Principles of Implant Occlusion: Part 4 — Recommendations for Removable Implant Prostheses
Ideal occlusion is of paramount importance for the long-term success of implant-supported restorations, yet controversy exists regarding the correct occlusal schemes for removable implant prostheses. Unfortunately, most occlusal guidelines for removable implant prostheses are derived from principles established for conventional removable prostheses, rather than based on the type and support system of the specific implant overdenture. In the literature, limited information is available on a classification system that relates to the number of implants, position of implants, arch form, occlusal force, opposing occlusion, primary support system and other considerations needed to establish proper occlusion for removable implant prostheses. Therefore, Part 4 of this series will discuss the various factors related to treatment planning for removable implant prostheses, including recommendations for an ideal occlusal scheme with respect to the type of overdenture.
OVERDENTURE SUCCESS RATES
It has been documented that implant-supported overdentures have a higher rate of failure than fixed implant prostheses. Goodacre et al. showed that the implant-supported overdenture has the highest complication rate of any type of implant prosthesis. Overdentures were shown to exhibit retention problems (30 percent), reline indications (19 percent), attachment fractures (17 percent), and prosthesis fractures (12 percent). Maxillary overdenture implants showed a failure rate of 19 percent, while mandibular overdenture implants resulted in failures only 4 percent of the time.1 The maxillary overdenture is at more risk in comparison to mandibular overdentures because of poorer bone quality, increased bone atrophy, interocclusal space limitations, esthetics and anatomic considerations (i.e., osseous angulation, nasal cavity, maxillary sinus and nasopalatine canal).
Jacobs concluded that the implant overdenture prosthesis is highly susceptible to occlusal-related issues, as patients with overdentures exhibit the lowest sensitivity in detecting damaging premature occlusal forces.2 While patients with natural teeth have demonstrated the capacity to detect an occlusal prematurity at approximately 20 microns, overdenture prematurities are detected at approximately 108 microns. Therefore, patients are less likely to be aware of occlusal-related complications, and there is a decrease in the patient’s perception of damaging forces. This is significant, as studies have shown that premature contacts may cause myofascial dysfunction-related issues and occlusal force is significantly increased when high or premature occlusal contacts are present.3
Thus, the prosthetic occlusal scheme for an implant overdenture is one of the most significant factors that can lead to the failure of dental implants. An improper occlusal design can lead to a concentration of force and stresses on the supporting implants, which will result in bone resorption.4 Fortunately, incorporating the proper occlusal scheme can minimize complications and thereby maximize treatment.
REHABILITATING THE FULLY EDENTULOUS ARCH WITH A REMOVABLE IMPLANT PROSTHESIS
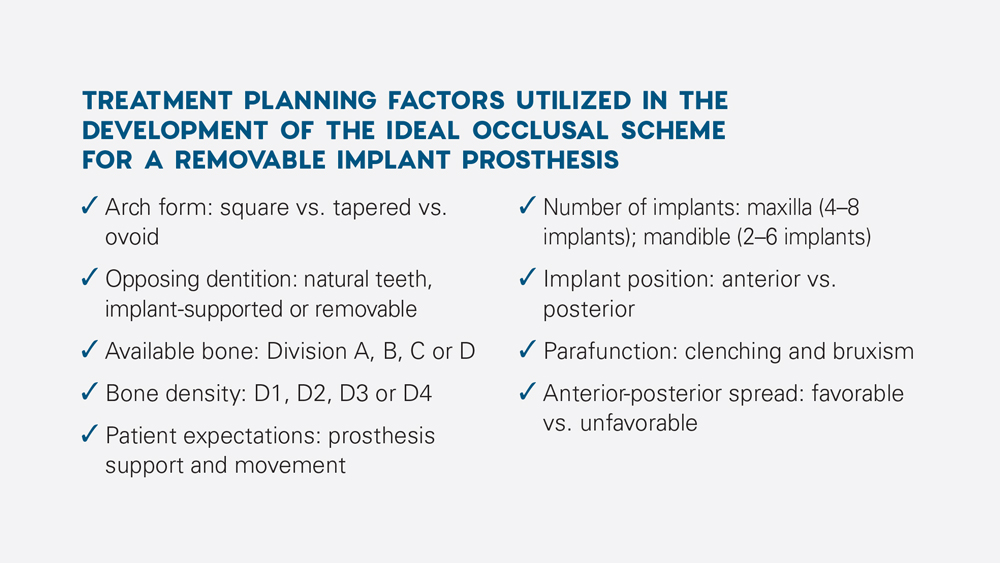
When treatment planning an implant overdenture, there are many variables to consider in order to optimize the longevity of the implants, attachments and prosthesis. It is imperative that the clinician integrate these treatment planning factors into the design of the prosthesis and evaluation of the ideal occlusal scheme. Various factors that should be taken into consideration include arch form, opposing dentition, available bone, bone density, patient expectations, number of implants, implant position, parafunction and anterior-posterior spread.
