One-on-One with Dr. Michael DiTolla: Interview of Dr. Brock Rondeau

I have been looking forward to this interview with Dr. Brock Rondeau for about three months now, since that was about the time I saw my first advertisement for Pure Sleep™ on television. Since then, it seems like I see the Pure Sleep commercial at least two or three times per day. I think it’s pretty clear that they are selling many of these appliances just from the frequency of the commercials. Pure Sleep is a boil and bite snoring device that the patients use without the input of a dentist or the custom fit of a lab-prescribed appliance. If you’ve always wondered about patients’ interest in snoring appliances, let Pure Sleep’s success be your answer. Read on to see how Brock wants you to incorporate snoring and sleep apnea treatment into your practice.
Dr. Michael DiTolla: Brock, it is nice to have you here again today. The last time we spoke, we had the opportunity to talk about two-phase orthodontics. Today, we’re going to talk about snoring and sleep apnea, so as we get started on this, why don’t you tell me a little bit about how you got involved with snoring and sleep apnea?
Dr. Brock Rondeau: Well, Mike, years ago I would take some small courses on snoring and unfortunately with the courses I took, dentists were just learning to make snoring appliances. The courses were mostly from dentists who actually invented those snoring appliances and named them after themselves. So I would take a course from one dentist and learn about his appliance, and I would take a course from another dentist and learn about his appliance, and then I would try the various appliances. I have also used the Silent Nite® appliance, which is one of the most popular appliances made by Glidewell. I like it very much as it’s a very simple appliance and very comfortable for the patients.
MD: So, in the beginning, it wasn’t really a unified field per se, and a dentist would come up with an appliance and the only way to tell a dentist about it was to teach your course. So it was not like you could go take a comprehensive class; every class that you took was centered around one appliance?
BR: Yes. When I joined the American Academy of Dental Sleep Medicine, they also talked about sleep apnea and snoring synonymously, and how sleep apnea is a medical disorder. And since we really need to treat the snoring as well as the apnea, a medical doctor, and not a dentist, must make the diagnosis. The oral appliance is the No. 1 treatment, the key to treating all mild and moderate cases.
Today, we do sleep studies in our office that determine whether or not the patient has mild, moderate or severe problems. If the patient has a mild or moderate problem, we make the oral appliance and confirm the results with another sleep study to make sure the oral appliance has stopped the snoring as well as the sleep apnea. So now we’re treating the whole patient, and I think if the profession embraces this philosophy, then oral appliances would be better accepted by the medical community.
There are really only three ways to treat sleep apnea: CPAP, oral appliances and surgery. CPAP — which is that device that goes over the nose with an air compressor that blows air up your nose all night — works very well for obese patients; they swear by it, their life improves so dramatically that they can’t live without it. It does prolong their life and I heartily recommend CPAP for any severe case. On the other hand, if a patient is just snoring and doesn’t have sleep apnea, or if the patient can’t wear the CPAP device, or for the mild to moderate cases, the oral appliance is the No. 1 option. The thing that turned it around for me is when I read in the January 2006 issue of the medical journal Sleep, from the American Academy of Sleep Medicine, in which they stated that for mild to moderate obstructive sleep apnea, the oral appliance is the first treatment option.
MD: That must have been a big change for them. We might like to think that medicine doesn’t have any politics in it or doesn’t have any factions, but you can imagine medical doctors and their associations looking for medical cures for this medical condition. Was it somewhat controversial when they came out with a dental recommendation for this medical condition?
BR: That’s right. It was actually Dr. Rob Vies who first enlightened me several years ago when he stressed the fact that if you treat snoring, you must also treat sleep apnea. I think it was a bit controversial and I think a lot of sleep specialists still don’t go along with it because I’m getting more patients coming to me that can’t wear their CPAP device. And that’s probably the No. 1 way patients find me. I have a radio ad and I put the word out that if you’ve been diagnosed with sleep apnea or you snore, and you’ve been given a CPAP device and you cannot wear it, then give me a call and we’ll see whether or not an oral appliance is the answer for you. So, we get at least three new patients a week coming in seeking alternative treatment.
MD: If 100 average people are given a CPAP, what percent would you say do fine with it, what percent are so-so, and what percent are unable to wear the CPAP?
