Restorative Photo Essay: The IOS FastScan® for an Anterior BruxZir® Bridge
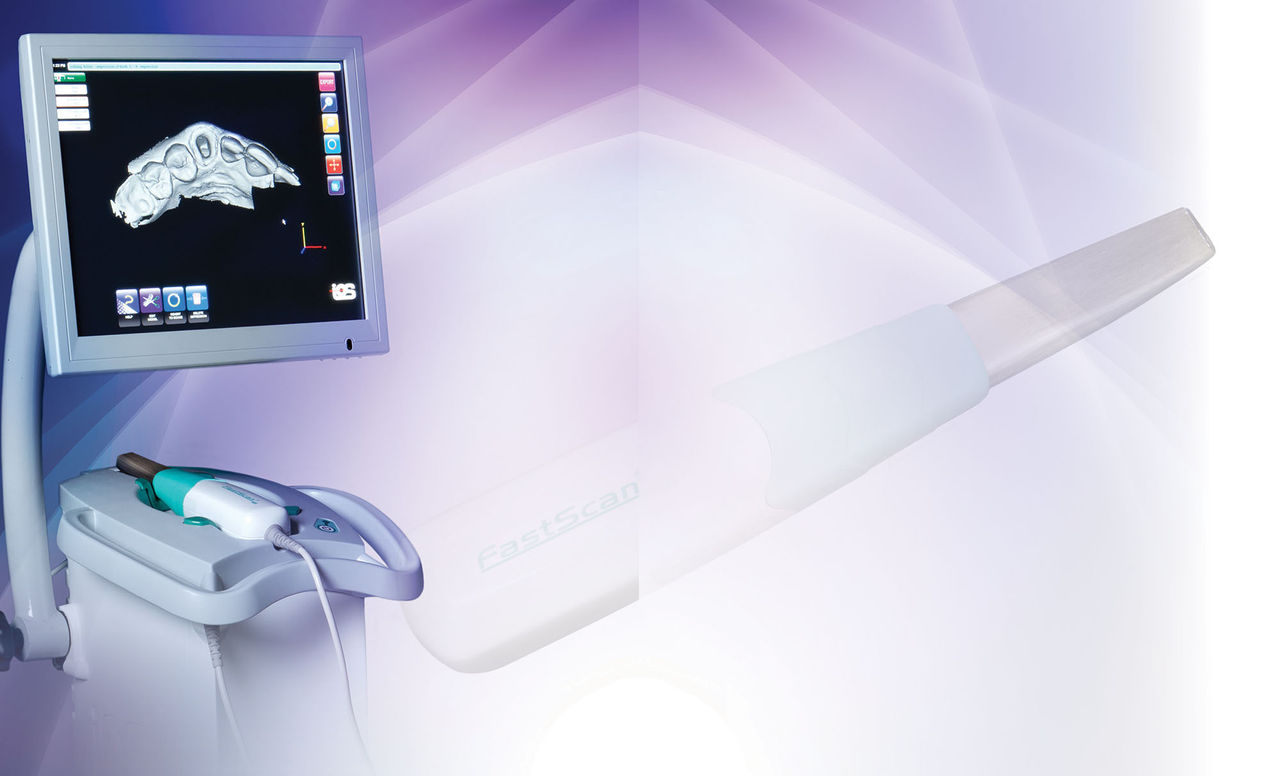
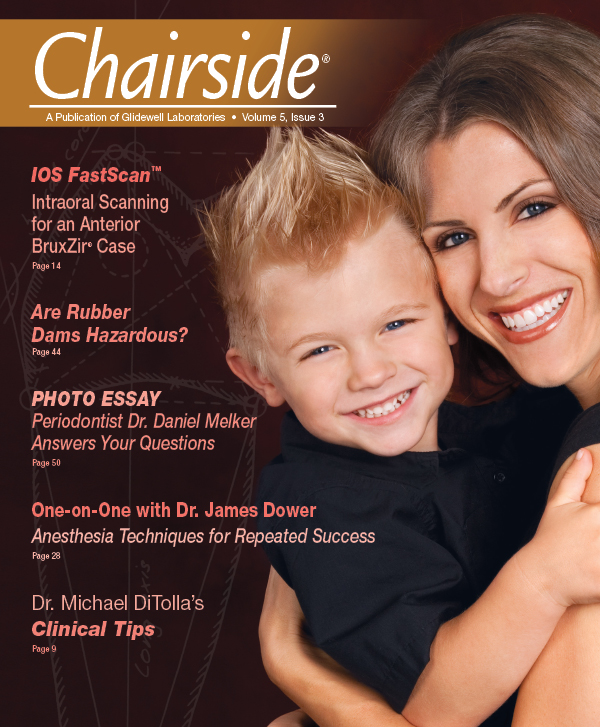
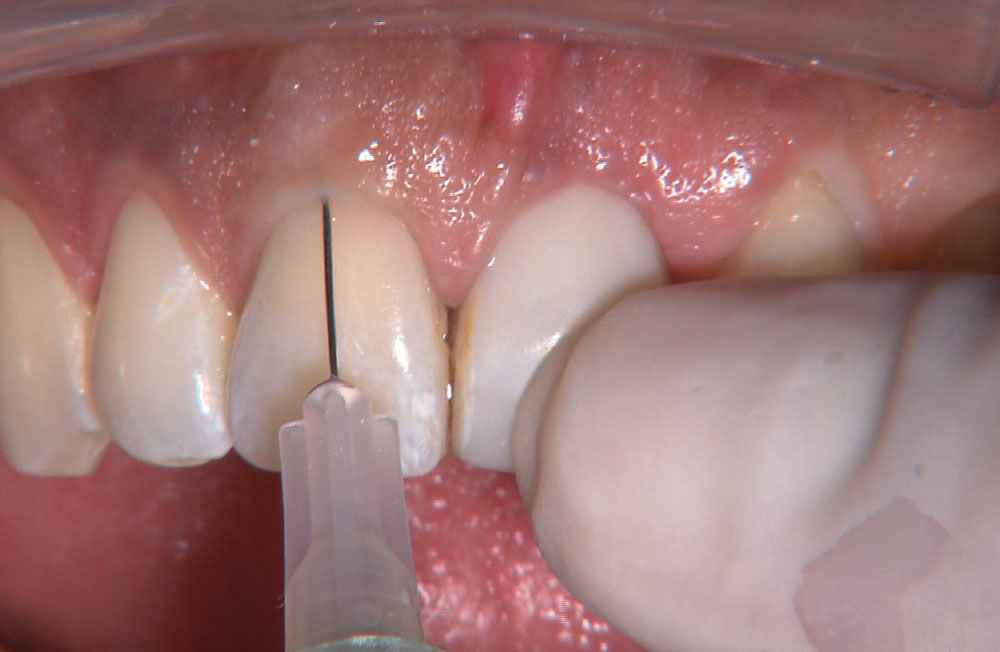