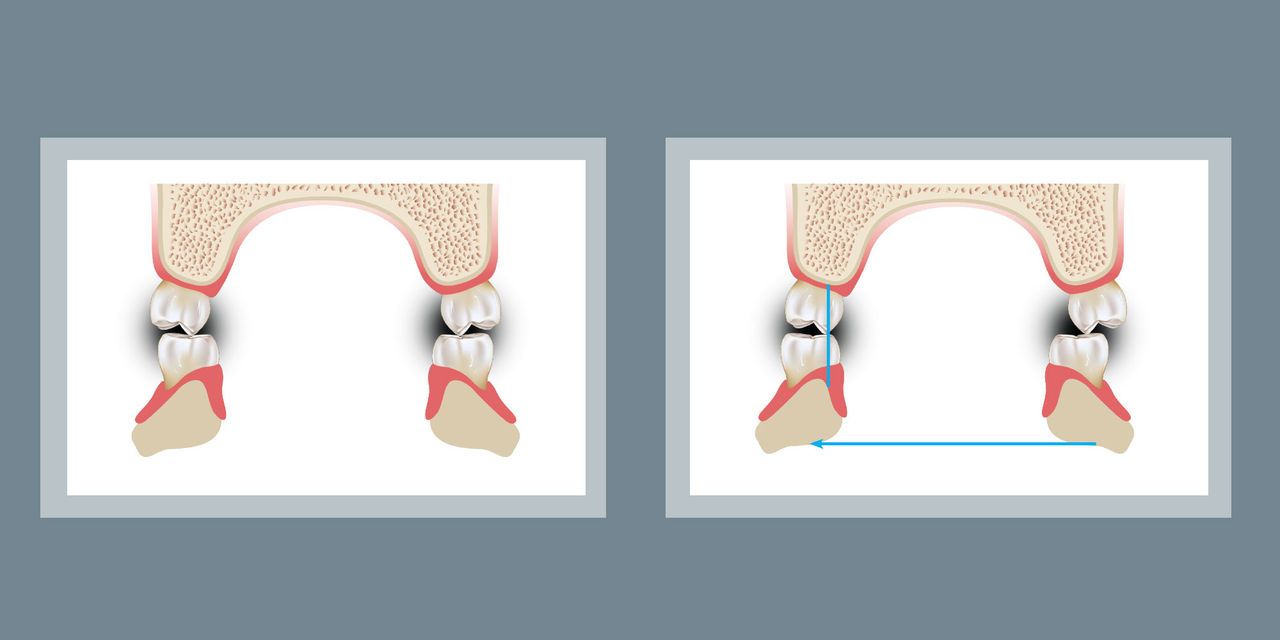
In addition to considering the aforementioned treatment planning factors, it is important to distinguish between the two types of removable implant overdentures. The Misch classifications differentiate overdentures into two specific prosthesis types, which are related to the kind of support system: The RP-4 prosthesis is totally supported by implants, with no support from the soft tissue (Figs. 1a, 1b), and the RP-5 prosthesis is primarily soft-tissue supported, with secondary implant support (Figs. 2a, 2b). Failure to differentiate between these two types of prostheses may lead to restorative decisions resulting in prosthesis failure, related complications, and patient expectation issues.
It is important to distinguish between the two types of removable implant overdentures.
With the fabrication of an RP-5 prosthesis, the primary stress-bearing tissue surfaces must be taken into consideration. The primary stress-bearing areas are defined as the anatomical locations most capable of withstanding the masticatory load in providing support for the prosthesis. These areas are usually consistent with tightly adhered fibrous connective tissue, tightly bound keratinized tissue, the presence of cortical bone, and anatomically located right angles to the vertical occlusal forces. With RP-5 prostheses, the primary stress-bearing areas must be utilized to decrease the stress on the implant system.
In the maxilla, the primary stress-bearing areas are the horizontal part of the hard palate, which is lateral to the midline, and the crest of the ridge. In the mandible, they are the buccal shelves, which are bounded medially by the crest of the ridge, laterally by the external oblique ridge and distally by the retromolar pad (Figs. 3a, 3b).
 Figure 1a
Figure 1a
 Figure 1b
Figure 1b
Figures 1a, 1b: Maxillary (1a) and mandibular (1b) examples of an RP-4 prosthesis, which is completely implant-supported, with no soft-tissue support. Note how the maxillary prosthesis has minimal palatal support and the mandibular prosthesis has minimal soft-tissue coverage and extension.
 Figure 2a
Figure 2a
 Figure 2b
Figure 2b
Figures 2a, 2b: The RP-5 prosthesis is primarily soft-tissue supported, with secondary implant support. Shown here is a maxillary RP-5 overdenture with complete palate (2a), as well as a mandibular prosthesis with buccal shelf support (2b).
