My First Implant with Vincent M. Foring, DMD

Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Dr. Vincent Foring is a general dentist with a thriving private practice in Oakhurst, New Jersey. Since he started placing implants, Dr. Foring has seen the implant case acceptance rate at his practice greatly improve. Here, he discusses how the comprehensive implant training he received simplified his transition to implant surgery, his successful strategy for presenting treatment, and why he believes that all GPs should learn to place implants.
Chairside® magazine: What initially got you interested in placing implants?
Dr. Vincent Foring: I originally got into implants for denture stabilization. I was working in an area where edentulous patients were underserved and didn’t have a lot of money. Conventional implants weren’t an easy sell due to the patients’ financial situation. I took a course on small-diameter implants and learned that you could do a complete case with minis to retain an overdenture for between $2,000 and $2,500. That was a great treatment option for these patients, who really appreciated the extra stability.
CM: How much were you exposed to implants during your dental studies at the University of Pennsylvania?
VF: At Penn they provided us with a lot of training for restoring implants, but not for actually placing them. But in my senior year, I was part of an honors program where we received some training in atraumatic extraction and socket preservation, which offered a bit of surgical exposure. So from the beginning, I was doing extractions and grafts and referring the patient out for implant placement so I could restore the case later.
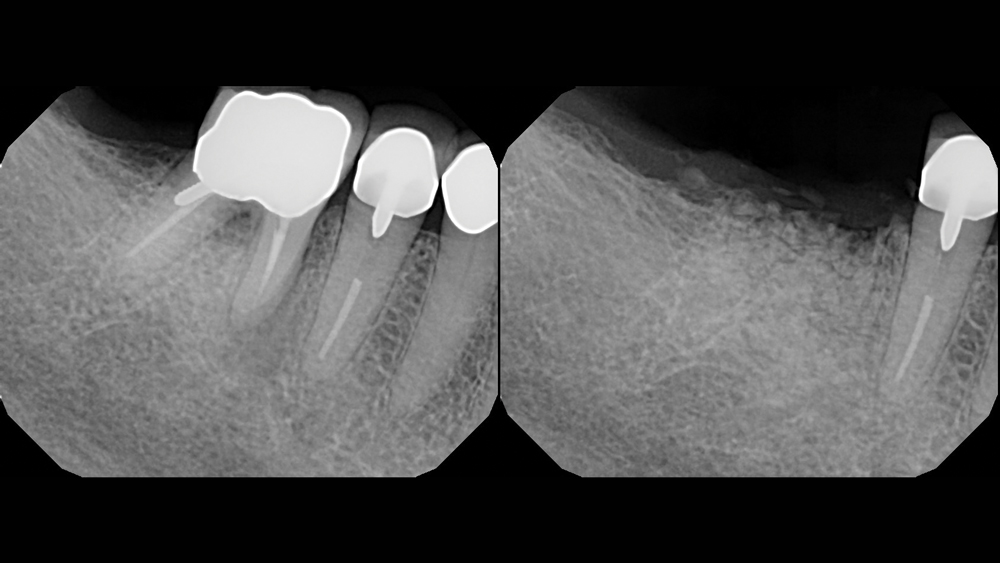
While away on vacation, the patient fractured tooth #30, necessitating removal by a local practitioner, who grafted the extraction socket. When the patient returned home, she sought consultation for tooth replacement. With plenty of ridge width and horizontal bone present, the patient was an excellent candidate for Dr. Vincent Foring’s first implant.
CM: What made you decide that you wanted to move on to conventional implants?
VF: I had been placing mini implants for four years before I decided to look for a course on conventional implant placement. In 2014, I acquired two practices and found that, of all these new patients I was referring out for implant placement, only about 20 percent were accepting the treatment. A lot of the time the problem was that the patient would either not follow through with the consultation because they didn’t want to get involved with another doctor, or they’d go to the consultation and get scared off by the price.
CM: We’ve certainly heard from a lot of practitioners that many patients prefer to stay under the same roof for implant treatment whenever possible.
