12 Alternatives to the Traditional Inferior Alveolar Nerve Block

Abstract
In the case of the difficult-to-anesthetize patient, the inferior alveolar nerve can be particularly challenging. In those patients, other approaches may be necessary to achieve profound anesthesia. This article presents techniques that may be utilized in those efforts. The clinician can change his target slightly, or increase the dosage of anesthetic. Accessory innervation by lingual and mylohyoid nerves sometimes needs to be addressed.
Some standard alternative approaches are Gow-Gates and Vazirani-Akinosi injections. Intraosseous and intraligamentary injections should be considered. For lower anteriors, infiltration and incisive nerve blocks can be effective. Slight changes in armamentarium, such as increasing the needle gauge, can be helpful.
Twelve approaches that can be used instead of, or as an adjunct to, the traditional Halstead injection are described.
Occasionally in dental practice, a patient will present for whom it is difficult to achieve profound anesthesia with the standard inferior alveolar nerve block. In those patients, other approaches to blocking this nerve may be necessary. This article describes 12 techniques for those efforts.
In the traditional (Halstead) technique for the inferior alveolar nerve block, the operator approaches the injection site with the barrel of the syringe over the contralateral second premolar. The needle is placed just lateral to the pterygo-mandibular raphe, approximately halfway up its length. The operator inserts the needle about three-quarters of the length of a long needle, or until bone is touched (Fig. 1). At this point the operator will aspirate, then inject almost a full cartridge of local anesthetic solution. The presence of the lingula, just anterior to the mandibular foramen, makes it advisable to approach the foramen from the contralateral side.
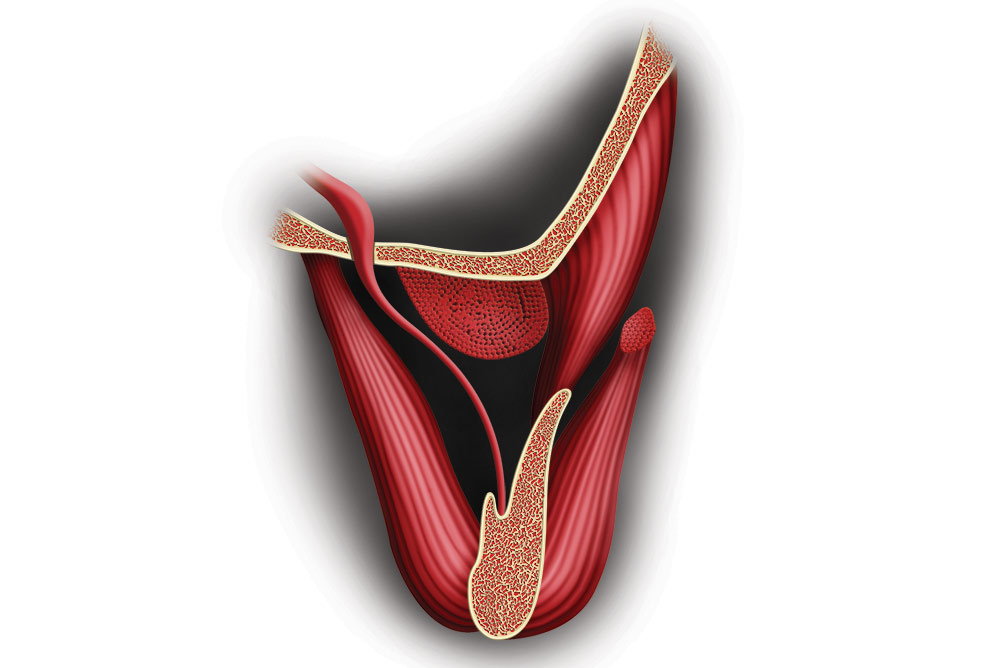
- Inject higher and deeper. The operator should bear in mind the shape of the pterygomandibular space (Fig. 2). Viewed from the operator’s perspective, the space is triangular in shape, with its base (the lateral pterygoid muscle) superior, and its apex (the attachment of the medial pterygoid muscle to the angle of the mandible) inferior. One should also remember the position of the inferior alveolar nerve as it runs down the lateral side of the medial pterygoid muscle and enters the mandibular foramen: It approaches the mandible superiorly and posteriorly. If we can contact the nerve anywhere along its length with anesthetic, it will interrupt transmission on the nerve and effect profound anesthesia.