Daytime sleepiness is the No. 1 symptom of obstructive sleep apnea; this constant daytime sleepiness, waking up unrefreshed and being tired all the time makes the patient susceptible to falling asleep when driving. Many car accidents — even the Exxon Valdez accident and the Chernobyl accident — were due to excessive daytime sleepiness because of sleep apnea.
BR: I think you have to break it down to mild, moderate, severe. And I think that’s where I’m having the problem, when they give the CPAP machine to the mild and moderate patients. Those patients really don’t take to it too well. First of all, their problem is not so serious that they are having severe daytime sleepiness and symptoms, and they find it cumbersome. So I think if you look at the severe cases, they are really in bad shape, really overweight and so tired that they can’t function normally. Daytime sleepiness is the No. 1 symptom of obstructive sleep apnea; this constant daytime sleepiness, waking up unrefreshed and being tired all the time makes the patient susceptible to falling asleep when driving. Many car accidents — even the Exxon Valdez accident and the Chernobyl accident — were due to excessive daytime sleepiness because of sleep apnea. Frequently, you pick up the paper and there are reports that some highway truck driver has fallen asleep and caused an accident. It’s a very serious problem. In fact, they’re saying obstructive sleep apnea causes more accidents than alcohol-related incidents. It’s a big deal. So the patients with severe sleep apnea adapt very well to the CPAP.
MD: Because it’s kind of like a matter of life and death for them almost, literally, to wear this unit.
BR: Yes, and to be honest, the oral appliance is not as effective at preventing obstructive sleep apnea if the truck driver has an extremely large neck, is grossly overweight, or has a severely retrognathic lower jaw. The oral appliance is not as effective in the severe sleep apnea cases, so I really think we have to work with the medical profession and say, “Look, you take the severe ones, give us the ones that are mild to moderate or just snoring, and let us treat those.” But I’m finding that even some patients who go to the hospital for a sleep test, if they come out and they’re snoring, the doctors don’t even treat them. They just tell these patients that they have to lose weight. They are ideal candidates for oral appliances and dentists should identify these patients in their practice who need and want oral appliance therapy. Failure to treat patients who snore is also unacceptable to spouses who do not enjoy being kept awake all night with loud snoring as well as apneic events.
MD: The CPAP machine is undoubtedly the most effective way to treat sleep apnea, but it also has the highest amount of side effects and objections?
The thing that turned it around for me is when I read in the January 2006 issue of the medical journal Sleep, from the American Academy of Sleep Medicine, in which they stated that for mild to moderate obstructive sleep apnea, the oral appliance is the first treatment option.
BR: Yes, and to finally answer your question, for the mild to moderate cases who are given CPAP, I’m finding a tremendous failure rate — I’m thinking that it could be as high as 70%, and that’s where I’m getting a lot of patients. Now, the other interesting thing is that Medicare has just been looking into this and they’re going to start paying for the treatment of patients with obstructive sleep apnea. Medicare wants to prove compliance because they don’t want to pay anybody to have these machines sit in their closet, they want the patient to wear them. So there’s actually a new CPAP device where you attach it to a dedicated telephone line just like a fax machine, and they’ll read directly from that CPAP device and it’ll tell you exactly how many hours per night the patient has been wearing it or if they haven’t been wearing it at all. If the patient is not wearing the machine, then the CPAP company is not going to get paid from Medicare.
I think this is an ideal opportunity for the dental profession to get involved and help these patients. It is important for dentists who are interested in oral appliance therapy to approach the medical profession and especially the pulmonologists in the sleep centers and hospitals, to refer the patients who cannot tolerate their CPAP devices to dentists who are knowledgeable in fabricating oral appliances. I have done that in my city and now have medical doctors and sleep specialists referring me patients. The system is not presently working for patients with sleep apnea. Once the diagnosis is made, the patients are referred to a company that sells them the CPAP device. If they cannot tolerate this device, then no further treatment is offered to the majority of these patients. Most patients who come to my office state that neither their medical doctor, the sleep specialist, nor the company that sells the CPAP machine ever mentioned to them that oral appliance therapy is a viable alternative to their treatment. I think there is something wrong with the system because I believe these patients’ treatment should be more closely monitored. By not treating these patients they are subject to cardiovascular complications, type 2 diabetes and GERD (gastroesophageal reflux disease).
