Laboratories Want Better Impressions

If you were to spend a few hours in a typical U.S. dental laboratory looking at impressions for crowns and fixed prostheses, you would be dismayed to find that only a few of the impressions could be considered adequate. Discussions with many laboratory owners and with national laboratory organizations have led me to the conclusion that we dentists need to examine the reasons why many of our impressions are inadequate, change our techniques and raise our quality expectations for impressions.
There are many reasons why fixed prosthodontic impressions are inadequate. This article discusses the potential methods to obtain better impressions in the hope that those needing improvement in impression making will change their techniques for the better.
IMPRESSION MATERIALS AND IMPRESSION TRAYS
Vinyl polysiloxane and polyether impression materials are among the best of all dental materials. These materials, used with good trays, provide nearly perfect accuracy. With few exceptions, we cannot criticize impression materials. All of the major impression material companies and most of the smaller companies have excellent, accurate and stable materials. The problem does not lie with impression materials; it lies with us.
Most dentists use the double-arch quadrant impression technique for one or two units. Popular and proven double-arch trays are the Sideless Posterior Triple Tray® (Premier Products; Plymouth Meeting, Pa.) and the QUAD-TRAY® Xtreme™ (Clinician’s Choice; New Milford, Conn.). Because the double-arch trays are not rigid, heavy-body materials are desirable for use in the tray. I prefer medium-body impression material for the injection procedure. The medium viscosity allows an air stream to be blown on the injected material and eliminates bubbles at the marginal areas. Light-viscosity material easily blows off the tooth preparation.
Some laboratory technicians and dentists have difficulty working with the double-arch tray concept. However, with experience, the technique soon becomes easy to understand and relatively simple to use. Clinical success should be expected most of the time if both dentists and laboratories use the concept adequately.
The double-arch technique is excellent if the clinician has accomplished occlusal equilibration before making tooth preparations, and if the laboratory technician fabricating the restorations pours the impression correctly.
However, full-arch trays are another matter. Laboratories and dental manufacturers will state that most full-arch impressions for crowns and fixed prostheses are made in stock trays and a much smaller percentage are made in custom trays. Most full-arch stock impression trays are flexible and can be distorted easily. I suggest using custom-made, light-cured tray material, of which two popular examples are Triad® Custom Tray Material or Triad TruTray™ Custom Tray Material (DENTSPLY; Milford, Del.). Custom light-cured trays are easily made, rigid and stable, and the dentist can modify them by adding small amounts of material and light curing it with a clinical curing light. These light-cured trays cost only a few dollars each, including the dental assistant’s pay for the time spent making the tray. The need for vinyl polysiloxane or polyether impression material is reduced by about one-half when one uses a custom tray rather than a stock tray, preventing waste and saving money.
In my opinion, the long-proven “double-cord” technique for impressions of crown and fixed-prosthesis tooth preparations is the most reliable method of making adequate impressions.
PREOPERATIVE PERIODONTAL TREATMENT
It has been my observation from examining working casts in dental laboratories that many teeth are prepared for crowns and fixed prostheses without undergoing preoperative periodontal treatment. I have even observed on working casts the presence of obvious calculus on teeth that were prepared for prostheses. Periodontal tissues need to be treated long enough before tooth preparations are planned so that the gingiva can tolerate the minimal trauma caused by tooth preparation without excessive bleeding. I suggest that soft tissues be allowed at least two to three weeks of healing after scaling and curettage, and preferably a few months of healing after conventional periodontal surgery, before teeth are prepared for crowns and fixed prostheses.
PREOPERATIVE CHLORHEXIDINE GLUCONATE MOUTHRINSE
Patients planning to receive multiple crowns or fixed prostheses should use 0.12% chlorhexidine mouthrinse at least once, and preferably twice, per day for two weeks before teeth are prepared. The result will be evident to practitioners. The soft tissues will be pink and firm at the tooth preparation appointment, and bleeding will be minimal or nonexistent. Although the chlorhexidine causes slight superficial tooth staining, it can be removed easily. I suggest continuing use of the chlorhexidine rinse during the provisional restoration period, as well as for two weeks after cementation. An occlusal adjustment a few weeks after the restorations are seated usually is necessary for multiple restorations, and chlorhexidine stains can be removed at that time.
PROTECTING GINGIVAL TISSUES DURING TOOTH PREPARATIONS
Some practitioners cut tooth preparations with little or no protection of the gingival tissues. The result is removal of the gingival epithelium by the rotary cutting instrument and excessive bleeding during impressions. I suggest placing a retraction cord after the initial supragingival tooth preparation and before making the final gingival margin preparation. The cord pushes the gingiva apically, and the gingival margins can be finished without cutting the gingiva. Wherever the margins need to be moved even more apically, a metal gingival protection instrument such as the Zekrya™ Gingival Protector (Zenith Dental; Englewood, N.J.) can be used on the facial aspect of the tooth to further protect the gingival as the tooth preparation margins are lowered apically.