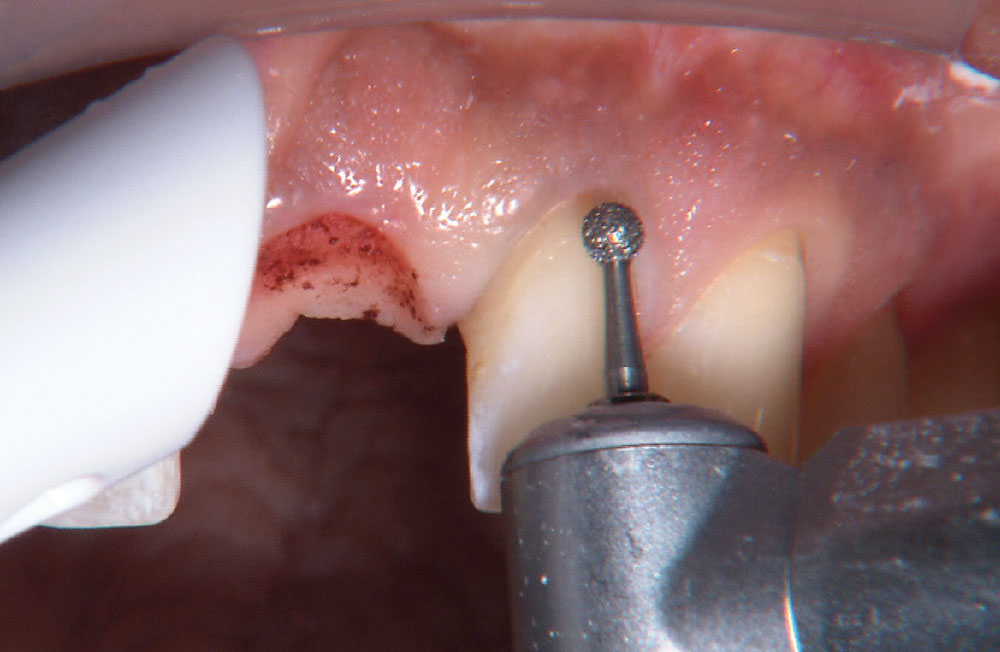
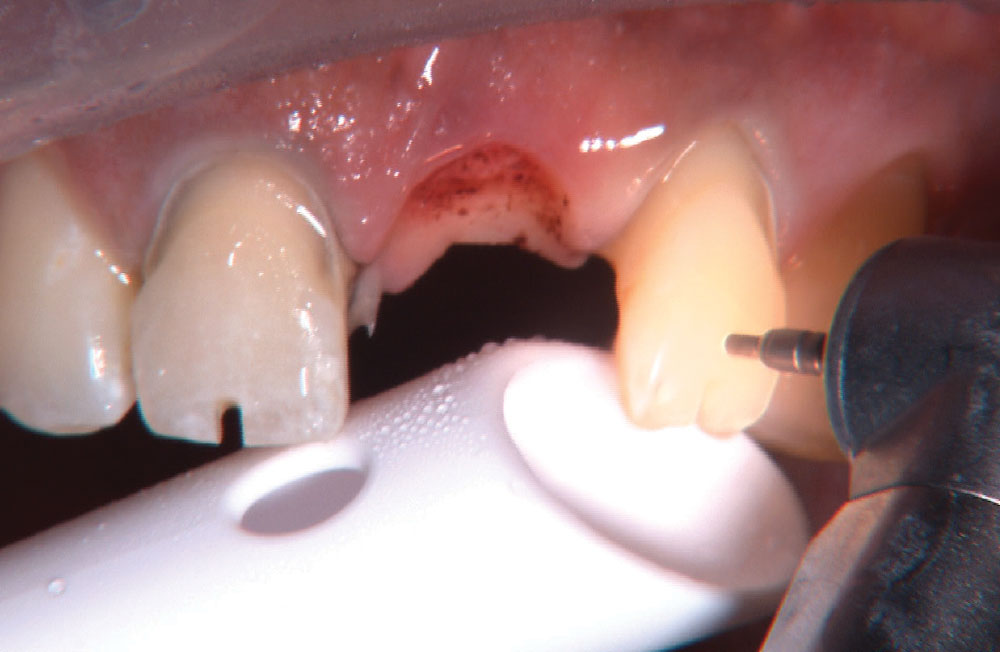
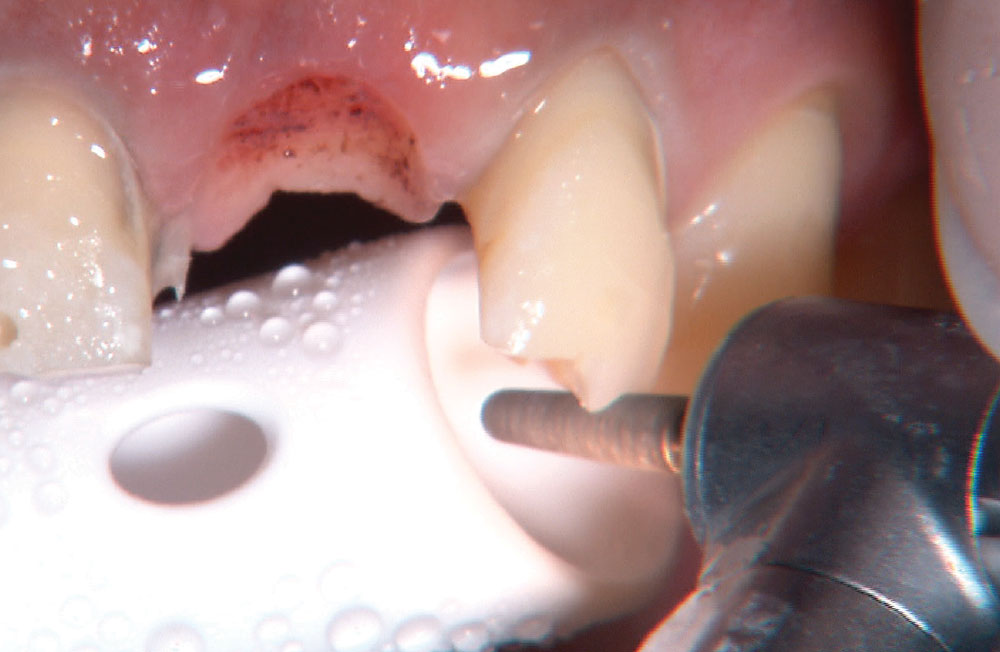
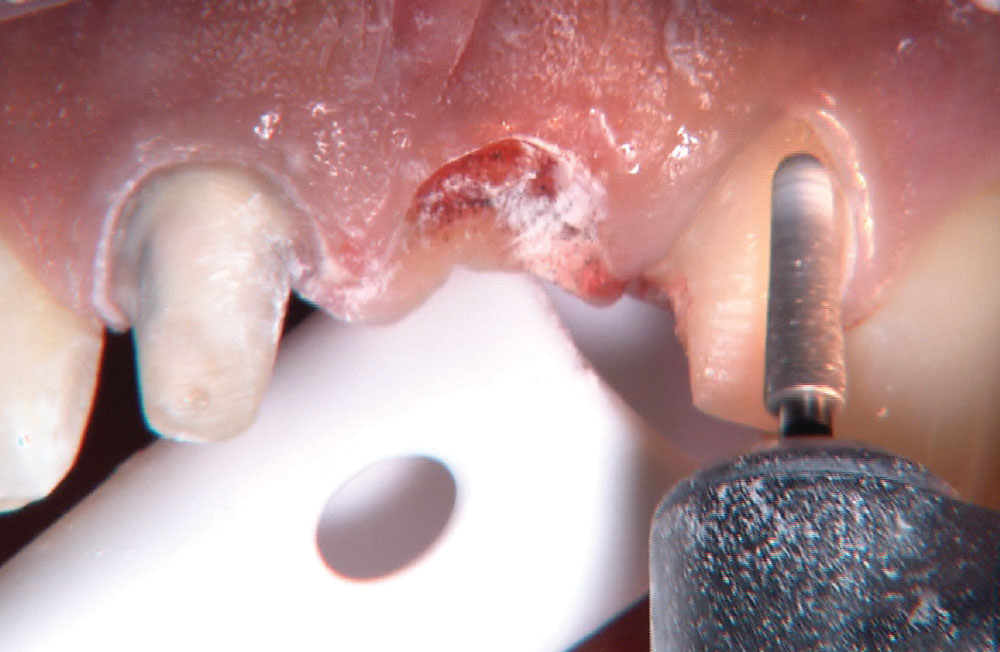
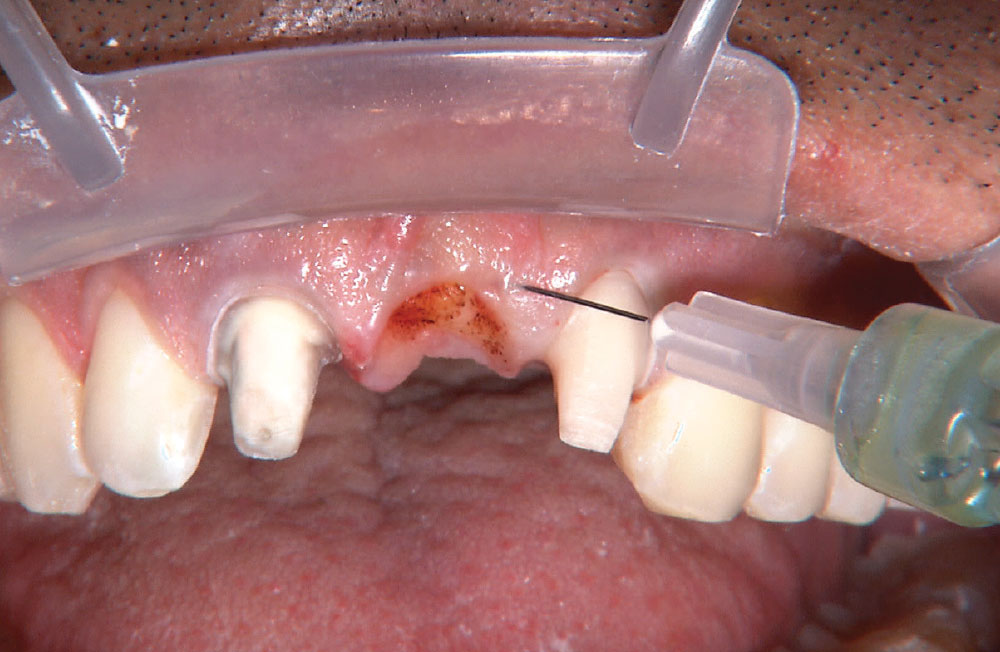