MD: I sleep on my stomach, for example, so I don’t think I could ever wear a CPAP unit. Sometimes, I even have a hard time falling asleep with my night guard in my mouth, let alone putting something like a CPAP on. There has to be some realization that CPAP is a great way to go, but there are a large percentage of people who can’t wear it. So your radio advertisements, what do they actually say?
BR: It’s a 30-second ad that says, “If you snore, or if you have sleep apnea and you can’t wear your CPAP device overnight, give me a call because oral appliances are often very effective at treating that condition.” It gives my phone number and the phone starts ringing. It’s interesting when the husbands come in and I ask them who referred them. Often they say that their wives forced them to come in. And then it’s really interesting when you send them for a sleep study, and they come back and you go over the sleep study and you say, “Well, you realize you’ve got a pretty severe condition here.” I ask them for their family history of heart attack, strokes or diabetes, and frequently they’ll say that their father had diabetes, heart disease or a heart attack. I tell them that’s the road they’re heading down unless we do something to intercede.
The cardiologists are starting to get on board now and they’re writing articles about the relationships between sleep apnea, heart attacks, stroke and cardiac arrhythmias. And the thing I found interesting at the sleep meeting was that many professionals believed that plaque builds up in the arteries mainly due to cholesterol and saturated fats in the diet. Well, it turns out that it’s the lack of oxygen that stimulates the saturated fats to go into the vessels. So, really, the cause of a lot of these problems is not just the diet but it’s the sleep apnea and lack of oxygen, and having all these apneic events during the night. When you understand that, you can see why perhaps Medicare is getting involved with sleep apnea: it’s a lot cheaper treating the sleep apnea rather than treating people for heart attacks and strokes.