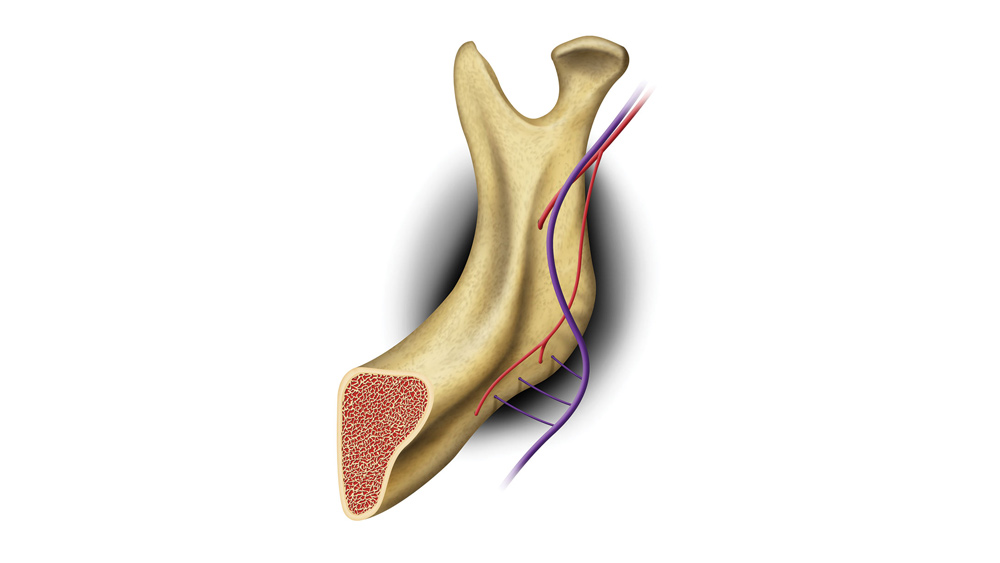
Therefore, if a second attempt is necessary, most operators will aim their needle higher and deeper. One must also consider the fact that in some cases, nerves enter smaller canals in addition to the mandibular canal, on the medial side of the ramus of the mandible. Most of these canals are located in a superior or superior/posterior position relative to the mandibular foramen (Fig. 3).1
Considering these facts, one would be advised to err on the side of being slightly higher and deeper than the site of the mandibular foramen. This leads to the popular rule of thumb for the inferior alveolar nerve block: If your first attempt fails, make your second attempt higher and deeper. Both for the sake of the inferior alveolar nerve itself, and for the sake of the alternative canals like those in Figure 3, this is good advice.
- Increase the anesthetic dose in the difficult-to-anesthetize patient. The healthy patient can tolerate several cartridges of anesthetic without encountering problems. Because the potential volume of the pterygomandibular space is about 5 ml, that amount of anesthetic will come close to filling the entire space. As a practical matter, it is impossible to do so, owing to the immediate dispersion of the solution into other tissue spaces and resorption of solution into the myriad blood vessels. However, injecting two cartridges of solution initially in rapid succession has proven of some benefit in some difficult-to-anesthetize patients.
The Council on Dental Therapeutics of the American Dental Association recommends a maximum dose of lidocaine, with or without a vasoconstrictor, of 2 mg/lb or 4.4 mg/kg.2 Therefore, two cartridges in rapid succession is well within acceptable limits.
