Photo Essay – Utilizing Digital Impressions and Chairside Mills

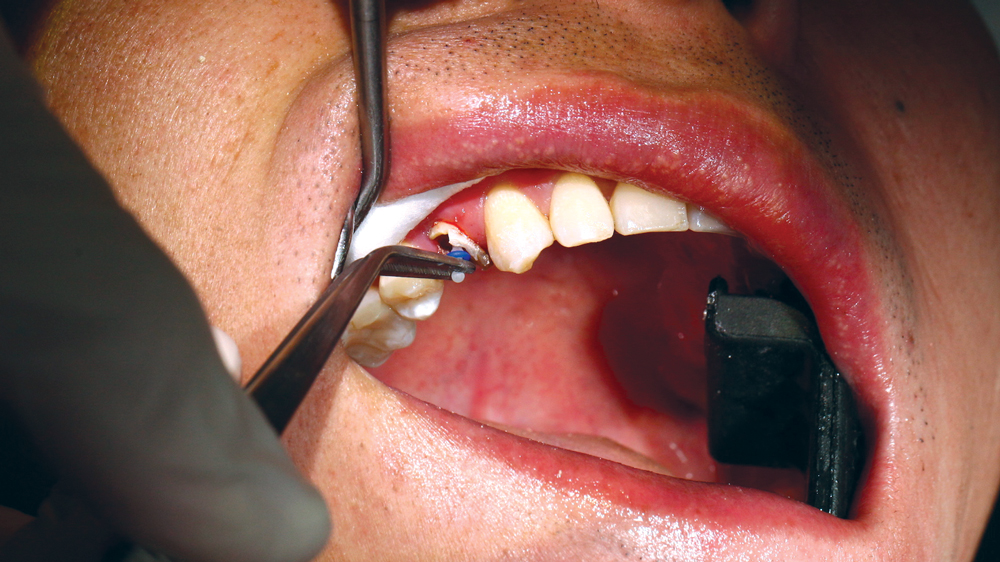
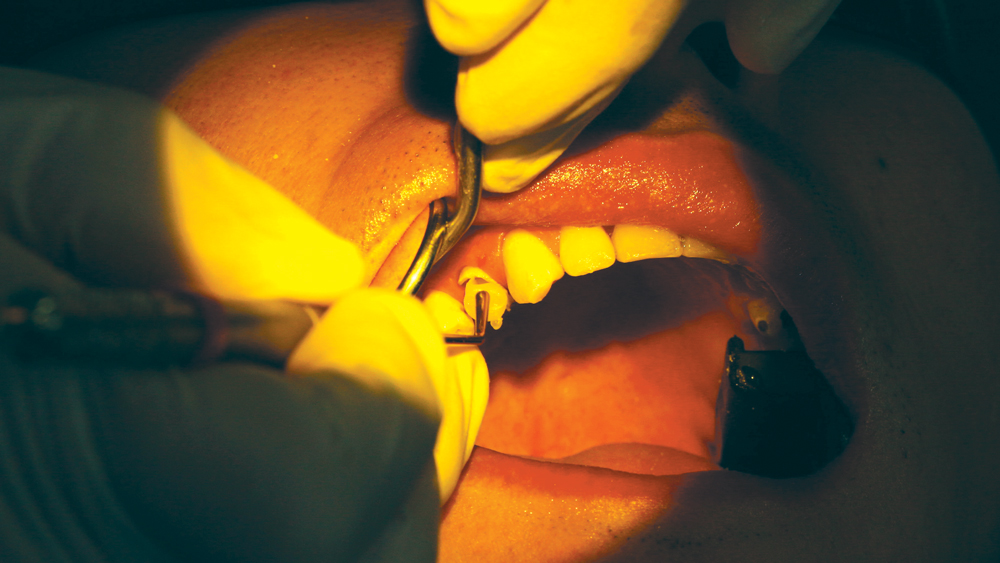
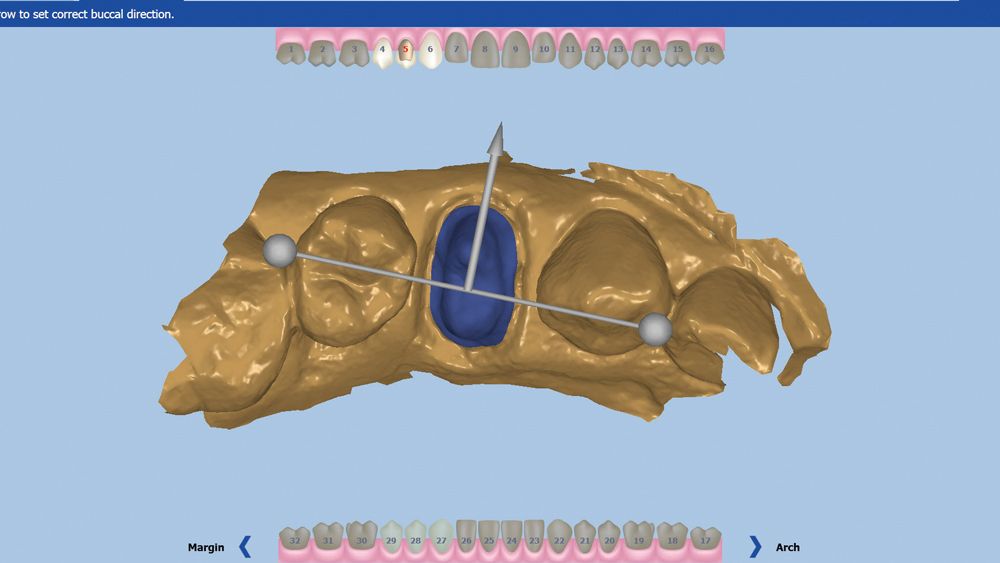
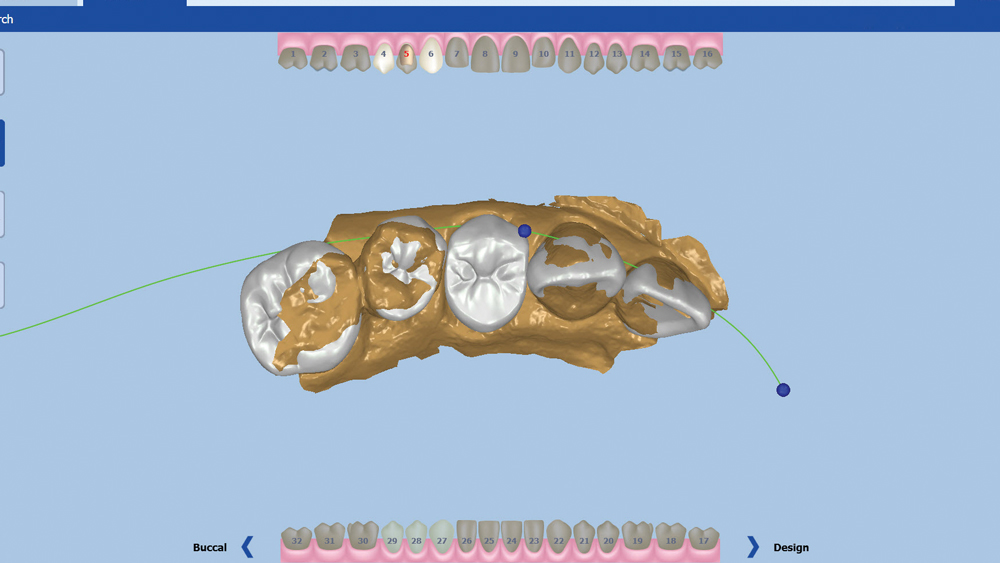
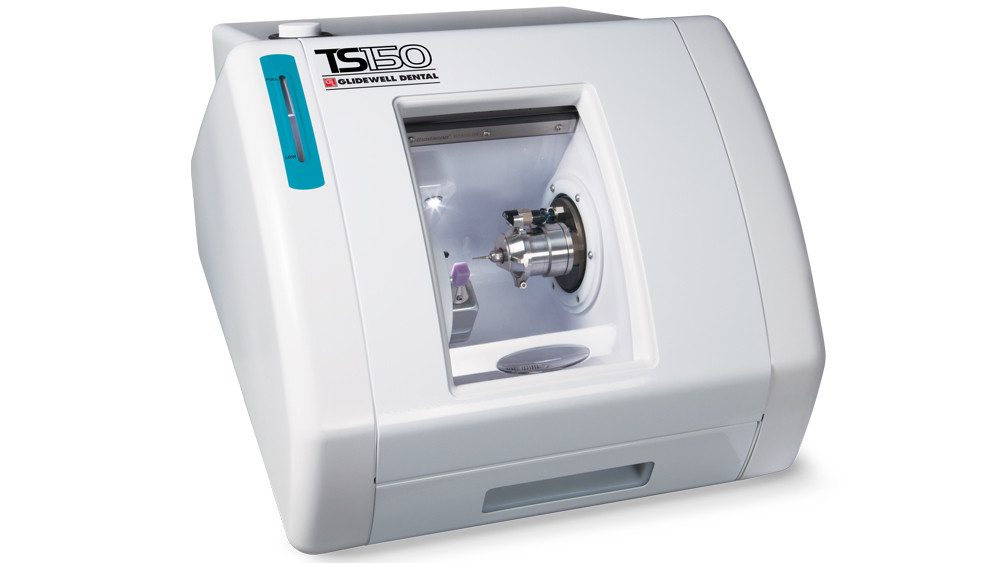
