Basic Procedures: An Excerpt from REALITY Publishing’s ‘The Techniques, Vol. 1’

There are numerous tasks in dentistry that are repeatedly performed and are common to many specific procedures. We have detailed these tasks in this article. The tasks are listed in roughly the order in which you would encounter them as you progress through a procedure.
Mark Occlusion Before Preparation (Figs. 1, 2)
This should actually be done at the exam appointment to determine whether the occlusal contact areas of a tooth fall on enamel or on an existing or planned restoration. By knowing the location of these contacts, you will be better able to advise your patient on the best restoration. For example, if you are restoring a mandibular second molar, a tooth which presumably is most susceptible to wear, and the centric stop is squarely on the restorative material, you would want to inform the patient that a material with superior wear resistance would be a prudent choice. In addition, if the tooth has an abfraction lesion, removing eccentric contacts could prevent the lesion from enlarging and may relieve dislodging forces from a subsequently placed restoration.
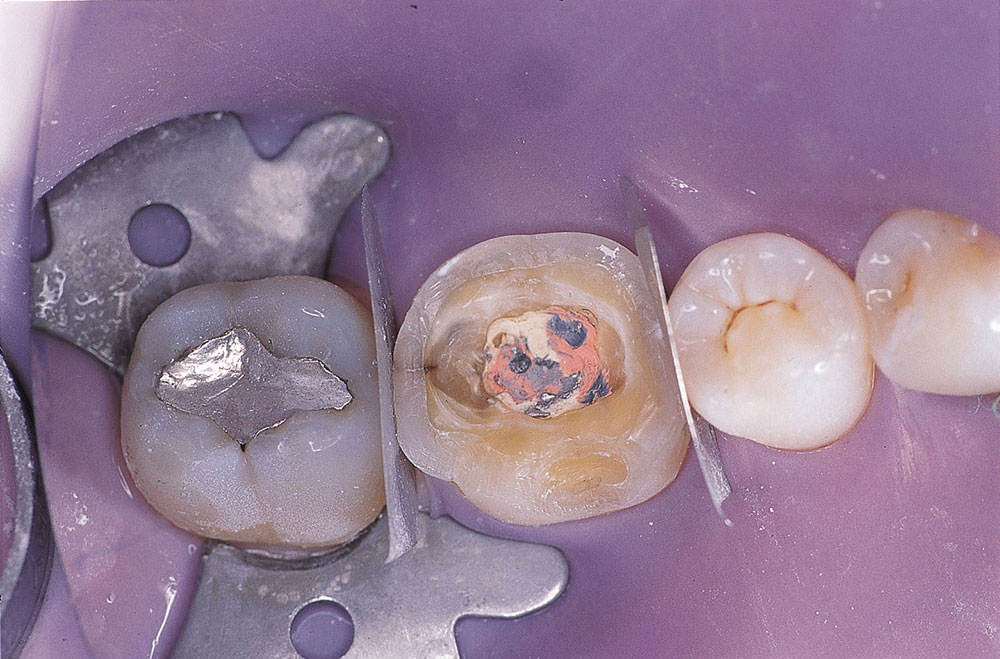
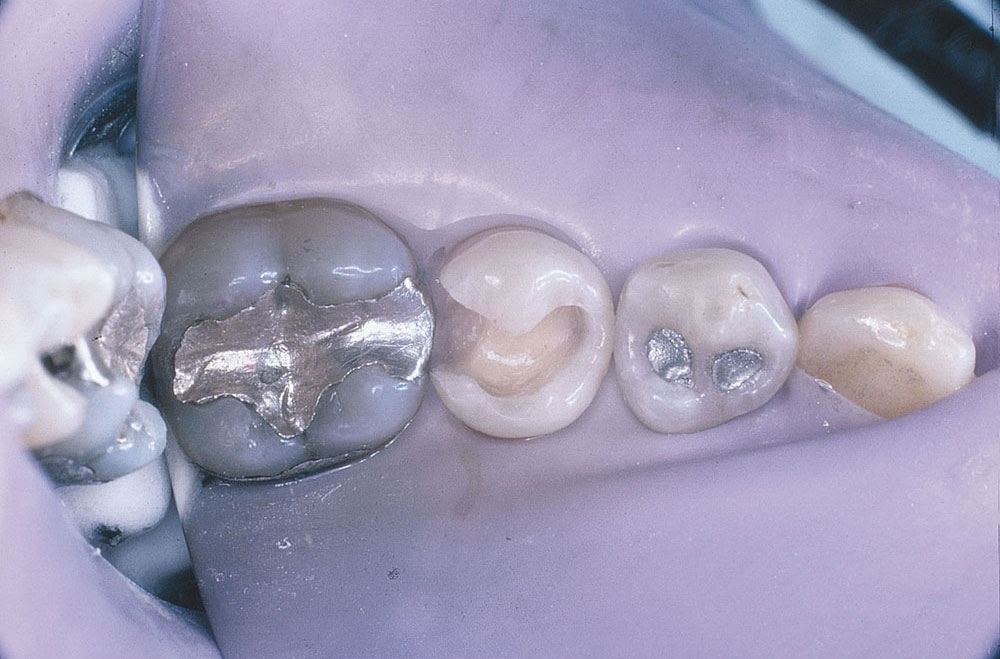
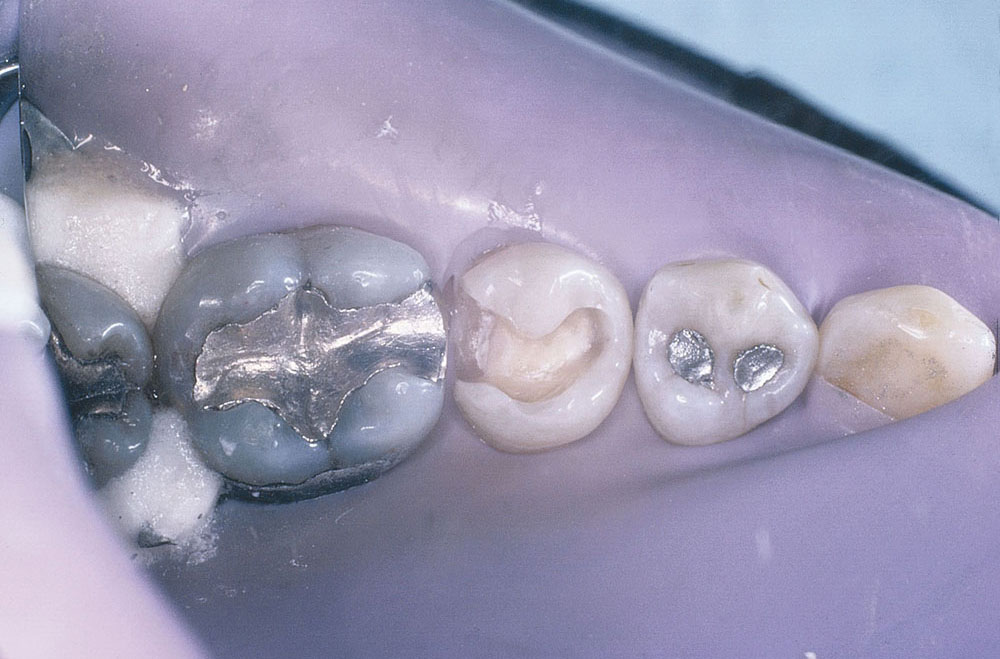
Check Existing Restorations Before Preparation (Figs. 3–5)
If there are existing restorations in teeth destined for full coverage, they should be carefully checked and replaced if there is any doubt at all as to their adequacy to serve as buildups. A good rule of thumb is: If you did not recently (within two to three years) place the restorations yourself, they should be replaced now. This can be done prior to beginning the actual crown preparation or be delayed until the gross preparation is finished.
The shade of composite used to replace faulty restorations is not critical, but should be in the same general shade range as the teeth, assuming the definitive restoration will be fabricated without metal support. This is especially true when the definitive restoration is fabricated from a relatively translucent ceramic or resin material.
On the other hand, when a metal-based restoration is planned, using a buildup material that contrasts with tooth structure can be advantageous because this contrast helps you see the transition from buildup to tooth and, therefore, ensures that the margin of the restoration will be prepared on tooth structure and not buildup material.

Figure 5: Definitive crowns have been cemented on preparations that were rebuilt with reliably bonded foundations.
