KP: At Glidewell, we’ve heard time and again that full-arch dental implants are perhaps the most rewarding in dentistry, which is why we’ve been looking forward to having you share your experience with us. Can you tell us how and when you learned to place implants?
WJ: I initially learned how to surgically place dental implants through implant seminars and courses. Since then, I have taken numerous and advanced-level CE courses, including classes offered by the Pikos Institute. I’ve been surgically placing dental implants for seven years and restoring them for over 10 years.
KP: Considering that you were restoring dental implants for a few years before you learned to place them, what inspired you to take the next step and start placing implants yourself?
WJ: I was good at extracting teeth and doing surgical extractions, and I felt comfortable doing flaps. So I had an interest in learning more about implant surgery. I thought it would be pretty cool and beneficial to provide that procedure for my patients.
KP: Did you find patients were more willing to accept treatment when you began offering implant placement in your own general practice?
WJ: There are patients in my practice that would prefer that I perform the surgery because they know and trust me. As a general practitioner, you develop a strong bond and relationship with your patients through recall. Also, since learning to place implants, the barrier to accepting treatment has been lowered because my fees are both fair and affordable, making implants more accessible for my patients, who also have the option of receiving treatment through financing or payment plans. So that has certainly increased case acceptance at my practice.
KP: Do you still refer some cases out to specialists if a more complicated procedure is required?
WJ: Yes, I do refer the more complicated cases to the oral surgeon or the periodontist if I think it’s something beyond my comfort level. That said, I enjoy doing the more challenging cases sometimes as it breaks the monotony of restorative work and allows me to treat more of my patients.
KP: Do you ever use guided surgery? Or does it depend on the anatomy of the individual patient?
WJ: It depends on the situation. For instance, if it’s a congenitally missing lateral incisor in a tight spot for a patient with a high smile line, I’ll use a surgical guide. But if there is an ample amount of bone, I usually feel comfortable placing the implant freehand.
KP: How has placing dental implants affected your practice? What about your patients?
WJ: It has definitely helped me give better options to my patients so they can reach their personal goals. Patients are happy to receive implants, and having different options available to them under one roof makes treatment more feasible and convenient for them. Personally, implant treatment has kept me engaged and brought me professional satisfaction as my skill set evolves and I continue to learn new techniques and procedures. As a general practitioner, I have found that variety is the spice of life.
KP: Going from a single unit or a few units to full-arch dental implants seems like a pretty big leap. When did you do your first full-arch dental implants case?
WJ: After placing quite a few single-unit implants, I took some more advanced courses, and that gave me the confidence to go further and do more challenging cases.
KP: Did you start with implant overdentures and then move on to fixed?
WJ: Yes, I first gained some experience doing implant-retained overdentures, and that gave me the confidence I needed to take it up a notch and do fixed full-arch dental implant cases. It was definitely a good learning curve to follow.
KP: You recently reached out to us here at Glidewell to share a really beautiful case you completed where you provided the patient with a BruxZir® Esthetic Partial-Arch Implant Prosthesis. Many dentists are familiar with the full-arch BruxZir Implant Prosthesis, but this was an 8-unit restoration alongside natural teeth. Can you tell us about that case?