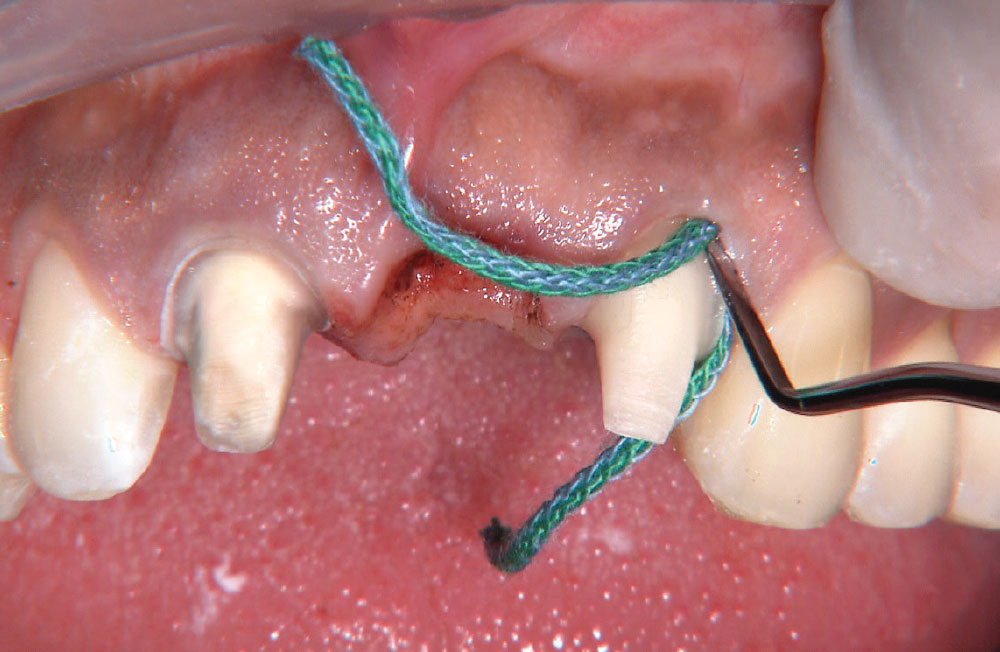
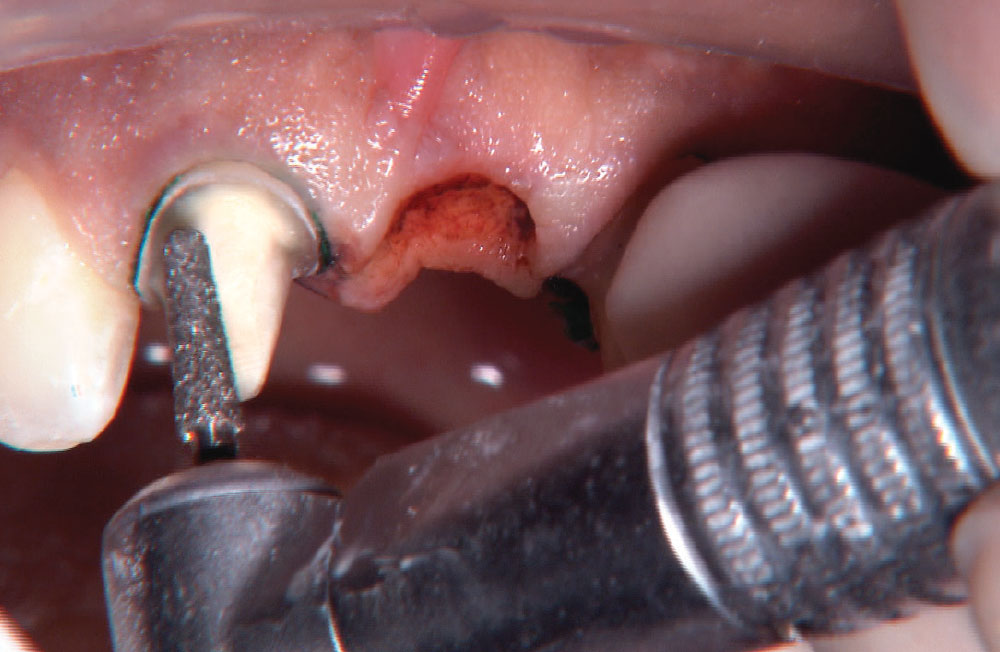
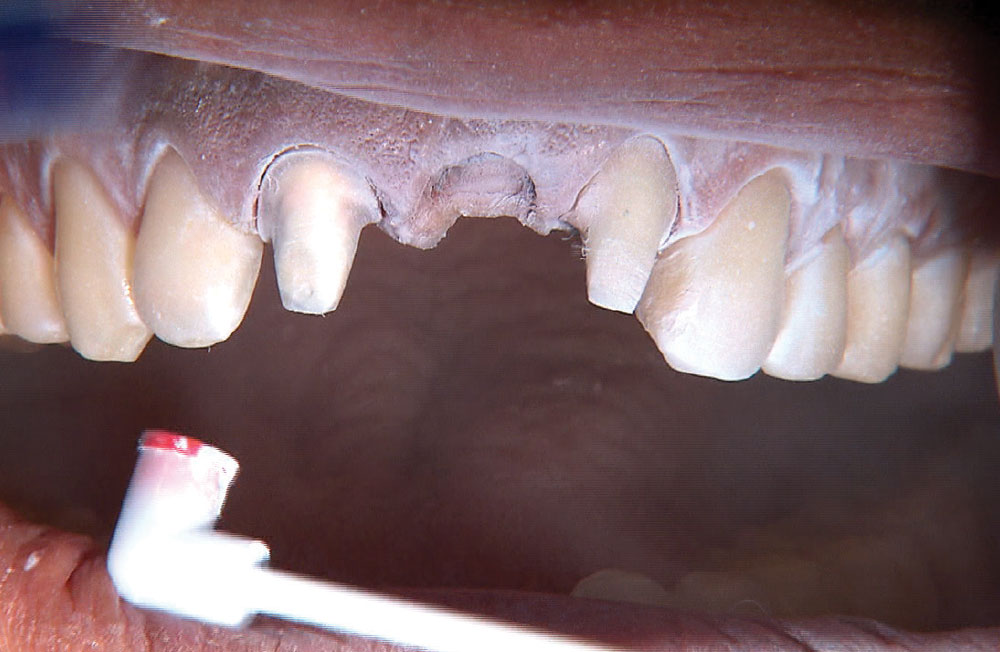
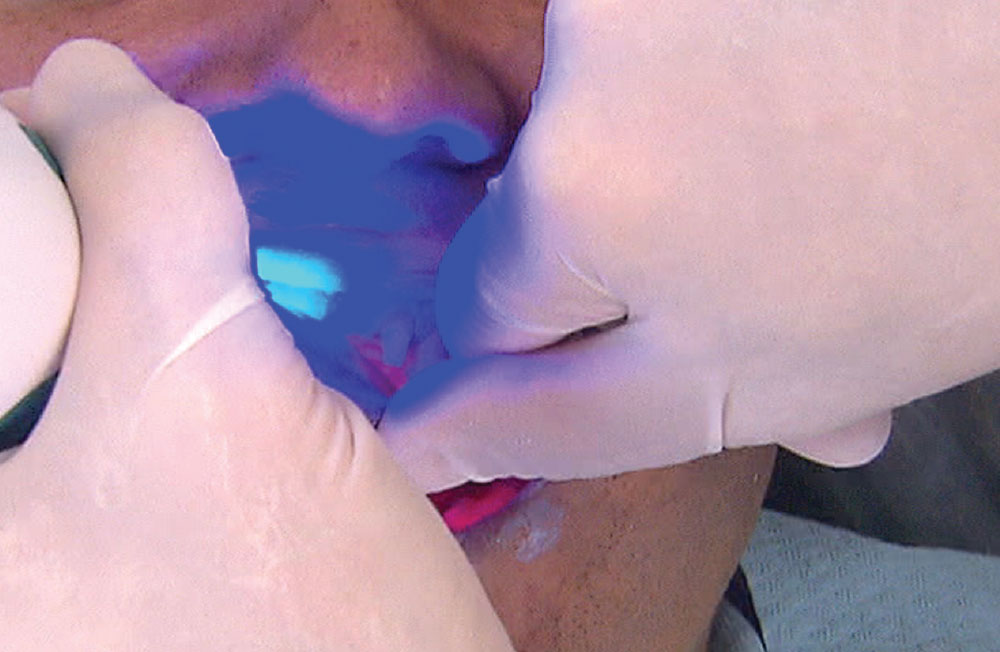
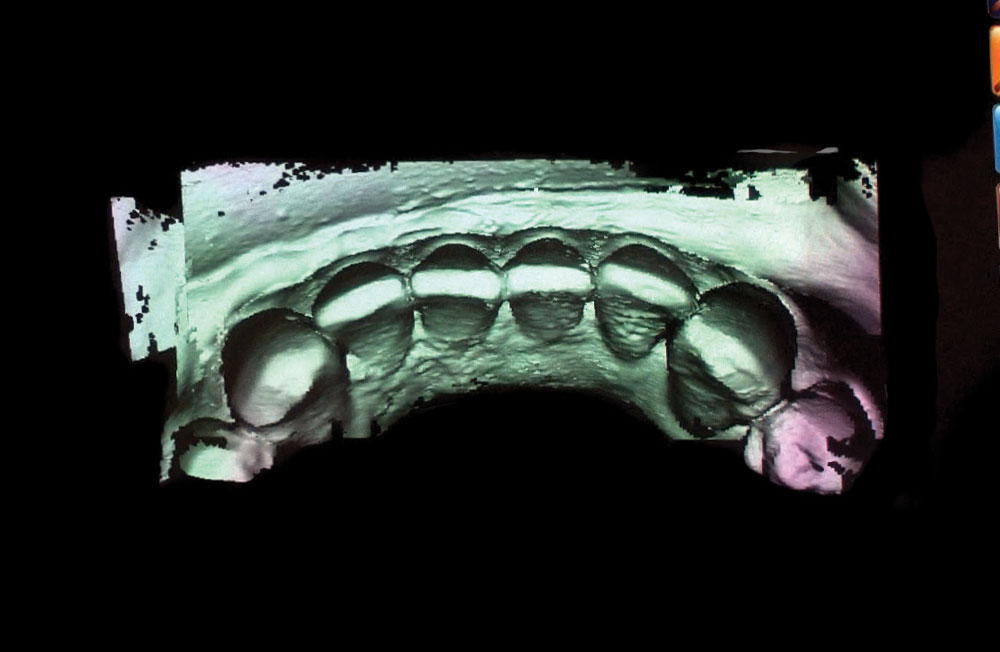