MD: Let’s say somebody hears your advertisement, a patient who has tried to wear a CPAP and just could not do it. Walk me through how you are going to treat that patient.
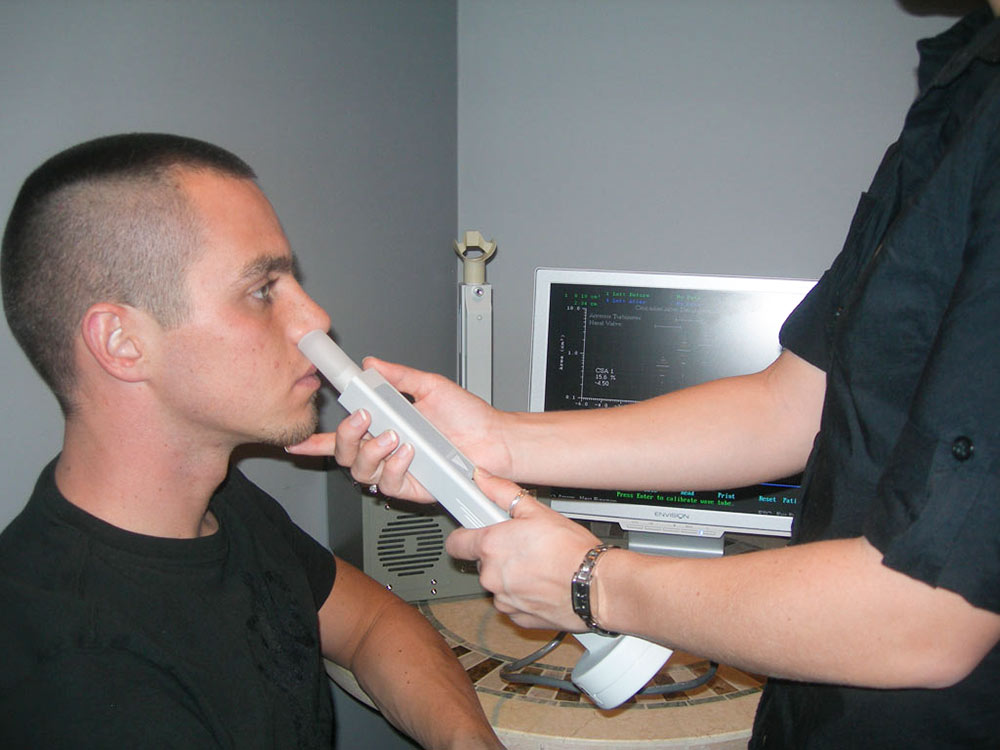
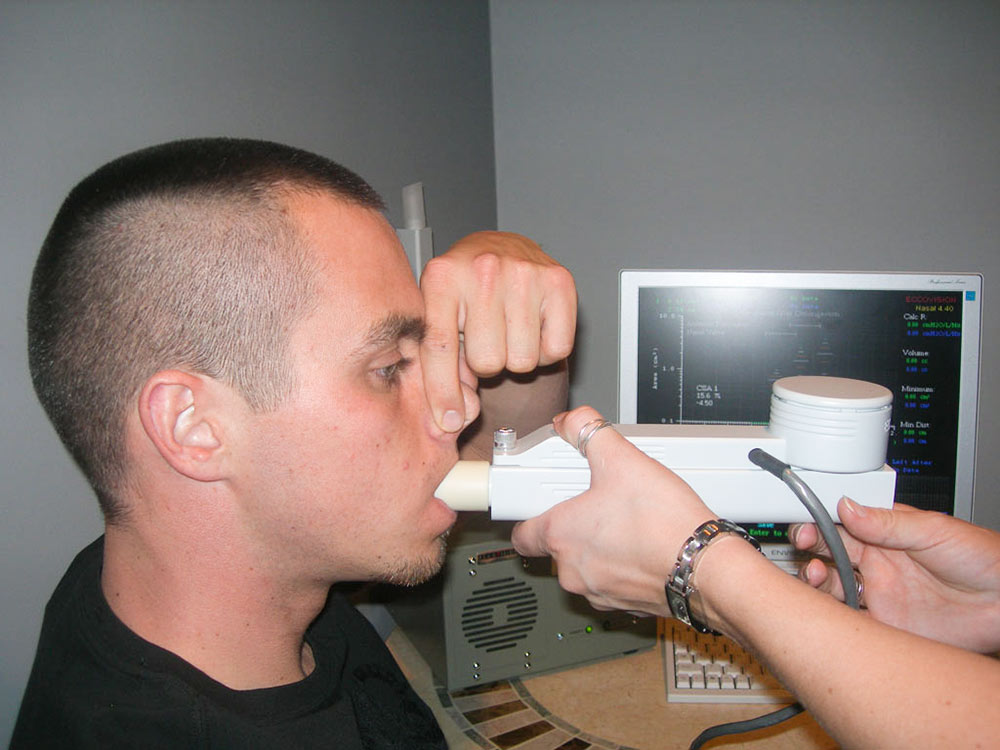
BR: Well, I think the key to every success is diagnosis, and I have a couple of devices in my office, which are unique to a sleep practice. One device is called a rhinometer, which evaluates any obstruction in the nose, and so we just put it up to one nostril and the patient doesn’t breathe and the sound waves go up the nose and any obstructions are recorded on the computer screen. I had a patient the other day who broke his nose and of course he’s got a blockage, but it’s not too far back in the turbinate area so it should be relatively easy to rectify the problem. The rhinometer tells us that if there’s any blockage due to enlarged turbinates, deviated septum, polyps or any allergies which cause swollen nasal mucosa. Now, the key is that if there is any blockage in the nose and if you see the patient mouth-breathing, then I think you should send the patient to an ENT specialist. Once the nasal airway is clear, then you’ve got a much better chance of the oral appliance working.
The second device is called the pharyngometer. We have the patient blow all the air out of their lungs, and then we measure to determine the size of the airway. We get a measurement, and then we put some wax between the back teeth and move the jaw to a position similar to a construction bite. For example, we might open the vertical in the anterior 5 mm and move the jaw forward 4 mm. We use the pharyngometer again to see if the airway measurement increases; sometimes, it is a 50% or 100% increase. When the airway significantly increases when the mandible is held forward, we are confident that the oral appliance will be effective. The oral appliance effectively protects the airway at night, even when the patient is lying on their back, by moving the mandible and the tongue forward.
MD: I think the idea of sending patients out for sleep studies seems confusing to dentists. You mentioned that you often have the patients do them at home with a take-home unit provided by your office?