VF: For sure. People trust and are just more comfortable with their primary-care dentist. Of course, when we refer a case out, we provide a strong recommendation for that specialist, but it’s hard when the patient goes in there and is presented with a much larger fee than they expected. We’ve been able to offer our patients significantly reduced fees because we’re doing both the surgical and the restorative phase.
CM: Can you discuss the training you received prior to placing your first conventional-diameter implant?
VF: I was looking at offerings by the large implant companies out there, and their classes were either hard to find or didn’t provide the kind of instruction I wanted — a comprehensive course that would teach you all you need to know to place an implant and find that first slam-dunk case. Then I came across Dr. Paresh Patel’s course offered by the Glidewell International Technology Center, and it was exactly what I was looking for.
I came across Dr. Paresh Patel’s course offered by the Glidewell International Technology Center, and it was exactly what I was looking for.
CM: Did the course live up to your expectations?
VF: Yes. The training that Dr. Patel provided was very straightforward and exact. I left with a clear understanding of everything he showed us during the two-day course. It wasn’t just: “Here are these great case photos. Look at my great work, but I’m not going to teach you how to actually do it,” which is what happens at a lot of courses. He broke everything down. When he showed us flap design and reflection, he demonstrated exactly how to do it and which instruments to use. When he talked about pharmacology prior to the appointment, he explained precisely which medicines to use and how to prescribe them. He gave detailed step-by-step instructions on osteotomy preparation and how to correct things if the angulation was off.
He covered everything very comprehensively: picking the right cases, diagnosis and treatment planning, evaluating patients with and without a cone beam, the surgical protocol and armamentarium, the follow-up. I left there feeling really excited to place my first conventional implant, and was confident that I knew exactly what to do when I got back to my office and sat down with my patient.
CM: What type of implants were you exposed to during Dr. Patel’s course?
VF: They were demonstrating everything with the Hahn™ Tapered Implant System (Glidewell Direct; Irvine, Calif.), which is actually one of the reasons I selected that course. When I saw that the implant is supported by the Misch Institute and was engineered by Dr. Jack Hahn, who developed the original tapered implant for Nobel Biocare, I felt really comfortable taking the course.
The implant helped simplify the learning process, and it remains my system of choice. The surgical kit walks you right through what you need to use. Everything’s lined up properly, so it’s very easy to follow. There’s not much to think about once you’ve properly planned out everything. And I really like the implant’s aggressive threads; in addition to providing great primary stability, if your osteotomy isn’t positioned exactly where you want it, you can slightly change the angulation without a problem.
The [Hahn] implant helped simplify the learning process, and it remains my system of choice.
CM: Was your first implant case a regular patient of yours?
VF: My first implant case was a regular patient I had been treating since 2014. She was actually down in Florida when the tooth fractured, and a local doctor did the extraction and grafted the socket. After returning to New Jersey, she visited my office and, because I knew I would be taking the course soon, I told her that we could place the implant for her after she healed. When I did the cone-beam scan, I saw that the ridge was 11 mm wide and thought that she would be a great candidate for my first implant. Even if I placed a 7 mm implant, there was plenty of bone every which way. She is also a very nice and understanding patient who was willing to work with me and have patience as I made my way through my first case, which helped a lot.
CM: Were you nervous before placing your first conventional implant, or were you more comfortable because you’d had experience placing minis?
VF: I wasn’t really nervous. I reviewed the cone beam the night before and went over the protocol to make sure I knew exactly what I’d be doing during the procedure. Dr. Patel, who has always been available to offer a second opinion on a case or answer any follow-up questions I have, was nice enough to look over my cone beam, confirm that the planning was correct, and make sure I didn’t have any unanswered questions.
CM: How did you go about preparing your office and staff for the procedure?
VF: After taking the course, I spent some time creating the protocols for our office. I held a meeting with my staff to go over dental implants, how the procedure would go, and the language we should use when talking to patients about treatment. I got my receptionist up to speed about scheduling implant treatment, calling in the pre-op meds and making sure they’re taken properly, and things like that. She’s also the treatment coordinator for these implant cases. If we’re doing an extraction and graft, she knows that four weeks later we’re going to be taking out the membrane, three and a half months later we’re going to be getting a scan, four months later we’re going to be doing the surgery, and so on. She makes sure everything is on schedule so we’re not falling off with any of the patients.