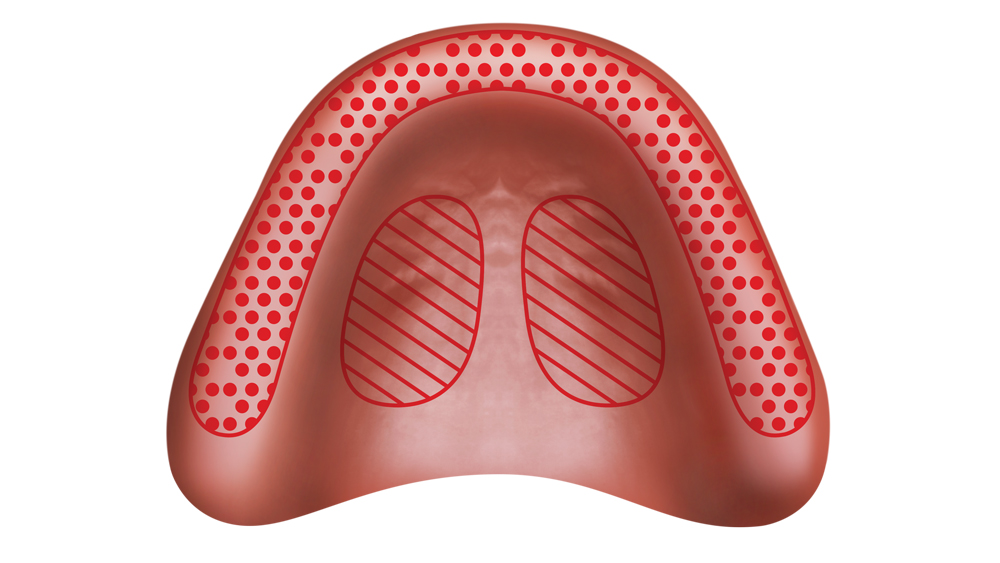 Figure 3a
Figure 3a
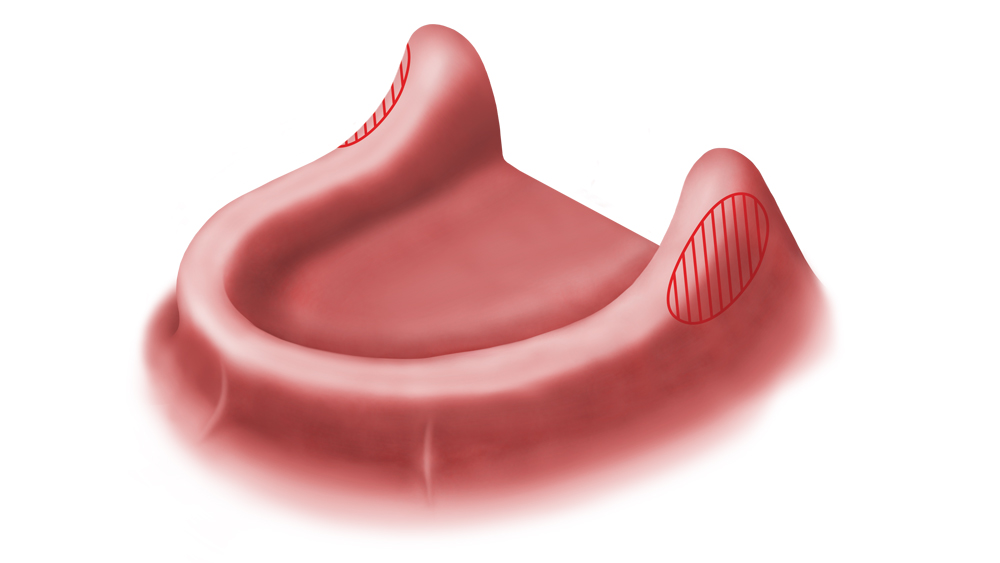 Figure 3b
Figure 3b
Figures 3a, 3b: The primary stress-bearing areas for an RP-5 include the ridge crest and horizontal palate for the maxilla (3a), and the buccal shelves for the mandible (3b).
OCCLUSION FOR A REMOVABLE IMPLANT PROSTHESIS (RP-4 AND RP-5)
After the prosthesis classification has been established based on the type of support system (i.e., implant- or tissue-supported), a determination can be made for the ideal occlusal scheme.
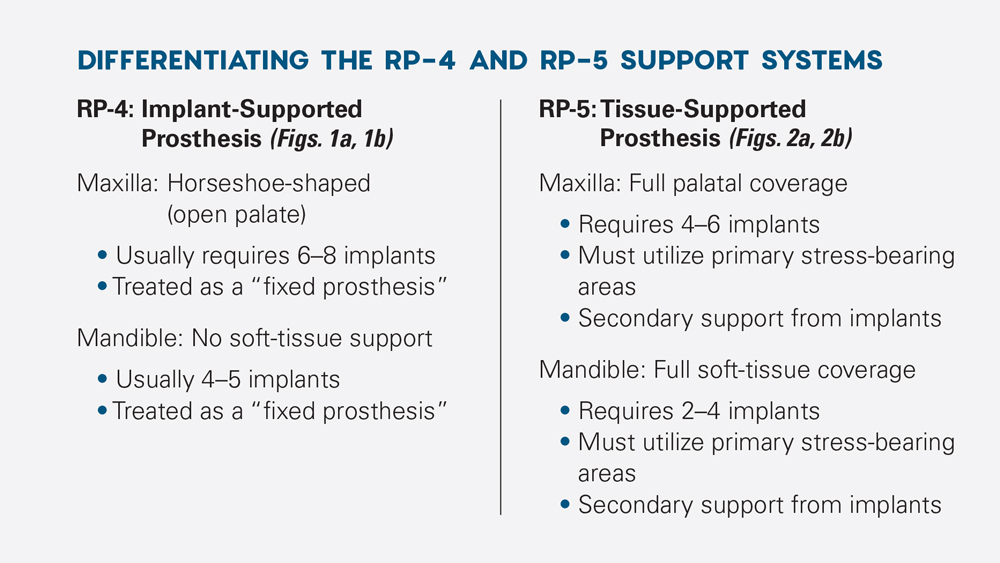
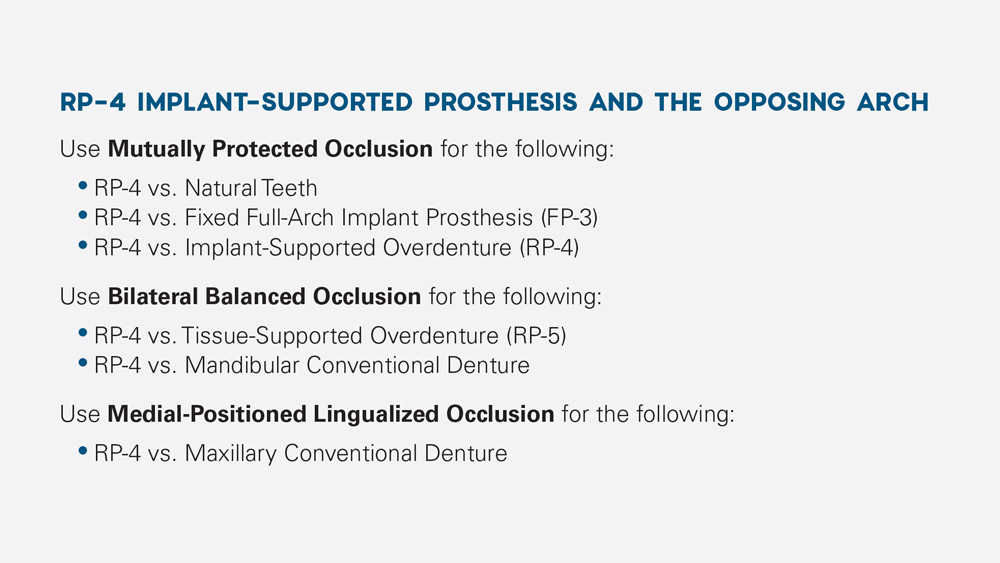
1. RP-4 Implant Prosthesis: The maxillary or mandibular RP-4 implant prosthesis should be treated as a “fixed prosthesis.” Because this type of prosthesis has no soft-tissue support for the distribution of occlusal forces, theoretically no movement of the prosthesis should occur. For an RP-4 prosthesis, mutually protected occlusion is recommended when the RP-4 restoration opposes an arch with natural dentition or an arch that is restored with a