I’ve spoken with many dentists who have implemented intraoral scanners into their practices, and the overwhelming majority have said these devices have made them better dentists. Digital impressions provide instant feedback when a preparation is scanned, and allow users to evaluate their own work, ultimately improving their skills and the quality of care for the patient. When digital impressions are paired with chairside mills, there are several advantages for both the patient and the clinician. As we eliminate the need for a separate appointment for crown seating, we empower patients who have difficulty taking time from work or other obligations. No longer do clinicians have schedule interruptions dealing with lost or failed provisionals. With the opportunity to deliver an accurate final restoration in a single visit, long seating appointments and adjustments can be eliminated. The workflows available today through digital dentistry are better than they’ve ever been, resulting in fewer variables — and making for stress-free dentistry.
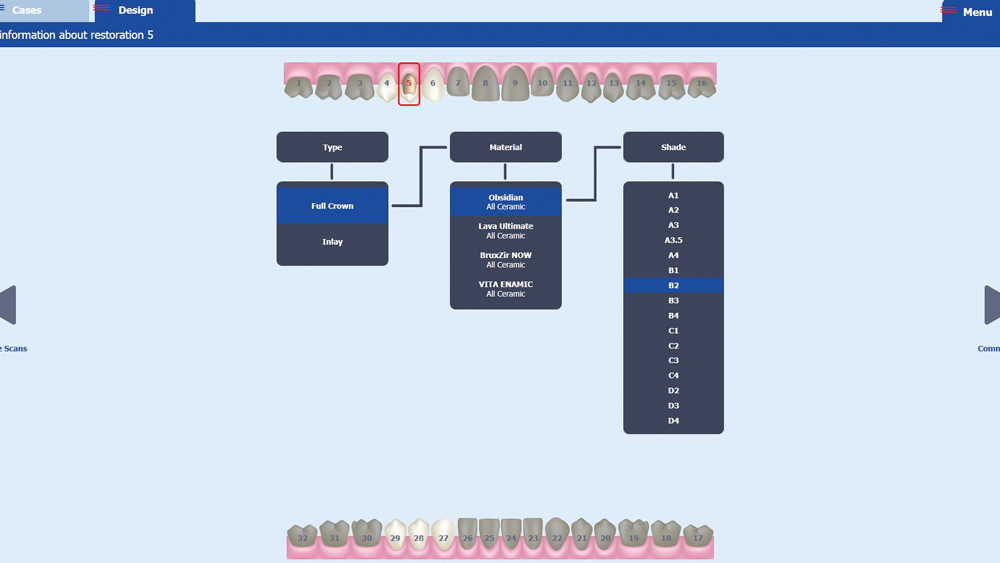
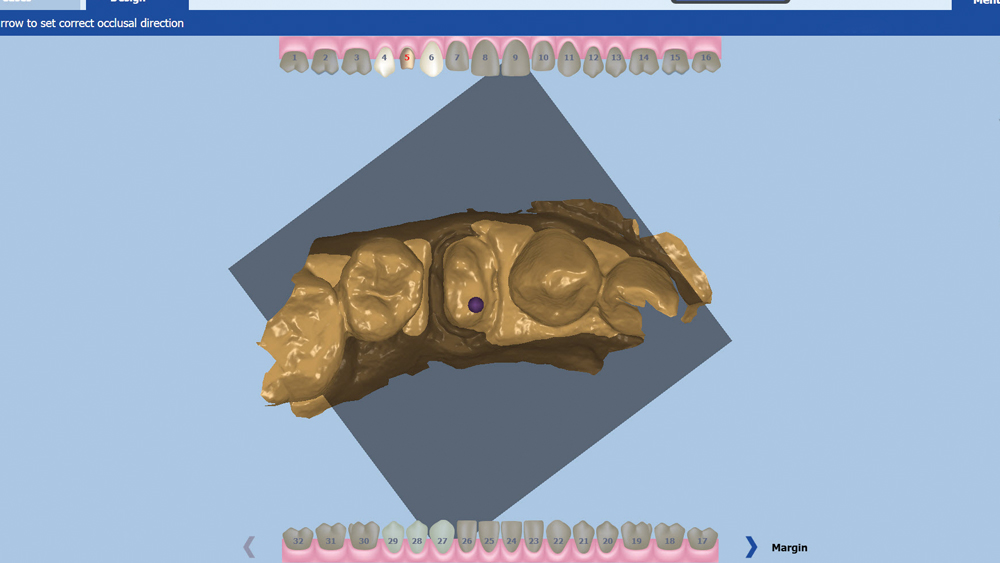