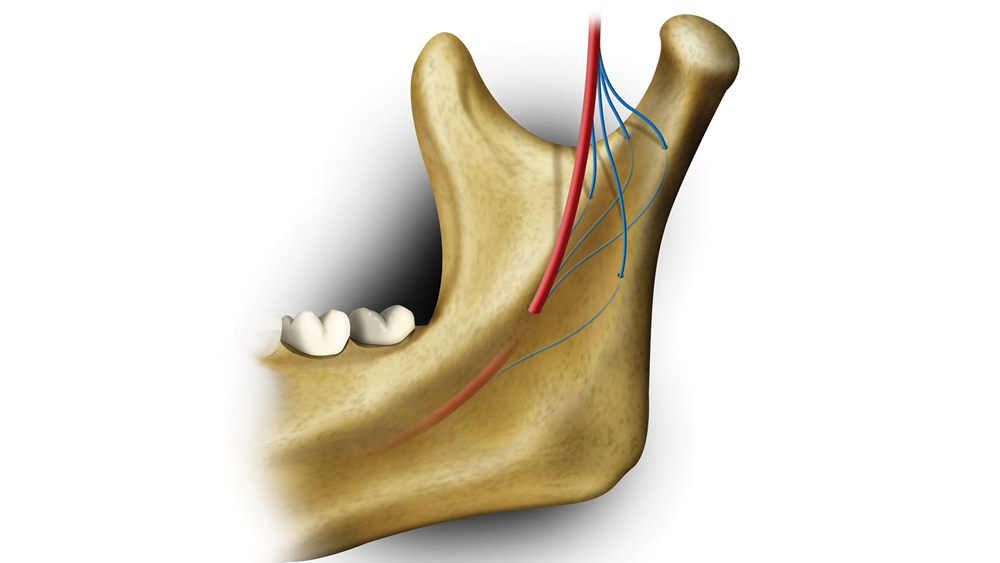
- Inject parallel to the ramus, at the depth of 18 mm. The mandibular foramen is usually found at or slightly below the level of the deepest concavity of the coronoid notch. Therefore, an injection at the level of the deepest concavity, as palpated with the operator’s thumb, will, with the average patient, place the anesthetic very close to the foramen. The usual approach is the Halstead method, described above, but an alternative approach to the same spot is as follows: Insert the needle close to, and parallel to, the medial surface of the ramus instead of approaching from the contralateral side. Three problems may arise in the mind of the operator with the parallel approach. These include how to avoid the temporal crest (Fig. 4), how to compensate for the flare of the ramus of the mandible (Fig. 5), and how deep the needle should be inserted before injecting.
An examination of a mandible will demonstrate the internal oblique ridge of the ramus, passing diagonally down toward the lingual aspect of the third molar (Fig. 3). This ridge must be avoided by penetrating the mucosa 10 mm medial to the coronoid notch.
The careful operator can determine the flare of the ramus (Fig. 4) by placing the thumb in the coronoid notch and the index finger on the posterior surface of the ramus. In this way, one can feel the front and back of the ramus and determine its flare. The needle penetrates the mucosa 10 mm medial to the coronoid notch (to avoid the temporal crest), and is inserted as if aiming for the operator’s index finger. The average depth of the penetration should be 18 mm. Because the conventional 25-gauge long needle is 34 to 38 mm long, and the conventional 27-gauge long needle is 36 mm long,3 one should insert the needle approximately half the length of a long needle, then aspirate and inject.
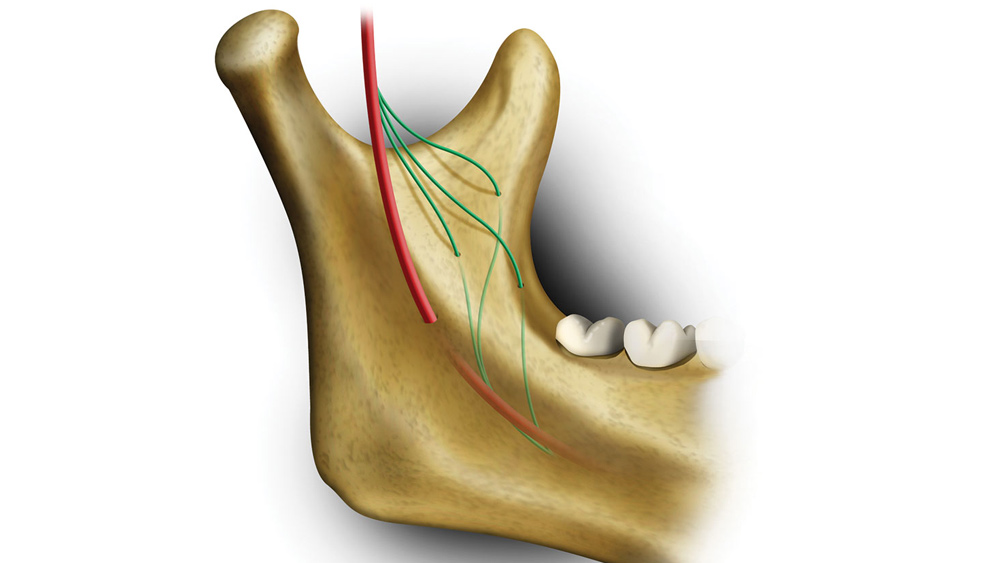
- Anesthetize the mylohyoid/lingual nerves. Close examination of the dried skull will reveal several distinct foramina on the lingual side of the body of most mandibles. These foramina can allow branches of the mylohyoid and lingual nerves to penetrate the bone, bringing sensory innervation to the pulps of some mandibular teeth (Fig. 6). Anesthetizing these branches can be a simple matter of injecting just under the mucosa, just lingual to the body of the mandible, in the area of the tooth to be anesthetized. Care should be taken to make the site of mucosal penetration close to the mandible, to avoid such structures as the lingual nerve and Wharton’s duct, which lie more medial (Fig. 7).