fixed full-arch implant prosthesis (FP-3) or RP-4. Mutually protected occlusion consists of the anterior teeth protecting the posterior teeth and the posterior teeth protecting the anterior teeth in all excursive mandibular movements. The mutually protected occlusal scheme was discussed in detail in Part 3 of this article series.
The bilateral balanced occlusal scheme is used when the opposing arch is an RP-5 prosthesis or mandibular conventional denture. A special form of bilateral balanced occlusion, known as medial-positioned lingualized occlusion, is utilized when an RP-4 opposes a maxillary conventional denture. See “Discussion” below for more on these occlusal schemes.
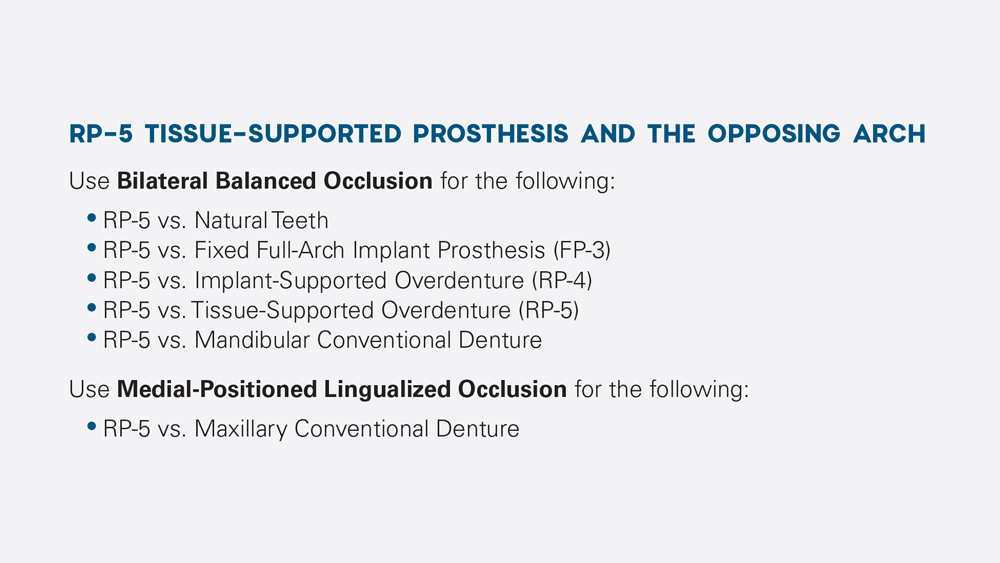
2. RP-5 Implant Prosthesis: The maxillary or mandibular RP-5 implant prosthesis is a soft-tissue supported prosthesis with a secondary support system (i.e., implants and attachments). Therefore, an RP-5 prosthesis should be treated as a soft tissue-supported prosthesis, not an implant-supported prosthesis, and bilateral balanced occlusion is recommended.