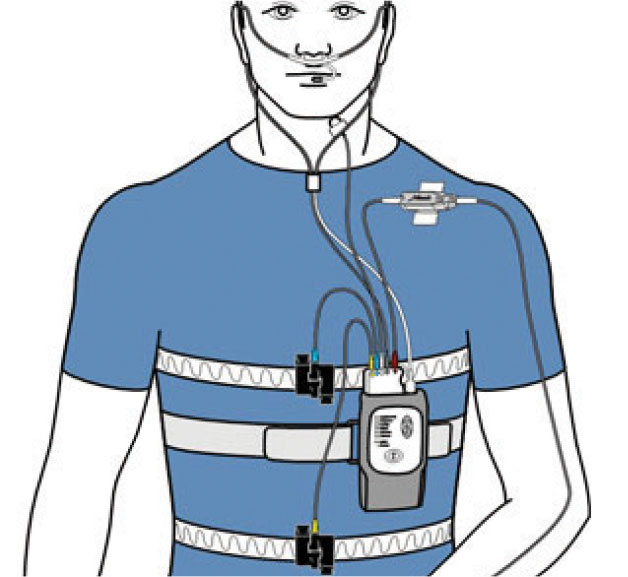
BR: That’s right. I’m using a device called Embletta® (Natus Medical Incorporated; Pleasanton, Calif.) now which is more recognized by the medical profession because it has a nasal cannula. The device I was using before wasn’t as recognized by the medical profession so I’m sticking to devices that the physicians recommend. I just met someone today who told me that many sleep specialists have adapted these overnight sleep studies — home sleep studies — in their sleep centers because some patients come in and they say, “I don’t want to sleep in a strange bed all night, I don’t want all of those things hooked up to me, I can’t do it, I’m claustrophobic,” so they give them the home sleep study. In Europe, most of the studies are home sleep studies because the Europeans have figured out that it’s a lot less expensive to do the home studies than it is to do the hospital studies. Here in Canada, like in Vancouver, B.C., it’s a year and a half to get a sleep study, and in Nova Scotia, it’s a six-month wait. In the U.S., you’ve got a better system, but still, if everybody that needed it went in for a hospital sleep study, you couldn’t possibly handle the volume. I talked to a pulmonologist in Reno, Nevada, and he told me he thinks that obstructive sleep apnea affects 15%–30% of the adult population, even though the published number in the literature is much lower. That is a large number of patients who need treatment, which means this is an excellent opportunity for dentists to get involved to help these patients.
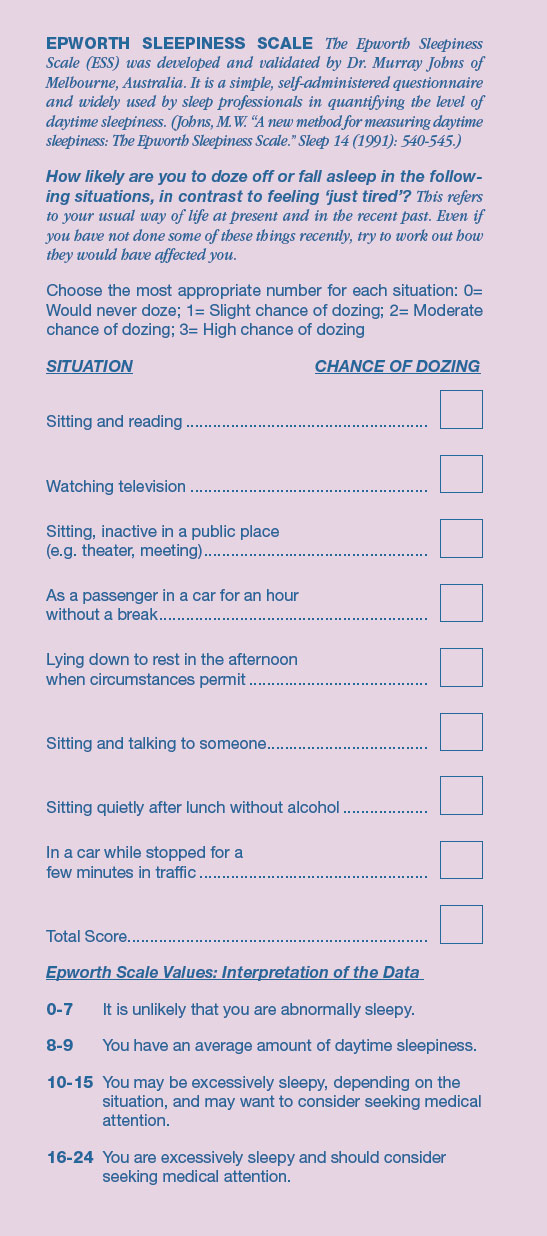
… he gave the Epworth Sleepiness Scale to all the patients who said they snored that came into his office during the next three weeks. Now he’s got a big practice — but in three weeks he’s got 50 people lined up for snoring appliances!