In most cases, a successful inferior alveolar nerve block will anesthetize the mylohyoid and lingual nerves as well, because these nerves pass in close to the mandibular foramen. Presumably, even if these two nerves give off branches to the lingual side of the body of the mandible, these nerves will have been anesthetized at the mandibular foramen, proximal to the branching, and no problems will arise. However, there are some cases in which the lingual and mylohyoid nerves branch from the mandibular nerve at some distance proximal to the mandibular foramen, and do not pass close to the foramen. Fibers from these unanesthetized lingual and mylohyoid nerves might enter the lingual side of the body of the mandible and bring pulpal innervation to the lower teeth. In these cases, anesthetizing as described above should solve the problem.
The transverse cervical nerve, a branch of the cervical plexus of nerves, carries sensory fibers and sends branches very close to the inferior border of the mandible. Considering the tiny foramina near the inferior border of the body of the mandible, some clinicians have implicated branches of the transverse cervical nerve in bringing sensory pulpal innervation to the mandibular teeth.4 This proposal has been largely disputed; in any case, an injection like the one used to combat mylohyoid and lingual nerve involvement should anesthetize fibers from the transverse cervical nerve as well.
- Anesthetize the retromolar pad. Accessory innervation is possible by anomalous branches of the inferior alveolar nerve entering the ramus in the retromolar pad area, usually from a site slightly buccal to the crowns of the molar teeth (Fig. 8). These can be readily anesthetized with an injection in the retromolar area, similar to the long buccal nerve block (Fig. 9).
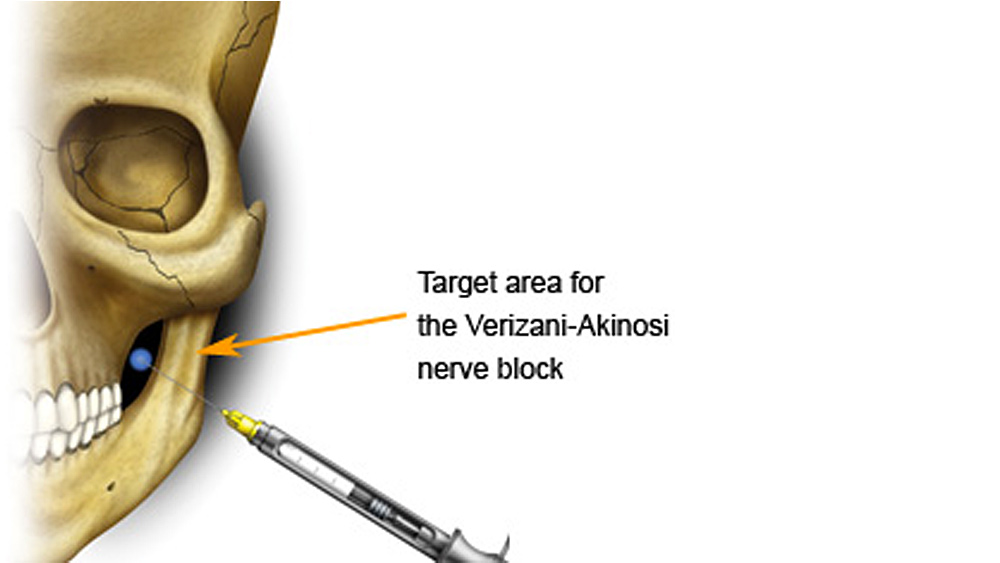
- Utilize the Gow-Gates or Vazirani-Akinosi technique. The Gow-Gates technique5 has a very high success rate in experienced hands, and eliminates most of the problems of accessory innervation described above, because it approaches the mandibular nerve very high in the pterygomandibular space, proximal to the place where mandibular nerve branches into mylohyoid, lingual and inferior alveolar nerves. Many clinicians who are accustomed to the traditional (Halstead) injection are uncomfortable with using extra-oral landmarks for an intraoral injection, but once these psychological barriers are conquered, the Gow-Gates can be very effective. Dr. Stanley Malamed writes that Gow-Gates can be effective 99% of the time in experienced hands (Figs. 10, 11).3
The Vazirani-Akinosi block6 requires lining up the syringe parallel with the occlusal table of the maxillary teeth at the height of the muco-gingival junction of the upper teeth. The target for this injection is below that of the Gow-Gates injection, but above that of the Halstead injection. This injection has the added advantage of being able to be performed with the patient’s mouth closed (Figs. 12, 13).