Bilateral balanced occlusion is used when the RP-5 restoration opposes an arch with natural dentition or one that is restored with an FP-3, RP-4, RP-5 or mandibular conventional denture. Medial-positioned lingualized occlusion is used only when the mandibular RP-5 prosthesis opposes a maxillary conventional denture.
DISCUSSION: BILATERAL BALANCED OCCLUSION AND LINGUALIZED MEDIAL-POSITIONED OCCLUSION
I. Bilateral Balanced Occlusion
The bilateral balanced occlusion concept dictates the simultaneous contact of all the teeth bilaterally in centric occlusion and eccentric excursions. The rationale for bilateral balanced occlusion is that the occlusal loads are evenly distributed across the dental arch, which stabilizes the prosthesis in centric occlusion as well as in eccentric and parafunctional movements. A completely balanced occlusal scheme may be developed with any cusp type as long as a compensation curve, in which the anterior-posterior and lateral curvature are aligned with the incisal and occluding surfaces of the artificial teeth, exists (Figs. 4a–4d).
The rationale for bilateral balanced occlusion is that the occlusal loads are evenly distributed across the dental arch.
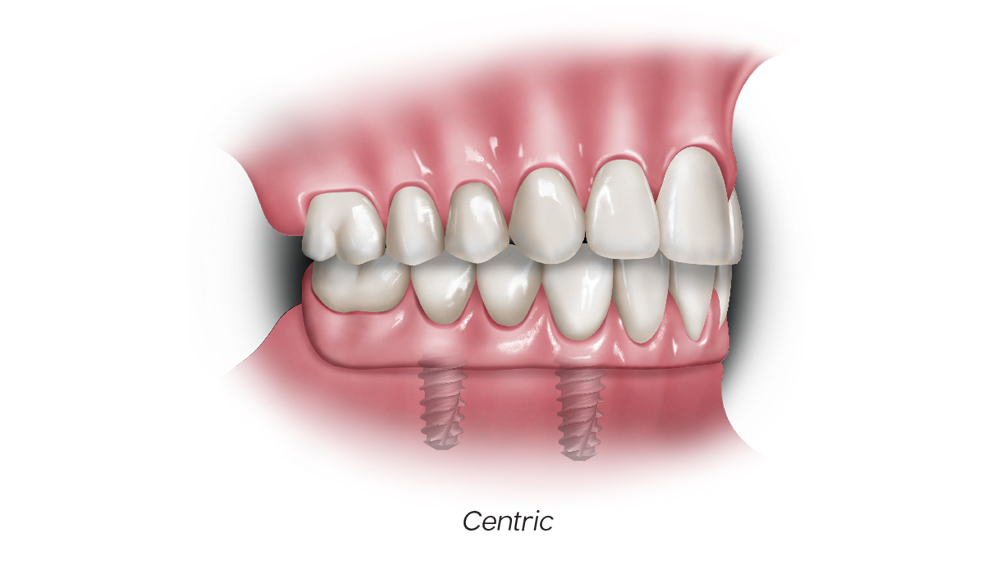 Figure 4a
Figure 4a
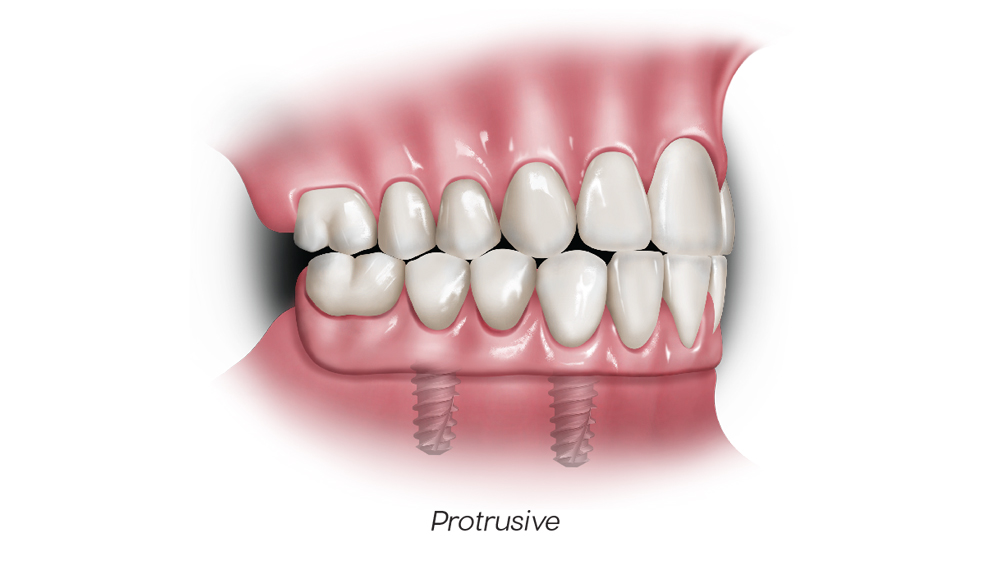 Figure 4b
Figure 4b
 Figure 4c
Figure 4c
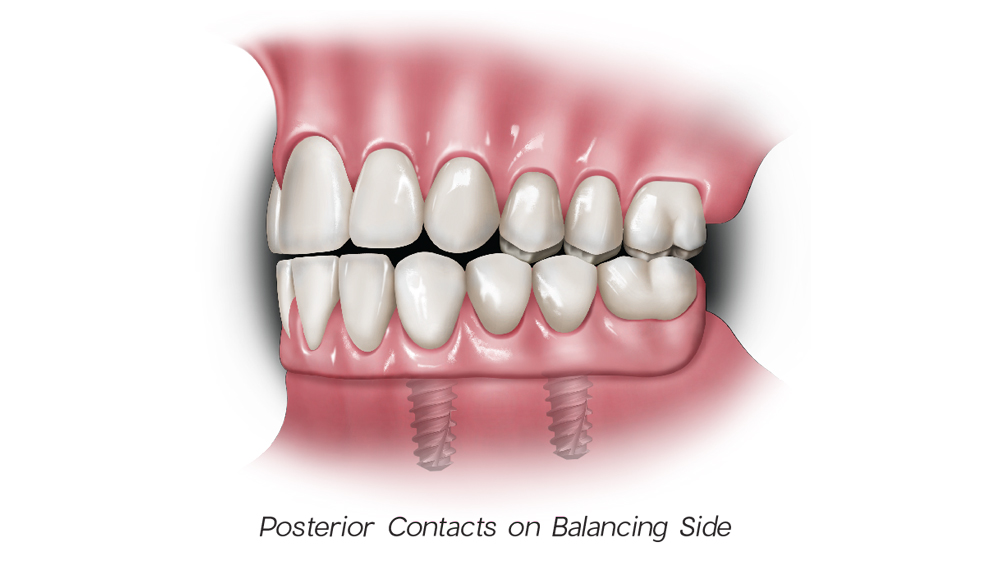 Figure 4d
Figure 4d
Figures 4a–4d: Bilateral balanced occlusion: In centric occlusion, anterior and posterior simultaneous contact should be present (4a). Upon protrusive movement, bilateral simultaneous contacts are present (4b). During right lateral excursion, posterior contacts are present on the working and balancing sides (4c, 4d).
II. Lingualized Medial-Positioned Occlusion