MD: For general dentists who aren’t currently making these appliances in their office and want to get started, what’s the best way to identify which of their patients might make a good candidate for these appliances?
BR: You need the Epworth Sleepiness Scale, because it basically asks patients how likely they are to fall asleep during routine situations. A zero means you would never doze off, one means a slight chance of dozing, two is a moderate chance of dozing, three is a high chance of dozing. You will be amazed at the amount of daytime sleepiness in your patient population. I had a dentist take my sleep course in Toronto and he went back to his office and he gave the Epworth Sleepiness Scale to all the patients who said they snored that came into his office during the next three weeks. Now he’s got a big practice — in three weeks, he’s got 50 people lined up for snoring appliances! This includes the hygienists giving the test to anyone who knows or has been told that they snore. So if dentists don’t know whether it’s going to be worth doing in their practice, they need to have some patients take the Epworth test and I think they might be surprised.
MD: Is that doctor now going to do home sleep studies on all those patients?
BR: Yes. He bought the Embletta, and he’s going to do the home sleep studies on those patients. I recommend that the home sleep study device, the Embletta, be used as a screening device to determine the seriousness of the problem. If the patient is severe, they should go to the hospital for an overnight sleep study which is known as a polysomnogram. The diagnosis must be made by a sleep specialist. If the diagnosis is mild to moderate sleep apnea, then the dentist can proceed with the oral appliance therapy. It is important to mention that following oral appliance therapy, patients must either repeat the home sleep study or go to the sleep center for a polysomnogram to confirm that the oral appliance effectively treated the sleep apnea. The Embletta home test is very good — obviously, if the medical doctors are buying it and using it in their sleep centers. It’s also the one that is reputed to be the No. 1 home sleep study used in Europe for the past eight years. It’s been well-researched and it corresponds very accurately with the polysomnogram at the hospital.
Now, if a dentist wants to get into this and doesn’t want to buy any equipment and says, “Look, I don’t want a rhinometer, I don’t want a pharyngometer, I don’t want to buy an Embletta, I don’t want to spend a nickel,” he can just hand out the Epworth sleepiness scale to his patients. He can just contact a sleep center and tell them, “I want to send you some patients.” Now, what sleep center would not want a dentist to send them some patients? So all the patients who score higher than a 7 on the Epworth scale are sent to the sleep center. If they are diagnosed with severe sleep apnea, then the patient stays with the sleep center and gets a CPAP. I urge the dentists to have an agreement with the pulmonologist or sleep specialist. “If the patient I sent you is mild to moderate, send them back to me for an oral appliance, and then I’ll send the patient back to you to see if the oral appliance is effective in reducing the sleep apnea.” The sleep specialist is getting numerous patients referred for sleep studies so naturally he’ll want to deal with the dentist, and then gradually the dentist builds up a good rapport with the sleep specialist. The objective is to get the sleep specialists sending you patients who won’t wear CPAP. The patient must receive the most ideal treatment, CPAP for severe sleep apnea and oral appliances for the mild to moderate sleep apnea. The good news for the dental profession is that the majority of patients who snore have mild to moderate cases, and are therefore ideal candidates for oral appliance therapy. The medical and dental profession must work together in the best interests of the patients.
MD: What would you say to our dentists about the profitability of treating sleep patients? Can it be a profitability center in the typical general dental practice? Are you comfortable talking about how much you would normally charge for the appliances themselves?