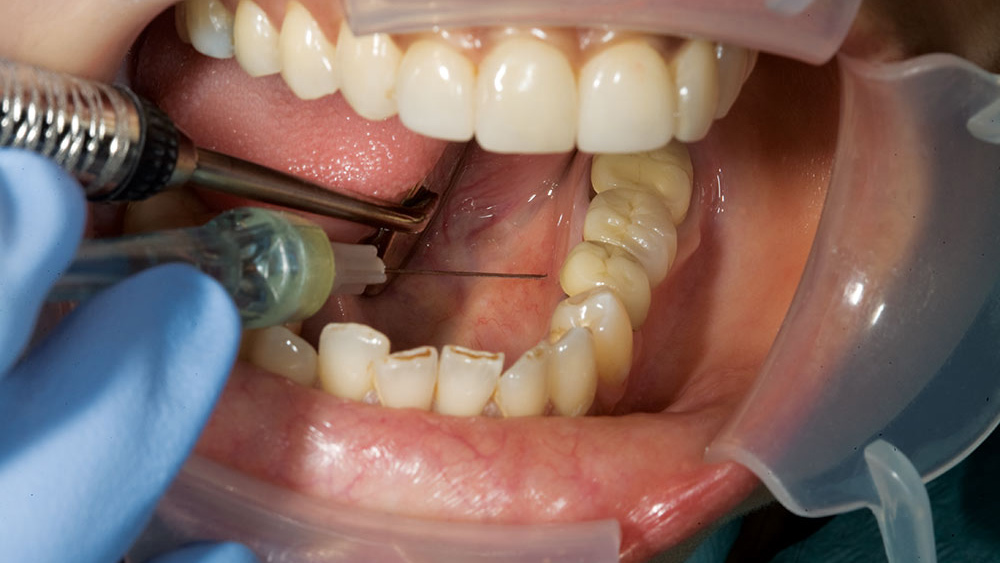
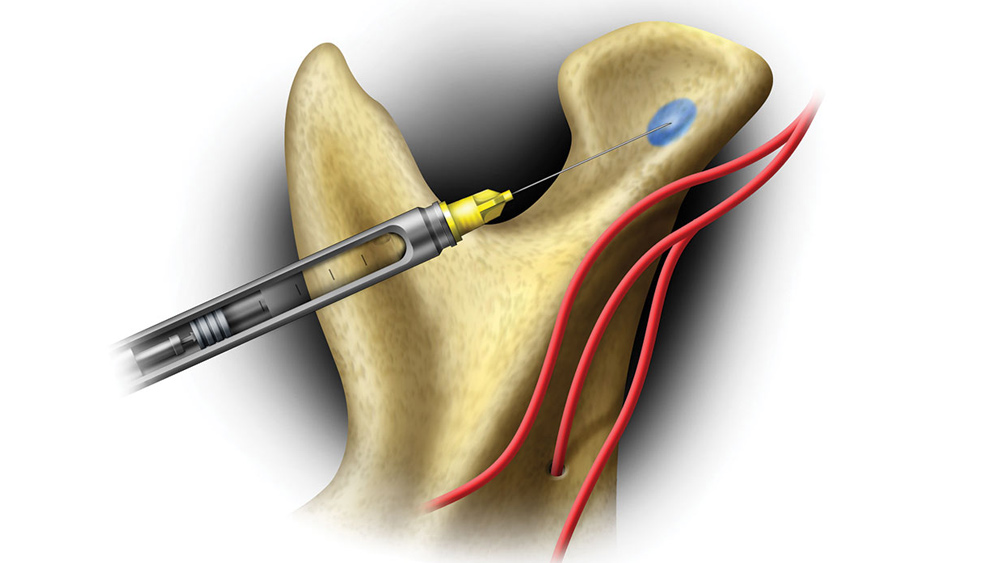
- The intraosseous injection. Intraosseous injections7 are often used for anesthesia of individual teeth when other methods have proven ineffective. Through the use of special kits, this injection places anesthetic in the cancellous bone of the alveolar ridge. Soft tissue infiltration anesthesia at the site is necessary before penetrating the bone.
