Increasing Treatment Acceptance by Not Being Normal

At the heart of a great dental practice are exceptional clinical skills and the ability to deliver outstanding care. However, clinical skills alone will not build a thriving practice, as 85 percent of the time spent with patients is communication and only 15 percent is clinical application.1 It’s one thing to have the clinical ability to treat a patient, but you may never reach the treatment phase if your communication skills are poor.
Most patients who call your office have already made the decision to choose your practice. It becomes the responsibility of the team to validate that they made the right decision. This is the first opportunity to set the office apart and give patients the right impression of the quality of care and exceptional experience they will receive.
Nobody notices normal.
– Kelly Swanson
Storyteller and Motivational Speaker
Award-winning storyteller and motivational speaker Kelly Swanson said, “Nobody notices normal.” Steer away from the standard conversation describing office policies and regulations and asking patients about their insurance coverage. These conversations should happen after you have impressed the patient with your customer service proficiency. Patients tend to be more compliant with your office standards when they feel they are going to be treated well. Avoid making office rules the focal point of the new patient introduction. Instead of asking standard questions like, “What insurance do you have?” try these:
“What inspired you to call?”
This question will immediately set your office apart from other practices and give the patient an opportunity to tell you what motivated them to seek your care. The question also leads the conversation into describing why your practice is right for them. An appropriate response may be, “Based on what you’re looking for, I can understand why you chose us.” Informing patients how your practice delivers care makes the office instantly distinctive.
It is important to gather important information from the patient to begin establishing records. Some practices launch into questions regarding personal details before establishing rapport or gaining patient permission.
As a courtesy to patients, and to demonstrate your sensitivity when asking them to divulge personal information, ask for their permission. For example:
“May I ask you a few questions?”
This minimizes the perception that you are asking scripted questions to complete a form. By asking permission, you are engaging the patient in the decision-making process. This will lead to a stronger rapport with the dental team and increase the confidence the patient has that the team is an active part of their care, especially when it comes to treatment planning.
“May I tell you a little more about our practice?”
This provides the opportunity to mention unique details about the practice and endorse the doctor. For example, “The doctor has great chairside manners,” or “We will give you all the time you need to help you make the right choices for your care.” These comments help the patient feel comfortable and reinforce the notion that they are in the right place. The dental auxiliary can also endorse the doctor and the excellent standard of care by telling the patient their own story. Why do they work there? What about the office makes them proud? How do they feel as a member of the team? These comments establish trust and act as an endorsement of the practice. Remarks must be authentic and not scripted or contrived. This extra step only takes a few moments but makes a significant difference in increasing patient confidence.
PRESENTING TREATMENT TO PATIENTS
The doctor’s treatment plan should be presented after the initial consultation, the collection of diagnostic information and the clinical examination. Rather than listing what the patient’s needs are, and prior to presenting a written treatment plan, ask the patient this:
“Would you allow me to tell you what I would like to do?”
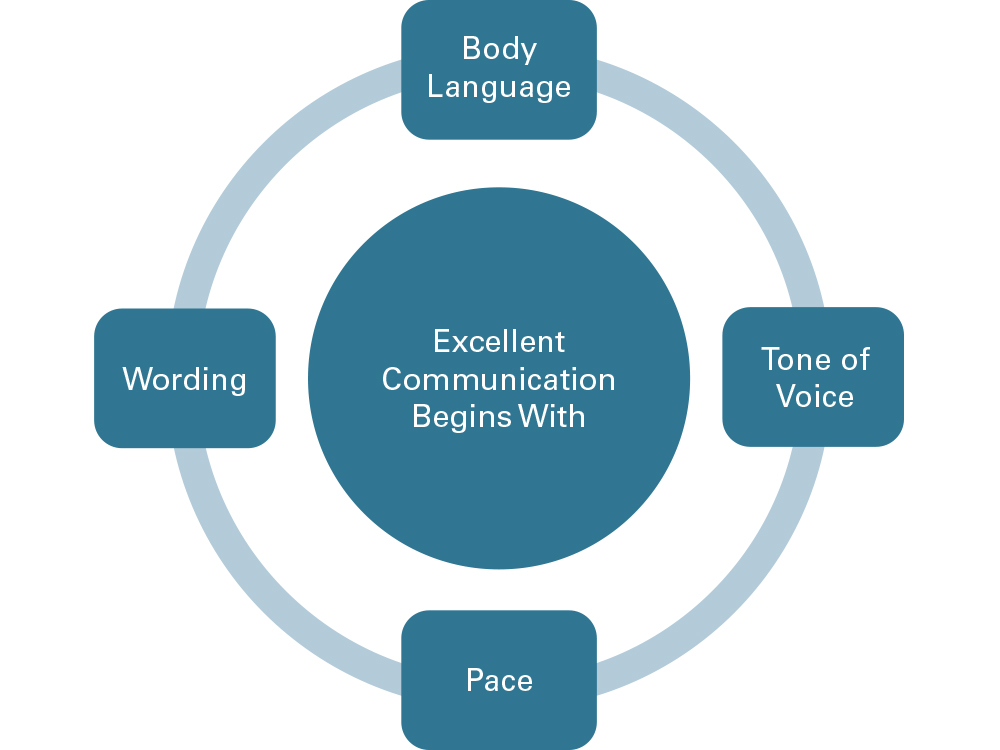
This question provides the opportunity to present the patient with the doctor’s plan for ideal care. The treatment discussion should be done with great sensitivity, incorporating all aspects of excellent communication — body language, tone of voice, pace and wording. This is not to be a rushed conversation. It is important to be an intentional listener and convey total engagement. The best way to indicate engagement visually is to sit eye level with the patient and lean slightly forward.