BR: Well, I think it’s very profitable because the records are all done by the staff. They explain the home sleep study and show the patient how to put the device on at night and how to record it, and when they come back the staff puts the Embletta chip into the computer and prints the report out for me. My staff does the initial consult and spends half to three quarters of an hour with each new sleep patient to educate them about what’s going on. Then they do the rhinometer test, the pharyngometer test, and give them the Epworth Sleepiness Scale and a few other forms that we have them fill out. I review all of this and go in to discuss the problem with the patient. I charge a total of $3,000; some dentists charge less but I include two or three home sleep studies for each patient with that fee. Thankfully, with the Embletta, the disposables only cost me seven dollars. The last system I used, the cost of each home sleep study was $85 and it wasn’t as good as the Embletta. I’m doing two sleep studies, sometimes three, and I’ve got the pharyngometer, rhinometer, I’m testing their nose, testing their airway. I put the appliance in, I test the airway again to make sure it opened up. To be honest, most of the members of the American Academy of Dental Sleep Medicine don’t have a pharyngometer, or rhinometer, or a home sleep study device. They send all their patients for hospital sleep studies (polysomnograms) before and after oral appliance therapy. Personally, I find these three diagnostic devices extremely useful in any sleep practice to improve my success rate.
MD: If they are interested in taking one of your courses, where’s the best place for somebody to find you on the internet?
BR: RondeauSeminars.com. The American Academy of Dental Sleep Medicine also has many courses, and their website is aadsm.org.
A 40-year-old female patient was snoring and depressed, because her husband would not sleep with her. The oral appliance successfully stopped the snoring and eliminated her depression and her husband came back to bed. She later said, “Thanks for giving me my life back.”
MD: I can personally vouch for your courses, they are all extremely practical, so I personally recommend your courses as a great jumping off point for most dentists. But you said the Academy has some as well?
BR: Yes, the Academy has them as well. You should join the Academy and get to work towards your certification and practice within the guidelines of the Academy. But I honestly think that if dentists really embrace this and start talking to pulmonologists or sleep center specialists in their area and work with the medical profession, that they’re going to have a very successful practice, and it’s going to impact the bottom line very positively. It’s a great service and it’s great knowing that you’re helping people live longer and you’re improving their quality of life. Although snoring and sleep apnea is more prevalent among males, I also have some female patients with these sleep disorders. One particular female patient was excessively tired and extremely depressed because her husband would not sleep with her due to her snoring problems. When I fabricated an oral appliance for her, it literally changed her life. She stopped snoring, her daytime sleepiness disappeared, and she went off her depression medication. Her husband came back to the bedroom and she felt loved again. The first month after inserting the oral appliance she jumped out of the dental chair, gave me a big hug and said, “Thanks for giving me my life back.” It’s nice to make money and it’s nice to have a successful practice, but it’s extremely rewarding to do it by helping people. And your lab does that by fabricating oral appliances for our patients. Your lab also provides education to dentists through your Chairside® magazine and I think it’s a valuable service that you’re providing.
MD: It’s funny you mention that because I think every dentist has had some experience with a crown and bridge case or veneer case where the patient was so happy she cried and she gave the dentist a hug. But I’ll tell you just what I’ve seen from doing all types of dentistry, there’s a lot more hugs and a lot more gratitude on the part of the sleep apnea patients, the patient who has felt like crud and run down and is falling asleep during the day and worried they’re going to kill somebody else when driving. And now, all of a sudden, they feel good again and they remember what it felt like to actually feel good on a daily basis.
BR: Well, particularly if it’s 15% to 30% of the adult population that has the problem. I think if you just get all of your snoring patients to fill out the Epworth Sleepiness Scale you will see this is true. The other thing is that it’s a good idea to get his wife to fill it out, too, because sometimes men will underestimate how sleepy they are, and the wives will always score higher. At the consultation appointment the women will frequently say to their husbands: “What do you mean you don’t fall asleep in front of the TV? You fall asleep every night in front of the TV!” The cardiologists are starting to get involved now, and they’re seeing a significant increase in cardiovascular diseases. It appears there’s a definite correlation between CVD and sleep apnea, so we need to get in there and get these people screened faster and treated faster. That’s why I think these overnight sleep studies are going to go over well and be much more cost-effective than going for the overnight sleep study at the hospital for mild to moderate cases.
MD: Well, you know, these sleep apnea patients are kind of the lost segment of the population that are different from some of the high visibility diseases like hypertension, diabetes and cancer, for example. Those get a lot of dollars and tons of ad space. Sleep apnea is relatively quiet, but unfortunately, it kills its fair share of people, so I think you’re absolutely right: It’s a great thing for your practice but more importantly, it’s a great thing for your patients. It’s been a pleasure, Brock — thanks for your time!
Clinical photos provided by Sleep Group Solutions, 16840 NE 19th Avenue, North Miami Beach, FL, 33162. 866-353-3936. sleepgs.com.