After taking the course, I spent some time … with my staff to go over dental implants, how the procedure would go, and the language we should use when talking to patients about treatment.
I did a mock setup with my assistant, provided her with an instrument list for the different procedures that we would be doing, and sat down for a mock surgery so she knew what was required for each step of the procedure.
I also spoke with my office manager, who handles the financial aspect, about making sure everyone is aware of the financing. If it’s an extraction and graft, for example, we’ll offer treatment to the patient for $500 down and a $375 monthly payment for eight months, which is how long it takes to complete the implant case. By the time we’re finished, the patient is all paid up and avoids having to shell out the money all at once.
CM: How was the final outcome for that first case? Was the patient happy?
VF: Like many first-time implant patients, she didn’t know what to expect. The word “implant” is scary to a lot of people because it means surgery. Her feedback was very positive, and she didn’t have any discomfort during or after the procedure. She’s been happy throughout the process and was very satisfied with the final restoration. Also, because I had great primary stability with the Hahn implant, I was able to place the healing abutment on the day of surgery, so it was nice for her that I didn’t have to go in to do a second procedure to uncover the implant.
CM: Was presenting and getting the patient to accept treatment a challenge when you first got started with implants?
VF: When my first patient came to the office for consultation, I hadn’t yet taken any courses. I told her that I’d be taking training soon and that I’d be able to place the implant for her and do everything here in my office if she could wait. When I was getting started, I was very upfront with my patients about my experience level, and it was never a problem because the patients trusted and had confidence in me.
After the first four or five implants, things really gained traction and we would just tell patients: “If you want to do an implant, we can do it here for you. We can make sure you’re comfortable, it will be less expensive than referring you out to a specialist, and we can restore it right here in the office.” When patients ask about the cost, I tell them: “When I was referring patients out to specialists for an implant, it was running anywhere from $5,500 to $6,000. In my office, the cost to place and restore an implant is $3,000.
“I can do a root canal; I can do a post and buildup. But will it last you five years? I don’t know. But if we do this implant for you, the literature says there’s a 95 percent success rate after 25 years. Do you want to spend $2,000 to do a root canal, post and a crown, or do you want to spend $3,000 and know that the tooth is not going anywhere?”
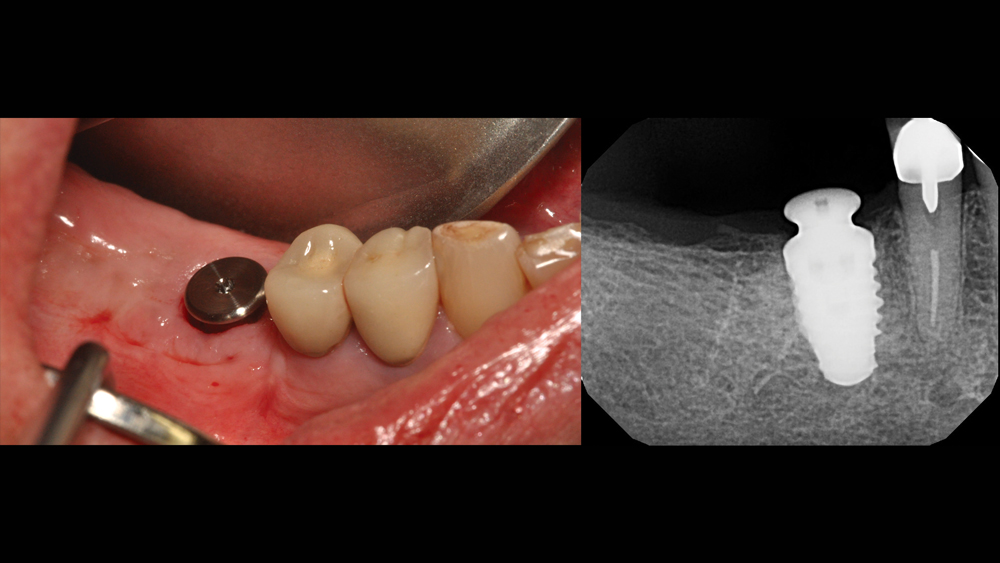
Four months after the extraction and socket preservation procedure, a Hahn Tapered Implant was placed. Because the primary stability of the implant was high, a healing abutment was connected to the implant on the day of surgery.