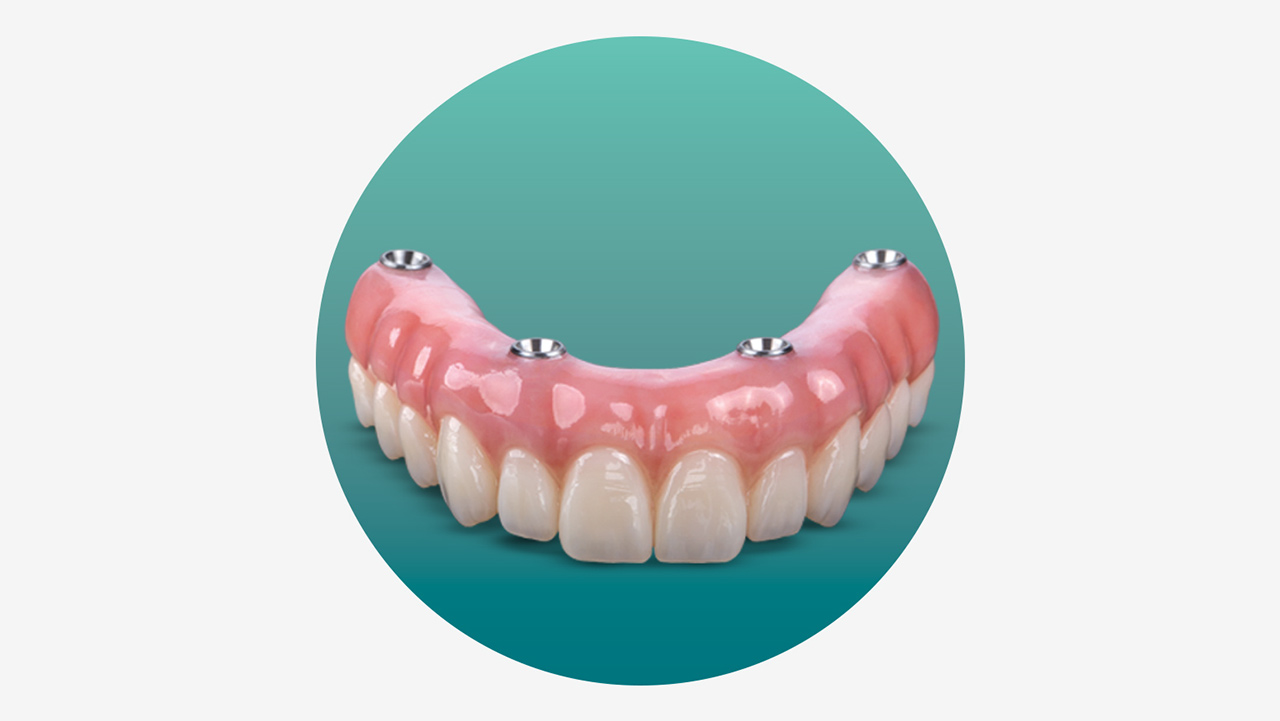
WJ: The patient, who had been partially edentulous for a few decades, came to our practice with a partial appliance and requested a fixed prosthesis. However, she was not interested in removing the remaining five posterior teeth that were still healthy and showed no signs of periodontal disease. A treatment plan was presented to the patient for the placement of four implants to support a fixed restoration. We decided to do a BruxZir partial-arch implant restoration, thereby saving her posterior teeth, which would also help maintain the vertical dimension of occlusion.
Orthodontics was done on her lower arch to level and align the curve of Spee and help intrude the supererupted lower anteriors to create enough interarch space for an FP-3 prosthesis. We performed alveoloplasty and bone reduction on her upper edentulous region, followed by horizontal GBR (guided bone regeneration) using non-resorbable high-density PTFE (polytetrafluoroethylene) membranes. Four months later, we placed four implants. After three months of healing, we provisionalized the implants chairside. I used an existing denture as a template and created the provisional chairside using plastic PEEK abutments. When the implants were ready for restoration, we followed Glidewell’s protocol for the BruxZir Implant Prosthesis.
KP: Did you send in a duplicate of the chairside provisional when you began the restorative process?
WJ: Yes, I took preliminary impressions and sent Glidewell a duplicate. After the setup try-ins, Glidewell provided a digitally milled provisional implant prosthesis for the patient to wear for two to four weeks. I made some slight modifications to the provisional and eventually returned it to the lab. They scanned it to finalize the prosthesis design and then made the final restoration.
KP: And how did the patient like the restoration?
WJ: Oh, she was ecstatic to have natural-looking teeth, because BruxZir Esthetic Zirconia is extremely lifelike. It was gorgeous. She specifically told me she didn’t want the teeth to be too white. She wanted something specific to her age that would match the color of her teeth and her natural gum tissue. The lab did an amazing job, and she was very happy.