A type of bilateral balanced occlusion, lingualized occlusion is an alternative first described by Dr. S. Howard Payne in 1941, then modified by Dr. Earl Pound, and further modified by Dr. Carl E. Misch in 1988.5-7 This type of occlusion utilizes the maxillary lingual cusps as the major functional occlusal unit and opposes mandibular zero-degree or shallow-cusp teeth. This occlusion concept integrates anteroposterior and mediolateral compensating curves in the mandibular arch, which permit balanced occlusion between the maxillary lingual cusps and the mandibular teeth during excursive movements. Therefore, the lingualized occlusion is preferred by many in order to eliminate or reduce lateral stress, especially if a maxillary conventional denture opposes an implant-supported prosthesis. Studies have shown that chewing efficiency and patient preference are superior with 30-degree maxillary teeth opposed by nonanatomic mandibular teeth.8
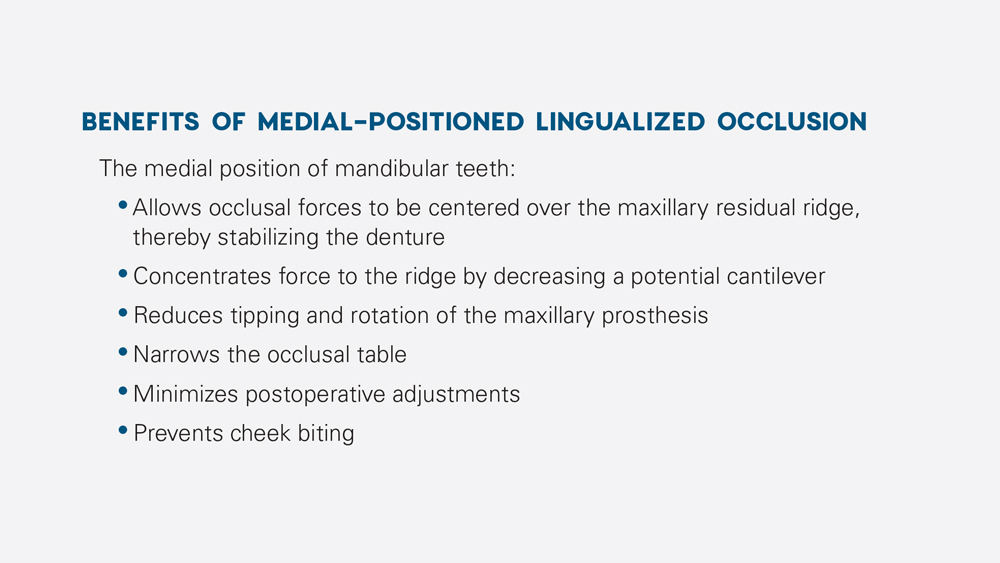
The original lingualized occlusal concept was modified by Dr. Misch to include a medial position of the mandibular teeth (i.e., medial-positioned lingualized occlusion). Because the maxillary edentulous ridge resorbs in a medial direction, the maxillary teeth are usually positioned lateral to the bony support, resulting in a cantilevered situation. Dr. Misch concluded that this type of occlusal design allows the mandibular teeth to be in a more favorable position to obtain denture stability and support (Figs. 5a, 5b). The more medial the posterior denture teeth, the more vertical the occlusal forces over the maxillary bone. This position results in reducing the tipping and rocking of the prosthesis and increases the upper denture stability during function, especially excursive movements (Figs. 6a, 6b).