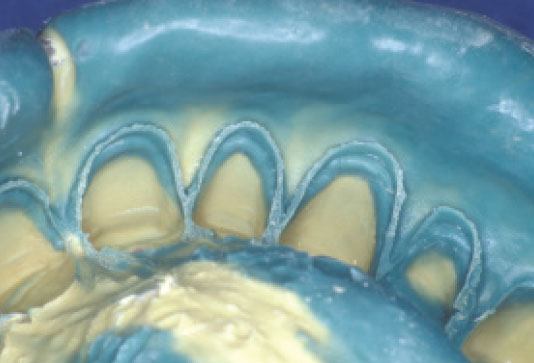
TISSUE MANAGEMENT USING TWO CORDS
It has been my observation in continuing education courses that the most commonly used tissue management procedure is the “double-cord” technique. When using this technique, the clinician places one cord to fill about one-half of the gingival sulcus after supragingival tooth preparation, and before performing final tooth preparation procedures. He or she places a second cord after completing the final tooth preparation and just before making impressions, and then removes it immediately before the impression material is placed. In my opinion, the long-proven “double-cord” technique for impressions of crown and fixed-prosthesis tooth preparations is the most reliable method of making adequate impressions. However, there are several other procedures that can be as acceptable when done properly.
Iron-containing styptics are the agents most commonly placed on cords to reduce or eliminate soft tissue bleeding while impressions are taken. Although they stain and are bitter-tasting, these ferrous and ferric sulfate liquids and gels placed on cords or in the gingival sulcus provide excellent gingival hemostasis. However, when used before placement of translucent indirect restorations (such as veneers), an objectionable gray stain that shows through the restoration often appears postoperatively. When translucent restorations are planned, materials containing aluminum chloride or other nonstaining ingredients are preferable.
When soft tissue begins to bleed slightly at the time of impressions, I suggest injecting a few drops of lidocaine containing 1:50,000 epinephrine a few millimeters from the bleeding site, using a 30-gauge needle. Slight bleeding will stop almost immediately, but it will start again about two minutes later, so the clinician must make the impression immediately after injecting the solution.
TISSUE MANAGEMENT USING ONE CORD
The one-cord tissue management technique, familiar to all dentists, is appropriate only when the gingival tissues are firm and pink, there appears to be little potential for bleeding, and the gingival margins have been placed supragingivally or only slightly subgingivally. Most dentists agree that the one-cord procedure is less predictable than the two-cord technique.
GINGIVAL MANAGEMENT USING ELECTROSURGERY OR LASER
When used properly, either electrosurgery or laser tissue management can control gingival hemorrhage extremely well, but in many cases, the eventual location of the healed gingival tissues cannot be predicted. I use these tissue management techniques when bleeding has not been controlled well with the two-cord procedure.
Additionally, from time to time after healing, gingival tissue is found to be at an improper height at the time of tooth preparation. In such cases, laser or electrosurgery can be used with success to remove the soft tissue at the tooth preparation appointment.
Some practitioners use these devices as their sole tissue management technique. Certainly, they can provide successful tissue management and excellent impressions, but experience is needed to be able to accurately predict the amount of gingival shrinkage that will be present after soft-tissue healing.
STYPTIC IN FOAM, CLAY OR OTHER MEDIA
In recent years, materials have been developed for soft-tissue management that contain high levels of styptic chemicals, usually aluminum chloride. The successful use of these materials usually depends on the placement of pressure with material similar to a cotton roll on the styptic-containing medium that has been placed on the tooth preparations.
When used properly, the techniques perform well for a few tooth preparations. In my opinion, when impressions are being made for multiple tooth preparations, other techniques are more predictable. These materials must be used exactly according to the manufacturer’s instructions for the impressions to be adequate.
SUPRAGINGIVAL MARGINS
Although leaving tooth preparation margins in a supragingival location is not possible in many situations because of esthetic reasons, dentists should consider this approach in nonvisible areas for patients who do not have high caries activity. Supragingival margins on the lingual surfaces of crowns do not stimulate gingival irritation and are not objectionable esthetically. Often, ceramic veneers can be placed with margins in a slightly supragingival location. Even though the margins are supragingival, their thin translucent nature usually makes the veneers blend with the tooth surface without objectionable display of margins.
SUMMARY
Technicians generally agree that impressions for crowns and fixed prostheses could be better. There are numerous clinical procedures that can assist dentists in making better impressions. Some of these procedures are performing adequate periodontal therapy before starting fixed prosthodontic procedures; using preoperative chlorhexidine mouthrinses; protecting gingival during tooth preparations; using a proper cord placement technique, preferably a two-cord procedure; judiciously using electrosurgery or laser for tissue management; and leaving some margins supragingival. Practitioners are advised to evaluate their impressions carefully and make changes in technique if the impressions could be better.
Dr. Gordon Christensen is the director, Practical Clinical Courses, and cofounder and senior consultant, CR Foundation, Provo, Utah. He is also the dean, Scottsdale Center for Dentistry, Scottsdale, Ariz. Contact Dr. Christensen through CRA Foundation, 3707 N. Canyon Road, Suite 3D, Provo, UT 84604.
The views expressed are those of the author and do not necessarily reflect the opinions or official policies of the American Dental Association.
Christensen GJ. Laboratories want better impressions. J Am Dent Assoc. 2007;138(4):527-9. Copyright ©2007 American Dental Association. All rights reserved. Reprinted by permission. Please note: All photos were added by Glidewell Laboratories, and did not appear in the original JADA article. The American Dental Association makes no representation and accepts no responsibility for the accuracy, timeliness or comprehensiveness of the photos.