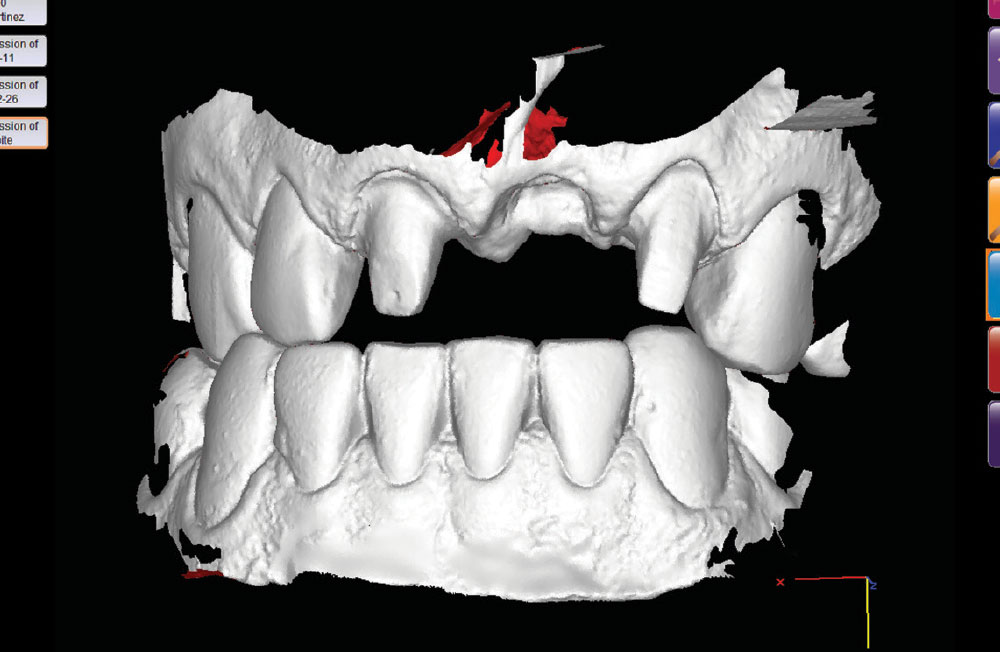
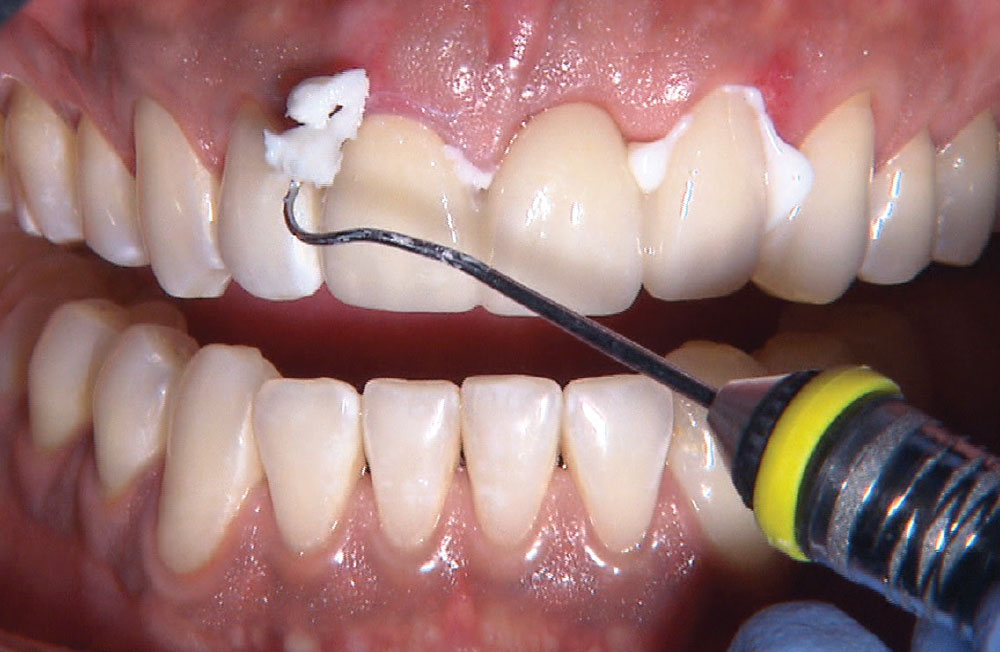
For the photo essay that follows, I wanted to highlight a case that demonstrates some of the techniques I use on a daily basis, while showing a few new techniques derived from our most recent clinical R&D efforts. The case begins with the Rapid Anesthesia Technique and then utilizes the depth-cut based Reverse Preparation Technique. Next, we use a BioTemps® provisional to create an ovate pontic receptor site. After utilizing the Two-Cord Impression Technique, we take a digital impression with the IOS FastScan® from IOS Technologies (San Diego, Calif.). The anterior bridge is then milled without a model using BruxZir®, a solid zirconia material primarily used for posterior teeth. We have received many requests from dentists who have wanted to use BruxZir as an anterior bridge material, so I was looking forward to seeing what type of esthetic result we could achieve on this first attempt.