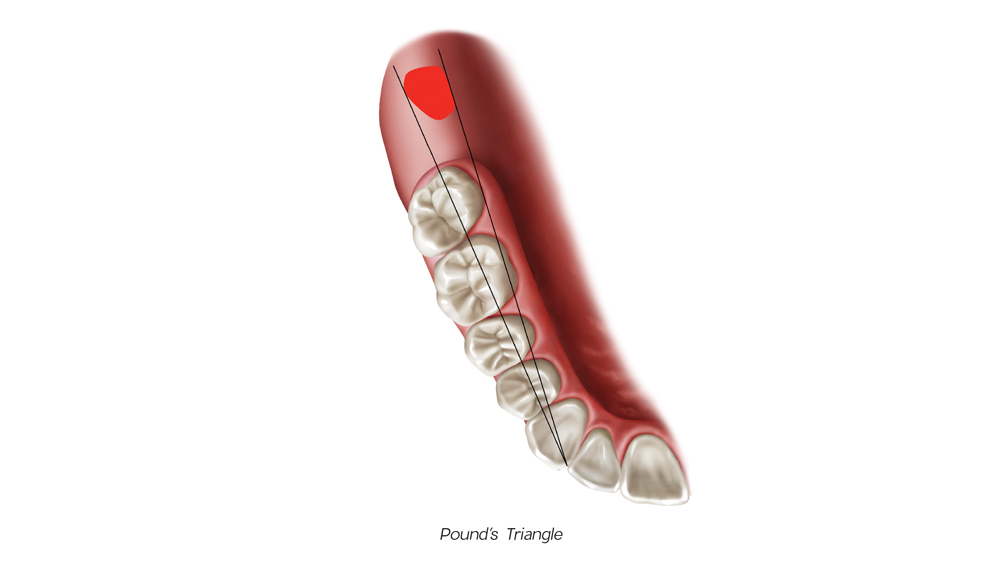 Figure 5a
Figure 5a
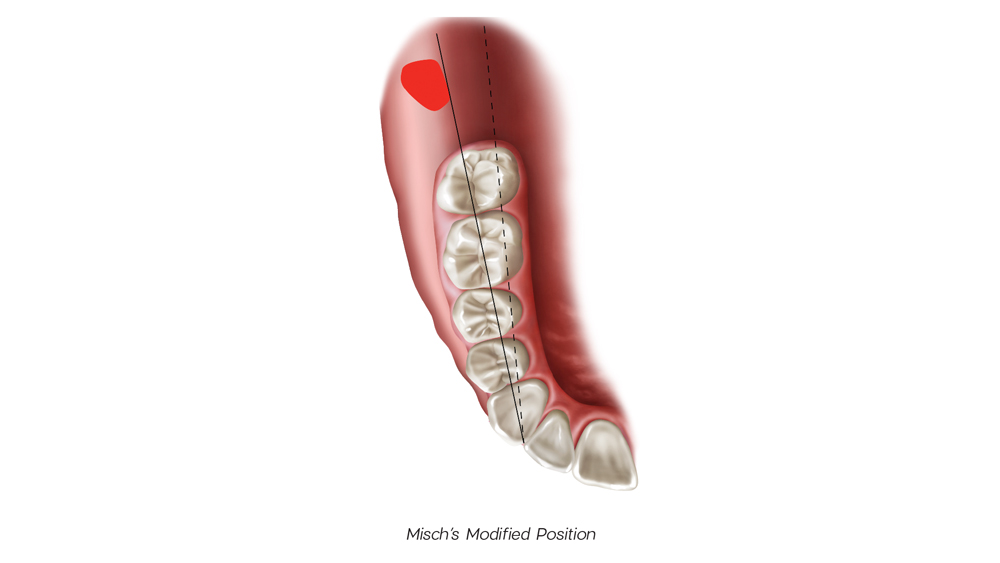 Figure 5b
Figure 5b
Figures 5a, 5b: Pound’s triangle (5a) is created by drawing two lines from the mesial aspect of the canine to both sides of the retromolar pad. This positions the lingual aspects of the mandibular teeth within the triangle. Misch’s modified position (5b) includes a line extending from the mesial aspect of the canine to the medial aspect of the retromolar pad. The central fossae of the mandibular posterior teeth are then positioned slightly buccal to this line, which results in the lingual surfaces being slightly lingual to the line.