In most cases, intraosseous anesthesia produces immediate profound anesthesia of the tooth. This profound anesthesia can be fleeting, perhaps as short in duration as 15 minutes, because of rapid diffusion of the anesthetic, and rapid absorption by the circulatory system. Vasoconstrictors do not markedly prolong anesthesia by this technique and can lead to palpitations.8
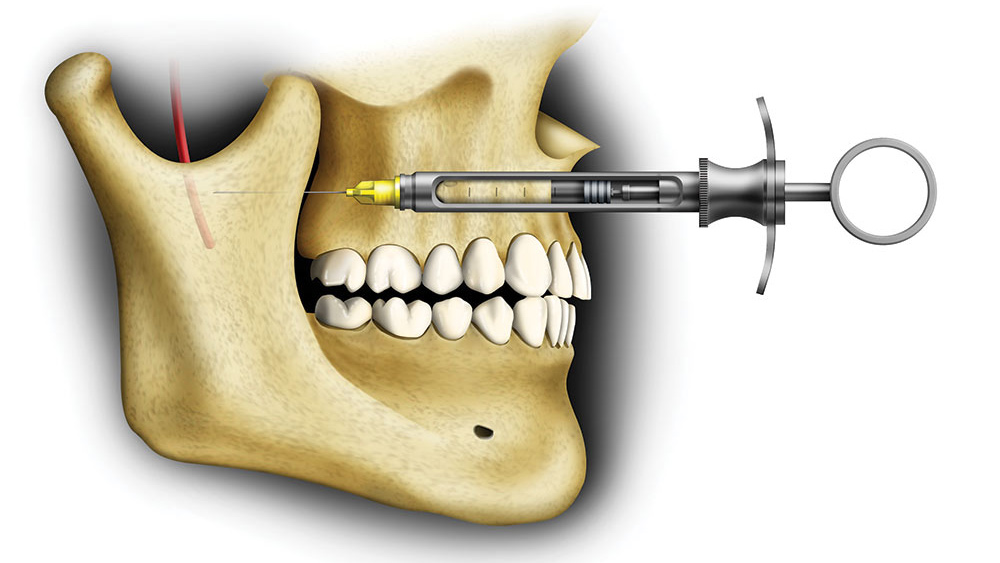
- Make the intraligamentary injection. The intraligamentary injection (variously called intraperiodontal, periodontal ligament, PDL injection)9 requires special armamentaria as well. Through the use of a syringe made specifically for this injection, anesthetic is placed into the periodontal ligament for about 5 mm on the mesial and the same distance on the distal of the tooth. A small amount of anesthetic (0.25 ml) is injected very slowly to minimize discomfort.8
- Use the incisive nerve block. The judicious use of the incisive nerve block can effect profound pulpal anesthesia from the midline as far back as the mandibular second premolar. The injection is relatively painless, and the landmarks are reliable and consistent. The target, the mental foramen, is located either buccal to the apex of the second premolar, or buccal to a spot between the apices of the first and second premolars. Often, the foramen can be palpated before giving the injection. Injecting into the foramen will give pulpal anesthesia to the midline of the mandible.
