighter sleep state. This lighter sleep state allows tone to return to the tissues of the upper airway, restoring the larger airway cross-section to normalize breathing. This cycle can happen dozens of times per hour of sleep. The lack of deep restorative sleep will leave the patient feeling tired and unrefreshed in the morning.
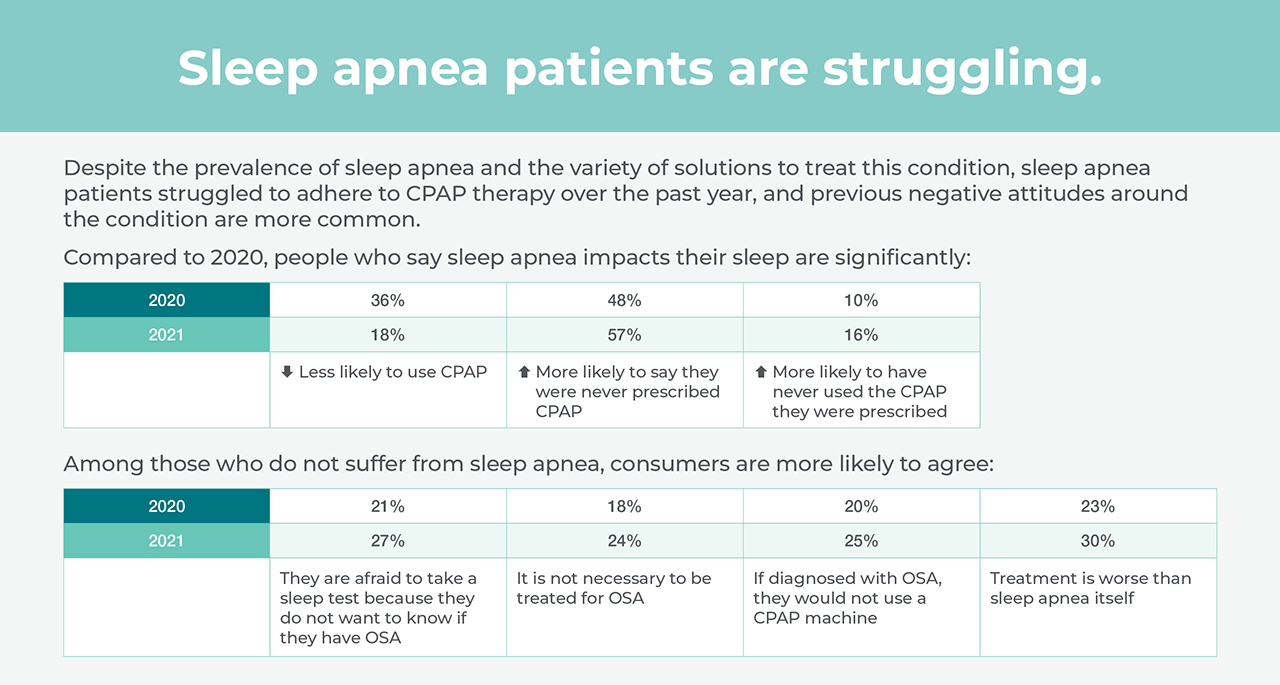
As mentioned above, most patients are unaware that they suffer from OSA. When patients do seek sleep apnea treatment, it has been shown that their primary motivations are bed partner disturbance and excessive daytime sleepiness.
It is important to understand when considering OSA that not all patients with OSA snore, but all snorers experience some OSA. Excessive daytime sleepiness is diagnostic of OSA and is a key screening criterion for the condition.