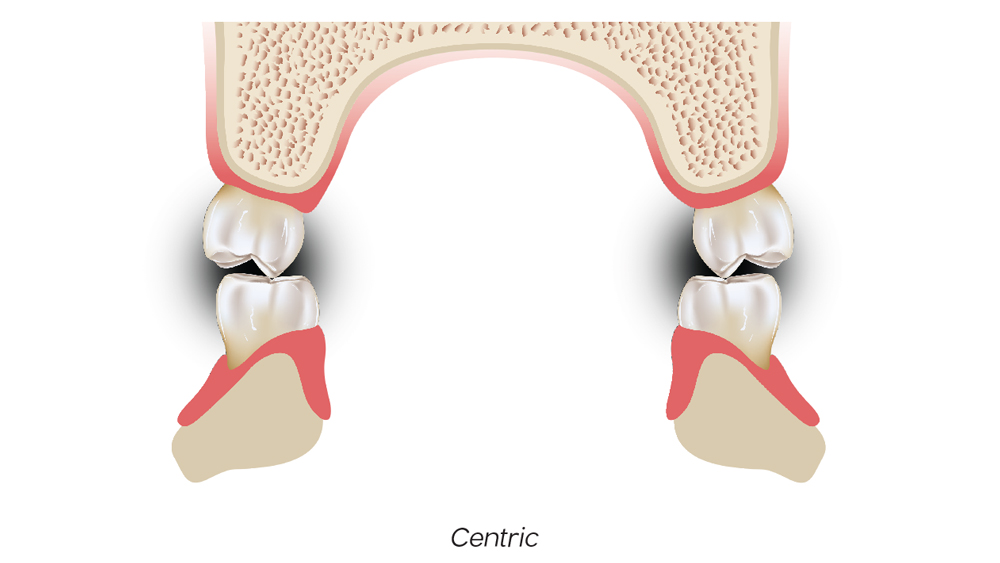 Figure 6a
Figure 6a
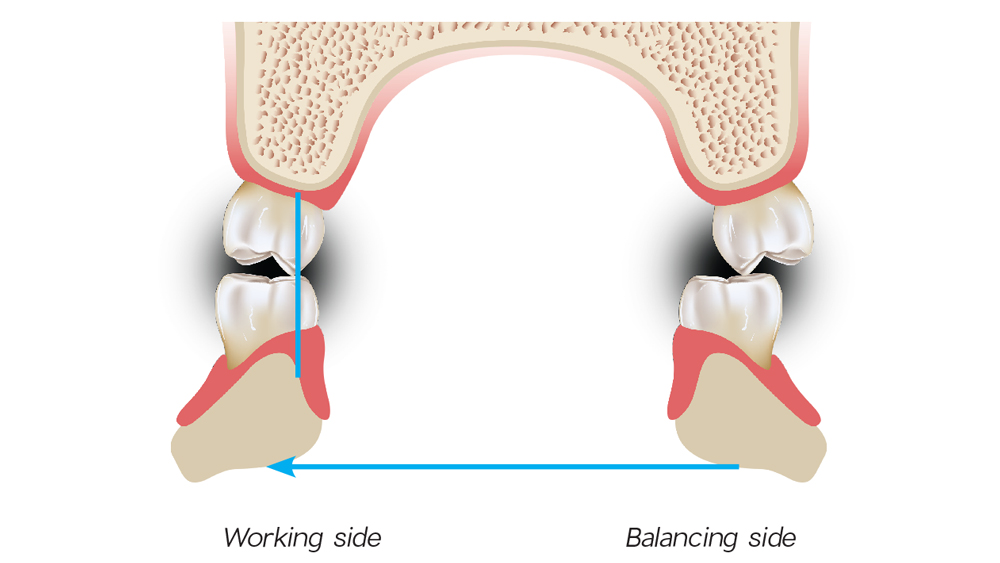 Figure 6b
Figure 6b
Figures 6a, 6b: Medial-positioned lingualized occlusion: The original lingualized occlusal concept was modified by Dr. Misch to include a medial position of the mandibular teeth.
CONCLUSION
As with any treatment modality, it has been shown that implant-retained overdentures are susceptible to complications if not planned appropriately. A strict adherence to the principles differentiating an RP-4 vs. RP-5 implant prosthesis should be followed for optimal long-term function. Particular caution should be exercised to prevent fabricating an RP-4 prosthesis when treatment planning factors and implant support point toward an RP-5. Patients with removable implant prostheses have been shown to have difficulties in recognizing occlusal prematurities. Therefore, the occlusal contacts should be strictly monitored and evaluated on a consistent basis to maintain stability and decrease any occlusal disharmony.
The proper occlusal scheme, as well as the ultimate success of the implants and the prosthesis, is based on careful treatment planning and the consideration of various factors and principles, which will allow for longevity of the restoration and harmony with the surrounding tissues.
References
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003 Aug;90(2):121-32.
- Jacobs R, van Steenberghe D. Comparison between implant-supported prostheses and teeth regarding passive threshold level. Int J Oral Maxillofac Implants. 1993;8(5):549-54.
- Laurell L, Lundgren D. Interfering occlusal contacts and distribution of chewing and biting forces in dentitions with fixed cantilever prostheses. J Prosthet Dent. 1987 Nov;58(5):626-32.
- Lundgren D, Laurell L, Falk H, Bergendal T. Occlusal force pattern during mastication in dentitions with mandibular fixed partial dentures supported on osseointegrated implants. J Prosthet Dent. 1987 Aug;58(2):197-203.
- Payne SH. A comparative study of posterior occlusion. J Prosthet Dent. 1952 Sept;2(5):661-6.
- Pound E. Utilizing speech to simplify a personalized denture service. J Prosthet Dent. 1970 Dec;24(6):586-600.
- Misch CE. Dental implant prosthetics. 2nd ed. St. Louis: Mosby. 2014.
- Khamis MM, Zaki HS, Rudy TE. A comparison of the effect of different occlusal forms in mandibular implant overdentures. J Prosthet Dent. 1998 Apr;79(4):422-9.