Of course, I present my patients with all of their options, and I still do root canals all the time. I just try to avoid “herodontics,” where we try to save teeth that won’t last. I think every practitioner has tried at times to salvage severely broken-down teeth because a patient doesn’t want to lose the tooth. Our sympathy for our patients as a practitioner sometimes overcomes our knowledge, and we decide to save a hopeless tooth with root-canal treatment and a post and core. A year later the patient is in the office with a tooth in their hand that we just treated.
My whole goal in this has been to bring the fee for an implant restoration close enough to the alternative to dissuade patients from making a poor medical decision based on cost. When the tooth can’t be saved, we want them to choose the best long-term solution instead of just doing what insurance would cover. People can afford it, and we’re still making very good money on the implant cases we do.
When the tooth can’t be saved, we want them to choose the best long-term solution instead of just doing what insurance would cover.
CM: Did you learn anything from that first experience that’s helped you improve the experience for the patients you’ve treated since?
VF: Although everything seemed a little scary at first when I decided to take that course, after placing that first implant, I learned that this is really simple when you’ve been properly trained, selected the right case, and properly planned everything out. I was doing one case a week for the first month, and I’ve been doing one or two cases a week ever since. If I had known earlier what I know now, I would have started placing implants sooner.
CM: What types of implant cases have you completed surgical procedures for at this point?
VF: I’ve done some multiple-unit cases, some bilateral implants for posterior reconstruction, and an extraction with immediate placement — a procedure I learned during Dr. Patel’s level two course, which I took a month after the first one. The day after I took that course, I happened to receive a call from a college basketball player who had just had one of her front teeth fractured during a game. There was no way to save the tooth, so we extracted it the same day, placed the implant, grafted the gap, temporized it, and got a pretty nice result. I’ve also signed up for the 300-hour AAID MaxiCourse®, so I’m excited to learn even more about implant therapy.

*Following osseointegration of the implant, a BruxZir® Full-Strength Solid Zirconia screw-retained crown was delivered. Thanks to proper training, planning and case selection, this predictable outcome was achieved with relative ease. *
CM: Now that you’re confidently placing implants, how do you decide which cases to refer out for implant surgery?
VF: I’ll usually refer out anything that requires significant bone augmentation. If the ridge isn’t wide enough, there isn’t enough vertical height, we’re close to vital structures or a sinus lift is needed, I’m just not at the level to be doing those things, and we have specialists who are very good at those types of cases. I do perform a fair amount of grafting using Newport Biologics™ Mineralized Cortico/Cancellous Allograft Blend (Glidewell Direct), mostly for extraction socket regeneration and immediate implants.
CM: Would you recommend that other GPs get involved with placing implants?
VF: I think GPs need to be placing implants. With the aging of the baby boomers, there’s a growing need for implants, and there are just not enough people placing them. Also, like we talked about before, I have found that case acceptance is a lot higher when you can treat patients within your own practice rather than referring them out to an oral surgeon. We’re now getting an 80 percent acceptance rate on cases for which we used to get 20 percent.
We’re now getting an 80 percent acceptance rate on cases for which we used to get 20 percent.
CM: How has the incorporation of dental implants affected your practice?
VF: We’ve placed close to 50 implants in under a year, which has grown the revenue for our practice exponentially. It’s also very rewarding to provide patients with a long-lasting restoration without having to worry about them coming back with a broken crown in five years. The ability to offer the patients a great service at a modest price is a morale booster for the practice, and my whole office gets excited every time we’re placing implants.
Learn more about the course and register at glidewellcecenter.com.