Avoid giving the patient a list of what they need and dismissing them too soon to discuss financial arrangements. Speak to the patient — not to the paper. The decision to accept treatment is the responsibility of the clinical team, not the financial team. The financial team is there to negotiate terms of payment after the patient and doctor have agreed on the treatment plan.
Pushing people into treatment by telling them what they need is not the winning approach to help patients appreciate and accept the doctor’s treatment plan. Avoid telling the patient what you can do, what you want to do or what they need. Instead, lead with this question: “Would you allow me to tell you what I would like to do if you were my brother, sister or aunt?” The patient never says, “No, don’t tell me.” This is a non-threatening approach to introducing your comprehensive treatment plan.
SUCCESS THROUGH HYGIENE
How much dentistry has been planned but not completed by patients of record? Improving communication skills in the hygiene department will have a dramatic effect on increasing practice productivity. Establishing a way to initiate a conversation with patients about their incomplete treatment plan can boost profitability. It should never be assumed the patient is not interested in, or cannot afford, treatment based on past conversations. If the office stops talking about incomplete treatment based on assumptions, the patient will never place importance on treatment needs that are not met. Hygienists need time to have this conversation with their patients. Here is an example of how this conversation would flow:
“In reviewing your records, I notice there is work the doctor recommended that has yet to be completed. What has prevented you from having this done?”
The patient will probably bring up the following reasons:
- It’s too expensive.
- It’s not bothering me.
- I don’t have time.
Working on communicating with the patients to address these objections will ease the conversation. Here are some examples of how to address these concerns:
“If we can find a way to help this be affordable, what other concerns do you have?”
“Our goal is to help you avoid having any dental discomfort or unplanned dental problems. If you wait until it bothers you, it will require significant treatment and be more costly.”
“If time is a major concern, it would be best to take care of this now, before it becomes a more significant problem that would require more appointments.”
It is also important to remember the reason the patient is coming to their hygiene visit. Be careful that it doesn’t become too social. Sometimes hygienists become so friendly with the patient they forget to talk about dentistry. Excellent communication is a balance of relationship building and clinical conversation.
DISCUSSING FINANCES
Communicating financially with the patient requires confidence, skill and knowledge of the art of negotiation. Patients are not interested in how your financial protocols serve the practice. They are interested in how financial protocols serve them. Written protocols should be established and used as a guideline for financial discussions. Presenting them in writing diminishes the ability to negotiate your preferred payment options. If the office has a financial option that is preferred it should be the first one presented. Wait for the patient to respond whether that option works for them. If it doesn’t, present the next option. If none of the options suit the patient, say:
“Tell me what you had in mind?”
If their preference does not work for your office, attempt to find an affordable solution that will be mutually beneficial. Remember: this is a two-way conversation.
When you begin the financial conversation avoid the statement, “We require …” and replace it with, “Most of our patients prefer to take care of their charges by (preferred method of payment).” Give the patient an opportunity to respond. Working in an atmosphere of financial discomfort is not conducive to patient or practice satisfaction. The team presenting financial options and negotiating payment terms must be thoughtful, professional and comfortable with their skills.
ATTITUDE AND THE BELIEF CYCLE
The belief cycle is a psychological concept that explains how beliefs influence actions, which in turn reinforce or modify those beliefs.2 This cycle consists of four key stages: beliefs, actions, results and reinforcement. Understanding this cycle is crucial for dental professionals when presenting treatment options, as it helps them overcome their preconceptions about treatment acceptance.
1. Beliefs
These are preexisting notions or perceptions that a person holds about a particular subject. These are thoughts or assumptions we hold to be true, whether or not they are based on facts. For example, while visiting dental practices across the country, I often hear doctors and dental teams predetermining patient interest or financial viability for dental treatment. They base their beliefs on patients’ previous remarks or attitudes when treatment has been presented or base it on insurance limitations and restrictions.
2. Actions
Our beliefs generate emotional responses, which lead to specific actions. If we believe something is true, that emotional truth reinforces the belief, even if it’s inaccurate. For example, the employee may believe the patient cannot afford the treatment based on their own feelings. Their feelings will modify their behaviors. For dental teams, these actions can include altering the treatment plan based on the belief that the patient will not choose the most comprehensive care or will choose based on insurance restrictions and can even lead to staff not introducing the doctor’s preferred treatment plan at all.