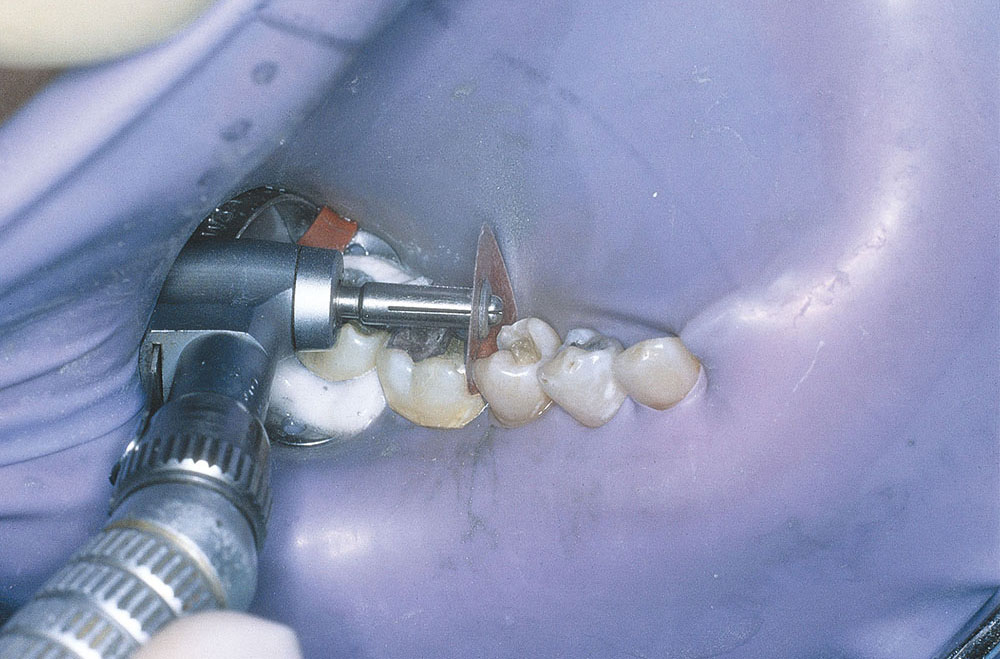
Protect Adjacent Teeth During Preparation (Figs. 6, 7)
Iatrogenic damage to adjacent teeth is widespread. A study, which we reviewed in REALITY NOW #106, found that 78% of 71 Class II cavities resulted in adjacent tooth surfaces being scarred as a result of the preparation. With small preparations, the risk of scarring the adjacent tooth increases.
While specific products such as InterGuard® (Ultradent Products Inc.; South Jordan, Utah) have been developed to prevent this type of damage, a simple (and inexpensive) Tofflemire-like band can also be used. And, because a Tofflemire-like band is relatively long and thin, it can also be “sawed” through a tight contact. To use a Tofflemire-like band, you would typically need to cut off the excess once it is in place, so it does not interfere with the procedure.
However, cutting a band once it is already in place can leave sharp edges and corners. If you are using a rubber dam, this sharpness will probably not be a problem, although it can tear your gloves. But without the dam, it can lacerate a tongue and/or cheek. Therefore, be sure to round the cut corners.
CAUTION: The thinness of a Tofflemire-like band, which makes it easier to place through a tight contact, can actually be a disadvantage because it is not difficult to cut through the band with a sharp carbide bur or diamond. Using a thin band may give you a false sense of confidence. If you repeatedly “nick” it during the preparation, you can still damage the adjacent tooth. You can also penetrate through a Tofflemire-like matrix with air abrasion. Therefore, if you can get a thicker protective device such as InterGuard through the contact, it would be a safer alternative.