The operator can increase the effectiveness of the injection by digitally pushing the anesthetic into the hole after injecting. After injecting one-half to three-quarters of a cartridge, there will be a “bubble” of mucosa at the injection site. The operator should slowly and gently “mash” the solution into the mental foramen, until the “bubble” is no longer there, which usually takes about 30 seconds. This will greatly enhance pulpal anesthesia in the area.
Many practitioners continue to refer to the incisive nerve block as the “mental block,” perhaps because the target is the mental foramen. The mental nerve is the branch of the inferior alveolar nerve that exits the mental foramen and provides soft tissue anesthesia only. If one is anesthetizing for pulpal anesthesia, one must get anesthetic solution into the foramen, and in contact with inferior alveolar and incisive nerves. The procedure is correctly called the incisive nerve block.
- Use a 25-gauge needle. Larger-gauge needles have some distinct advantages. There is less deflection in the tissues with the larger gauge, leading to greater accuracy in hitting the target. Intravascular injections are less frequent, because positive aspirations are more clearly seen by the operator.3 With fewer intravascular injections, the solution stays in the immediate area of the injection and is more accessible to the nerve. Malamed3 reports that injections with larger-gauge needles are as comfortable as those with smaller-gauge needles.
- Infiltrate lower anteriors. Although the operator will find it futile to infiltrate the mandible in most areas for pulpal anesthesia of the lower teeth, the lower incisors can be quite readily accessed in this way. A small amount (1/4 cartridge) of anesthetic injected just submucosally, buccally at the level of the apex of the teeth will diffuse through the cortical plate of bone, which is quite thin in that area in most patients (Fig. 14). Infiltration injections can be placed lingually as well, where the thickness of bone is even less in most patients. A very small amount of solution (1/4 cartridge) is sufficient (Fig. 15).
- Try articaine. Articaine, because it diffuses through tissues very well, has the potential to diffuse through the pterygomandibular space and to reach the target nerves well. In addition, a great deal of consistent anecdotal evidence credits Septocaine® (Septodont; New Castle, Del.) (articaine) with the ability to infiltrate mandibular teeth for pulpal anesthesia. These injections are made buccally and lingually to the target tooth, similar to the injection made to anesthetize the lingual and long buccal nerves. Articaine has been associated with an increased incidence of paresthesia of the tongue and lip following anesthesia of the mandibular arch.10
Conclusion
Twelve suggestions are given for treating patients who experience pain with treatment despite the conventional (Halstead) injection. Depending on the preference of the operator, one or more of these alternative approaches may be effective, even with the difficult-to-anesthetize patient.
Dr. William Forbes is course director at University of Detroit Mercy School of Dentistry and adjunct professor of human anatomy at Wayne State University School of Medicine. To contact Dr. Forbes, email forbeswc@udmercy.edu or call 313-494-6643.
References
- ^Lang J. Clinical anatomy of the masticatory apparatus and peripharyngeal spaces. New York: Thieme Medical Publishers; 1995. p. 32.
- ^Council on Dental Therapeutics of the American Dental Association: accepted dental therapeutics. 40th ed. Chicago: American Dental Association; 1984.
- ^Malamed SF. Handbook of local anesthesia. 4th ed. St Louis: Mosby; 1997. p. 86, 203.
- ^J Am Dent Assoc. 1992;123(3):69-73; Br Dent J. 1976;140:237-9.
- ^Gow-Gates GAE. Mandibular conduction anesthesia: a new technique using extraoral landmarks. Oral Surg. 1973 Sep;36(3):321-8.
- ^Vazirani SJ. Closed mouth mandibular nerve block: A new technique. Dent Dig. 1960;66:10-3.
- ^Kleber CH. Intraosseous anesthesia: Implications, instrumentation and techniques. J Am Dent Assoc. 2003 Apr;134(4):487-91.
- ^Jastak JT, Yagiela JA. Regional anesthesia of the oral cavity. St. Louis: Mosby; 1981. p. 165-6.
- ^Walton RE, Abbott BJ. Periodontal ligament injection: a clinical evaluation. J Am Dent Assoc. 1981 Oct;103(4):571-5.
- ^Haas DA, Lennon D. A 21 year retrospective study of reports of paresthesia following local anesthetic administration. J Can Dent Assoc. 1995 Apr;61(4):319-20, 323-6, 329-30.