Inspired by a passion for improving lives through oral health, Glidewell Clinical Education provides contemporary, continuing education for dental professionals. Read our chief publication, Chairside® magazine, for cutting-edge clinical techniques and industry news, or take a free online CE course to expand your skillset. Listen to our “Chairside Live: Dental Insights” podcast or check out our library of over 10,000 education videos.
Dental Education
-
 Online CE CourseIntroduction to Digital Dentistry for the Dental Auxiliary
Online CE CourseIntroduction to Digital Dentistry for the Dental Auxiliary -
 Online CE CourseIntroduction to Dental Sleep Medicine
Online CE CourseIntroduction to Dental Sleep Medicine -
.png/_jcr_content/renditions/thumb-png-mobile-full.png) Online CE CourseImplant Treatment Planning: The Contributing Factors
Online CE CourseImplant Treatment Planning: The Contributing Factors -
 Online CE Course4 Ways to Provisionalize Dental Implants
Online CE Course4 Ways to Provisionalize Dental Implants -
 Online CE Course10 Things I Learned the Hard Way
Online CE Course10 Things I Learned the Hard Way -
 Online CE CourseGuided Bone Regeneration: 8 Steps to Successful Ridge Augmentation
Online CE CourseGuided Bone Regeneration: 8 Steps to Successful Ridge Augmentation -
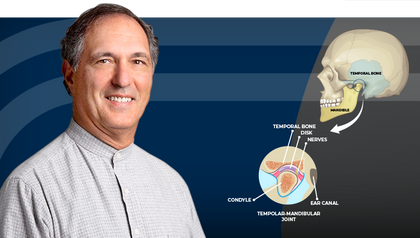 Online CE CourseTemporomandibular Disorders and the Human Jaw
Online CE CourseTemporomandibular Disorders and the Human Jaw -
 Online CE CourseRestoration of Implant Overdentures
Online CE CourseRestoration of Implant Overdentures -
 Online CE Course11 Steps to Increase Practice Production Right Away – Part 2
Online CE Course11 Steps to Increase Practice Production Right Away – Part 2 -
 Online CE CourseUsing Laboratory-Fabricated Provisionals
Online CE CourseUsing Laboratory-Fabricated Provisionals
-
 Online CE CourseTreatment Planning for Single-Unit Implant PlacementTreatment planning for single-unit implant placement requires a comprehensive understanding of biological, esthetic, and functional principles. In this course, Dr. Taylor Manalili will introduce a top-down treatment planning approach, integrating digital technology to optimize outcomes.
Online CE CourseTreatment Planning for Single-Unit Implant PlacementTreatment planning for single-unit implant placement requires a comprehensive understanding of biological, esthetic, and functional principles. In this course, Dr. Taylor Manalili will introduce a top-down treatment planning approach, integrating digital technology to optimize outcomes. -
 Online CE CourseSuccess with Local Anesthesia: Key Drug Properties, Dose Updates and Buffering Local AnestheticsIn this course, Kathy Bassett will thoroughly explore the key pharmacological properties influencing profound anesthesia. Participants will review the latest guidelines for local anesthetic dosing and labeling to ensure safe usage.
Online CE CourseSuccess with Local Anesthesia: Key Drug Properties, Dose Updates and Buffering Local AnestheticsIn this course, Kathy Bassett will thoroughly explore the key pharmacological properties influencing profound anesthesia. Participants will review the latest guidelines for local anesthetic dosing and labeling to ensure safe usage. -
 Online CE CourseBenefits of Clear Aligner TherapyThis course offers an in-depth look into clear aligner orthodontic therapy, emphasizing both theoretical understanding and practical application. Participants will gain insights into the benefits of expansive versus retractive orthodontics, explore various arch forms and their relationship with malocclusion, and learn a systematic diagnostic protocol for identifying malocclusions.
Online CE CourseBenefits of Clear Aligner TherapyThis course offers an in-depth look into clear aligner orthodontic therapy, emphasizing both theoretical understanding and practical application. Participants will gain insights into the benefits of expansive versus retractive orthodontics, explore various arch forms and their relationship with malocclusion, and learn a systematic diagnostic protocol for identifying malocclusions.
The best educational resource in the dental industry