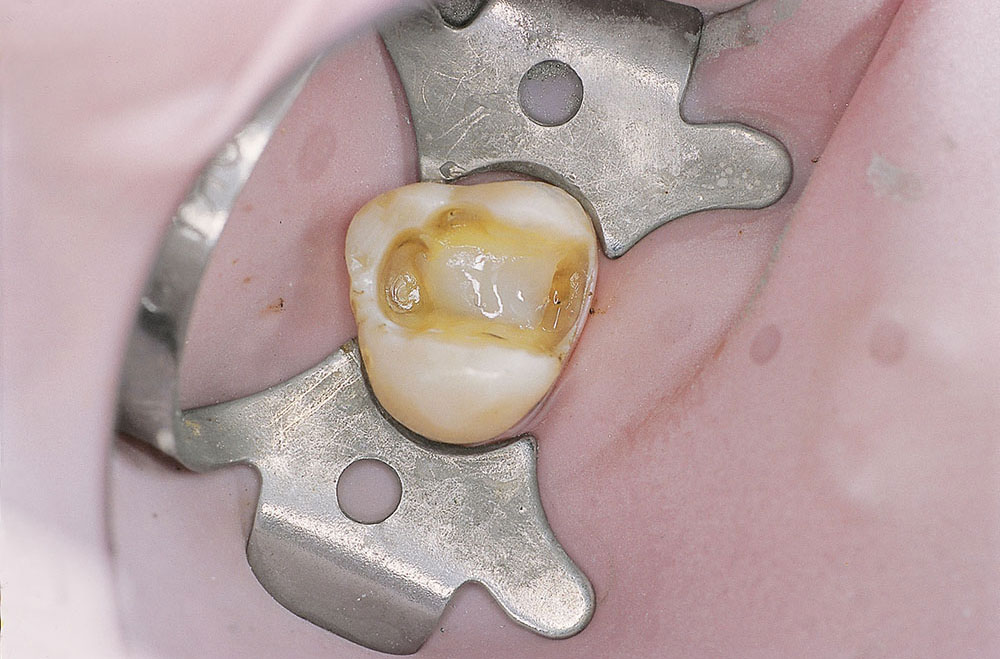
Apply Caries-Detecting Dye and Remove Carious Lesion (Figs. 8–14)
Even though their efficacy has been seriously challenged, 68% of the REALITY Editorial Team still uses a product in this category at least some of the time. If you do use one of these products, apply for 10 seconds and rinse. Any stained tooth structure is then removed with the least destructive instruments, typically slow-speed burs and spoon excavators. Reapply the dye and repeat the removal of any stained tooth structure until the dye no longer stains the tooth. Discretion needs to be used, however. If you are getting close to the pulp and the dentin is still staining, you should stop removing any additional tooth structure.

Figure 14: Caries-detecting dye has been applied and rinsed, revealing stained carious tooth structure. Darker dyes are sometimes preferred to the original red color for more contrast, especially as the lesion approaches the pulp.
Pulp Protection (Figs. 15, 16)
With a properly sealed restoration, pulp protection is not necessary. However, you need to guard against mechanical trauma to the pulp. If there is no exposure, you can proceed with the rest of the procedure, being careful not to put pressure on thin dentin over the pulp. To protect against mechanical trauma, place a small amount of a flowable material (composite, compomer or resin ionomer) over the pulp. With mechanical exposures, achieving hemostasis is the most important aspect. Once hemostasis is accomplished, you can proceed with the rest of the adhesive procedures.
Using a sterile cotton pellet that has been dipped in 5% sodium hypochlorite (Clorox, but check the concentration on the bottle) and then blotted to make it damp, apply pressure for 20–60 seconds, depending on the size of the exposure. Gentle rinsing with sterile saline and hemostasis should follow. Then proceed with adhesive procedures, again using a flowable material to prevent mechanical trauma to the pulp.
With a carious exposure, no suppuration should be present. If there is suppuration, endodontic treatment is inevitable. Otherwise, slight bleeding is probably advantageous because it may help remove some of the bacterial invasion of the pulp. In fact, if a carious exposure does not bleed, it may be advantageous to induce slight hemorrhaging to remove some of the bacterial invasion. Then proceed with the same procedure as described for mechanical exposures.
In a recent REALITY Editorial Team survey, 88% of the members stated that they have bonded over exposed pulps. It was also estimated by these editorial team members that this treatment failed in about 18% of the teeth. Therefore, we strongly advise that you inform your patients that, while this treatment has an estimated success rate of about 82%, they still may require endodontics.
Check Adjacent Teeth After Preparation (Figs. 17–22)
Be sure to check the adjacent tooth surface for possible caries or to smooth existing restorations. If proximal caries exists in the adjacent tooth, this is the optimal time to restore it. At this point, you have direct access to the carious lesion, allowing the most conservative preparation possible. If the adjacent tooth has a rough, overcontoured or overhung restoration, it should be smoothed and/or recontoured with finishing discs or finishing burs, if access permits.
However, when the contact is not broken, you may not have access to completely smooth an adjacent restoration. In this instance, a finishing strip (aluminum oxide or diamond) would be used instead of a bur or disc. A perforated strip (interproximal scaler) may also be used to clean proximal surfaces of hard adherents prior to placing the restoration.
Dr. Michael Miller is the co-founder, president and editor-in-chief of REALITY. He maintains a dental practice in Houston, Texas. Contact him at a mm@realityesthetics.com
Reprinted by permission of REALITY Publishing Company. © 2003 REALITY Publishing Co. Vol. 1, The Techniques, pp. 11–14.