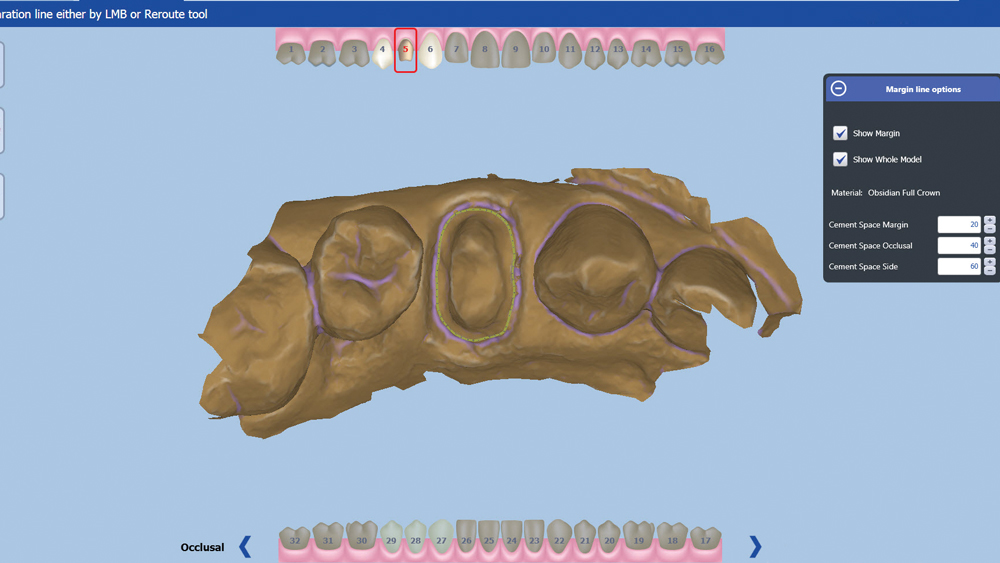
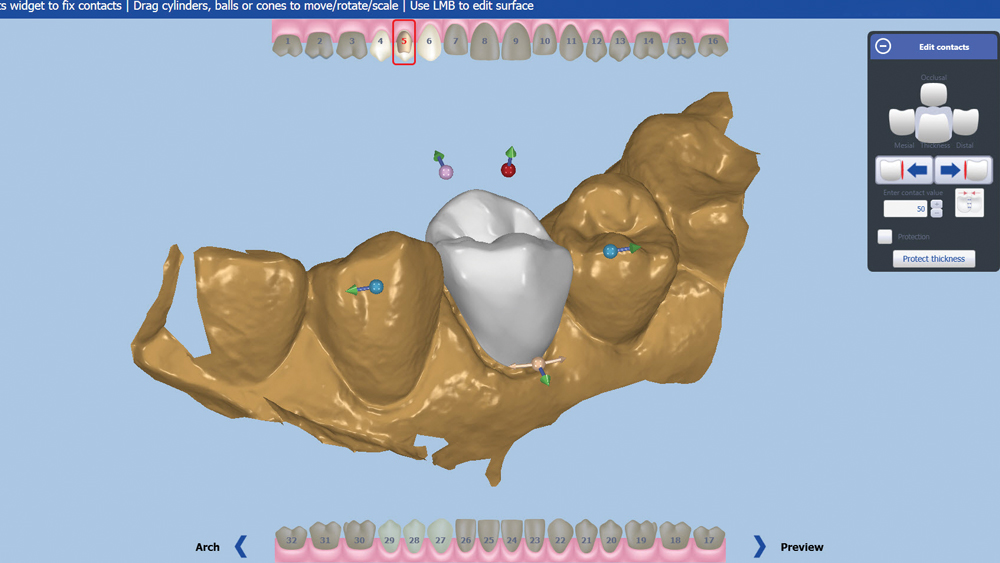
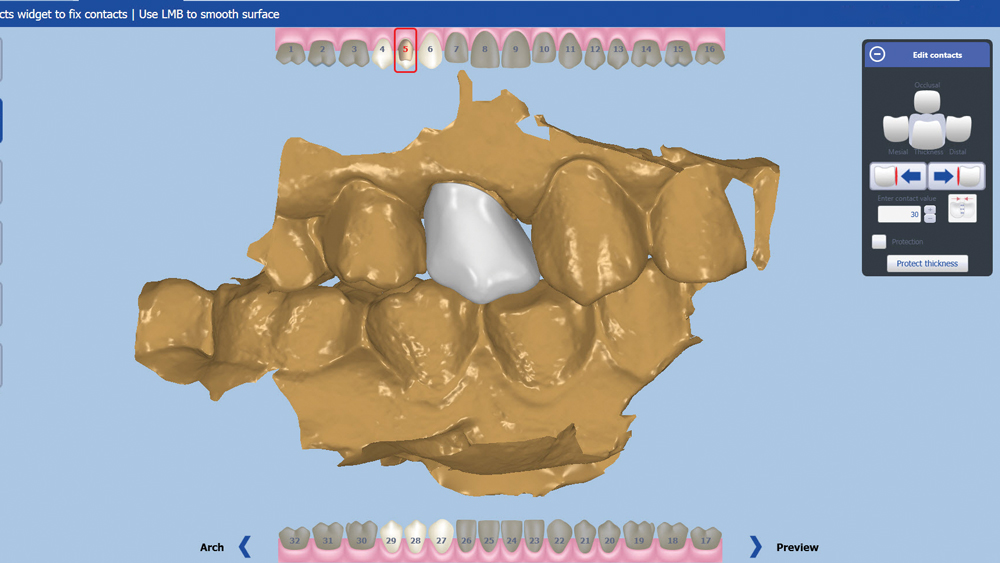
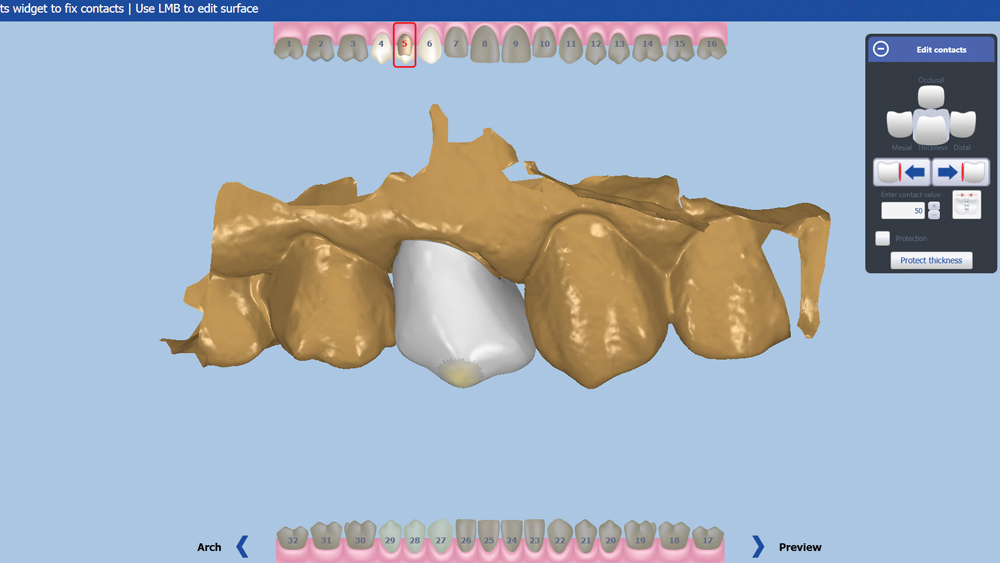
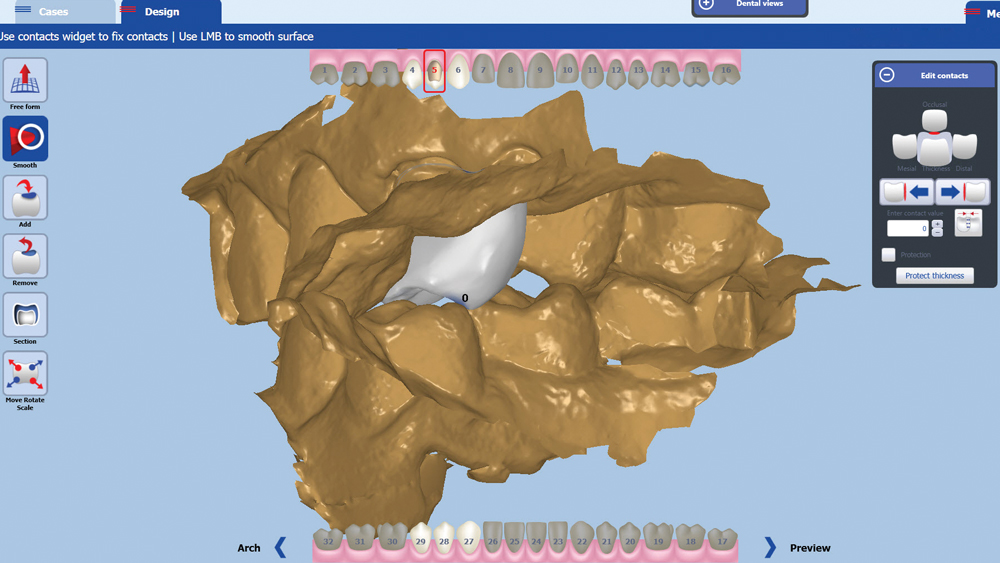
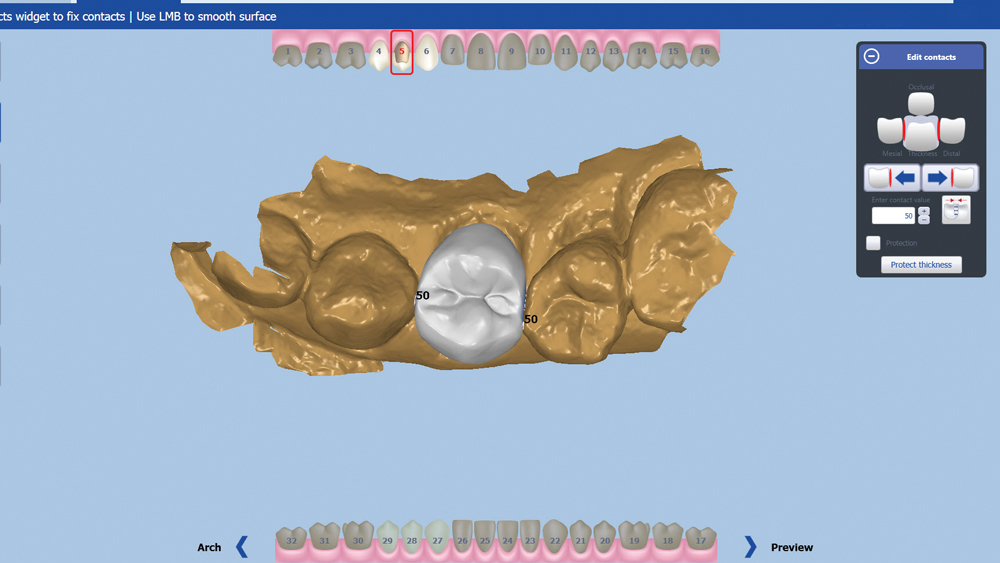
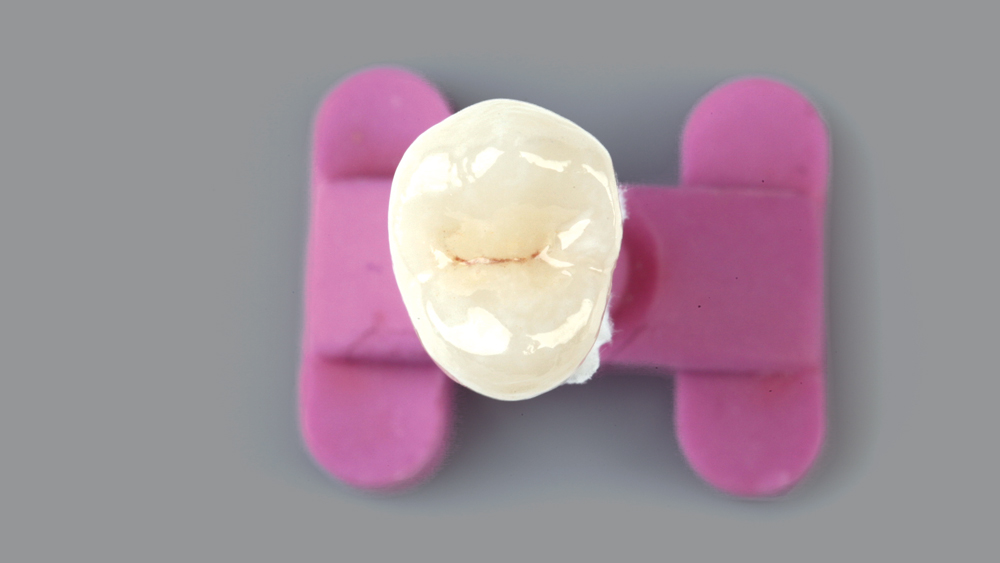
An advantage of CAD/CAM is that each clinician can choose his or her own personal preference when setting up contact values and parameters to enter into the software.
We have the technology and the materials to create excellent crowns, not just in laboratories but in the clinician’s office as well.