3. Results
These are outcomes that result from the action taken. In dental care, this can mean the plan is presented in such a way that the patient is dissuaded from choosing the recommended care. The tone of our treatment discussion is less than positive and encouraging, if presented at all. And even if treatment is discussed, remarks such as “This is what we would like to do, but it won’t be covered by insurance” can imply that the care is less significant than the patient’s insurance coverage.
Here’s how the belief cycle plays out in a dental case acceptance scenario:
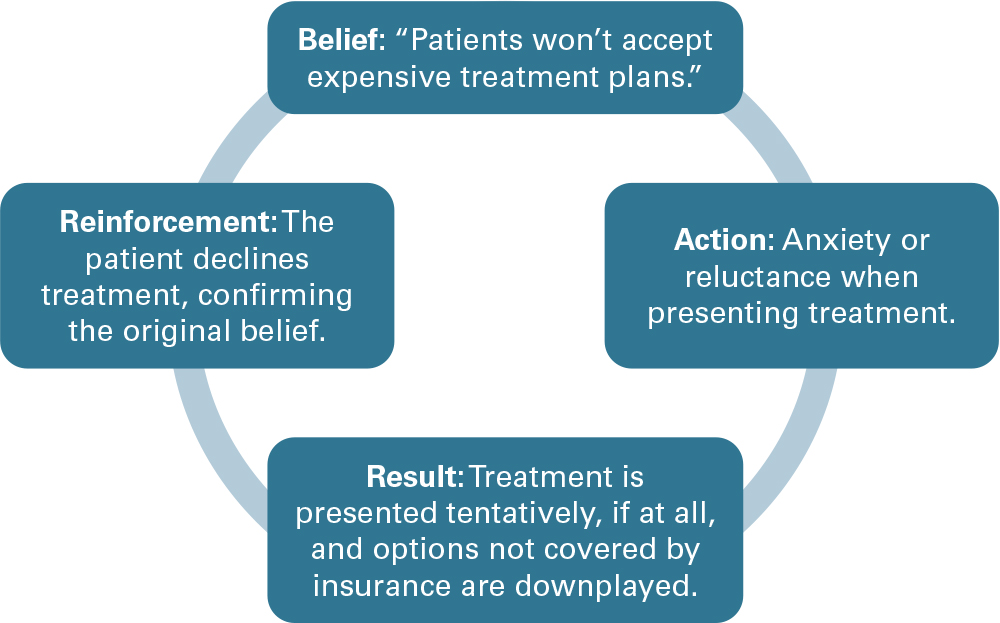
This belief cycle is often played out with patients of record during their hygiene visit. The patient has been in the practice for years and has established a habit of not choosing previously recommended treatment. The hygienist has a “belief” that the patient isn’t interested in moving forward with treatment and stops talking about it or doesn’t call attention to incomplete care.
To break free from the negative loop of the belief cycle, dental professionals must actively challenge preconceived notions. This begins with examining the beliefs that drive actions and questioning whether these beliefs genuinely serve the patient’s best interests or merely reflect assumptions rooted in past experience. By recognizing that every patient is unique, with their own priorities and needs, teams can create a more open and inclusive approach to care. Empowering the dental team with a mindset focused on possibilities rather than limitations transforms interactions.
When professionals enter discussions with optimism and trust in the patient’s ability to make informed decisions, their tone becomes more engaging, their presentation more thorough, and their confidence more evident. It is this shift that lays the foundation for meaningful and impactful communication. Changing our belief changes our attitude and our approach.
By approaching patient care with a proactive mindset, dental teams can begin to foster a culture of empowerment and education. For example, instead of hesitating to discuss treatment plans due to perceived patient disinterest, professionals should view such discussions as opportunities to educate and engage. Patients may hold misconceptions about their oral health or the financial implications of treatment, and it is the team’s responsibility to address these concerns with clarity and empathy.
When professionals enter discussions with optimism and trust in the patient’s ability to make informed decisions, their tone becomes more engaging.
Integrating tools like visual aids and patient-centered language can bridge gaps in understanding. When patients see tangible representations of their oral health or hear how a proposed treatment aligns with their long-term wellbeing, they are more likely to perceive its value. Shifting focus from assumptions to active dialogue invites collaboration, ensuring that patients feel empowered to make decisions that resonate with their personal needs and aspirations.
Ultimately, it is about creating an environment where patients feel heard, respected and supported. By cultivating trust and focusing on shared goals, dental teams can redefine these moments from transactional exchanges to meaningful experiences.
CONCLUSION
Mastering the art of communication is critical for every member of the team. Even a subtle shift in approach can change the conversation. Dental professionals who excel in communication foster trust, alleviate patient anxiety, and contribute to the success of the practice. By asking the right questions, actively listening, and expressing empathy, the team can improve patient outcomes and increase practice productivity.
References
-
Waylen A. The importance of communication in dentistry. Dental Update. 2017 Sep.;44(8):774–780.
-
Bandura A. Social foundations of thought and action: A social cognitive theory. Health Psychol. 1986.