Implant Surgery: When Should You Use a Flapless Technique?

Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Implant placement is becoming increasingly routine in the general practice, but with it comes a range of decisions that must be made as we evaluate the patient in advance of surgical intervention. When treatment planning a case, we must assess the available bone and quality of the soft tissue, and plan a restorative-driven surgical procedure. A key consideration involves determining which surgical technique to use to access the implant site.
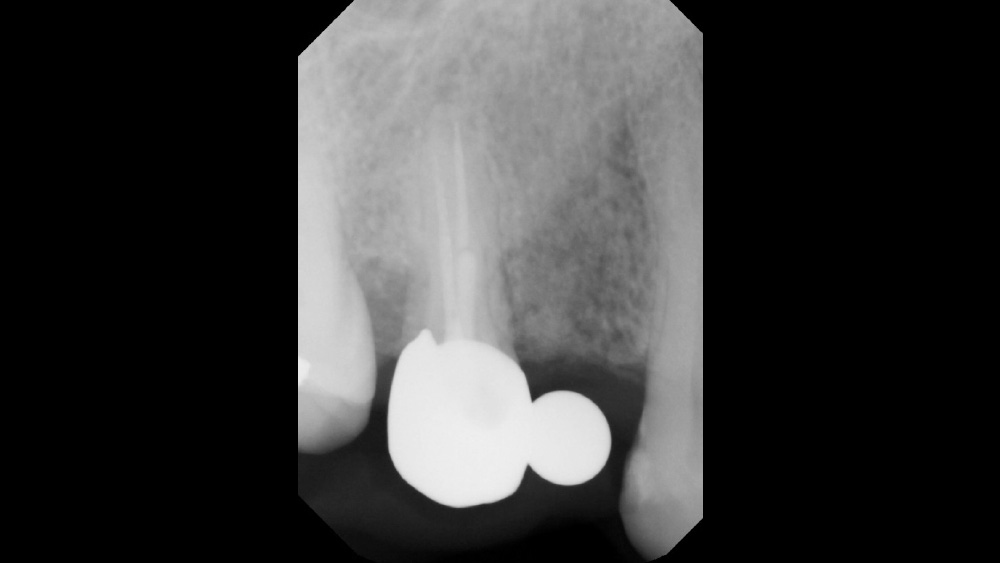
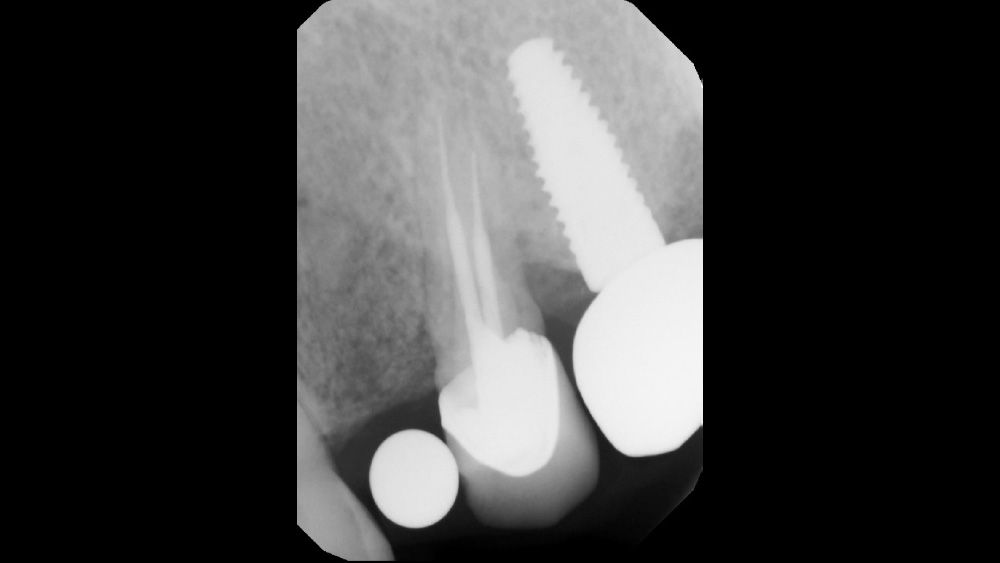
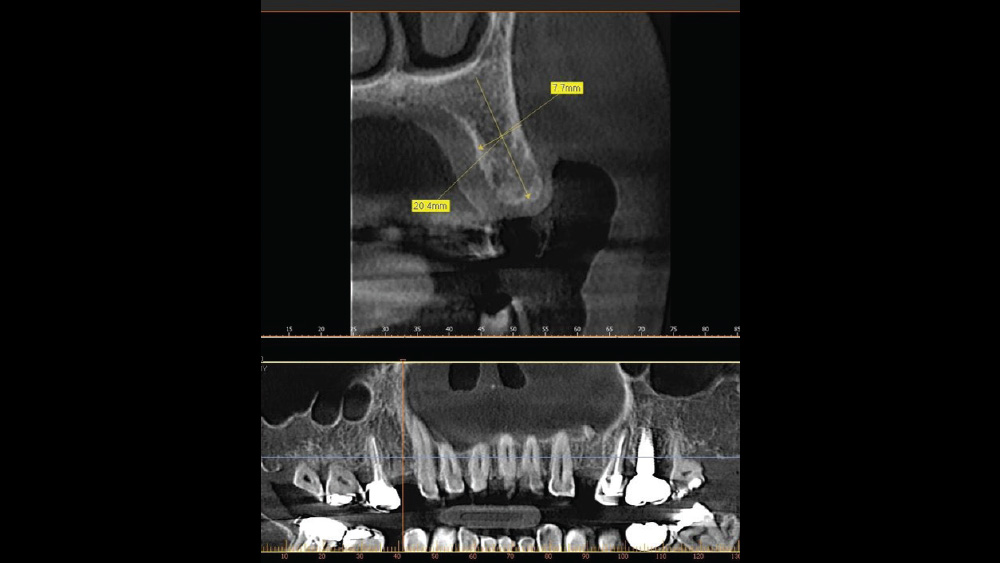
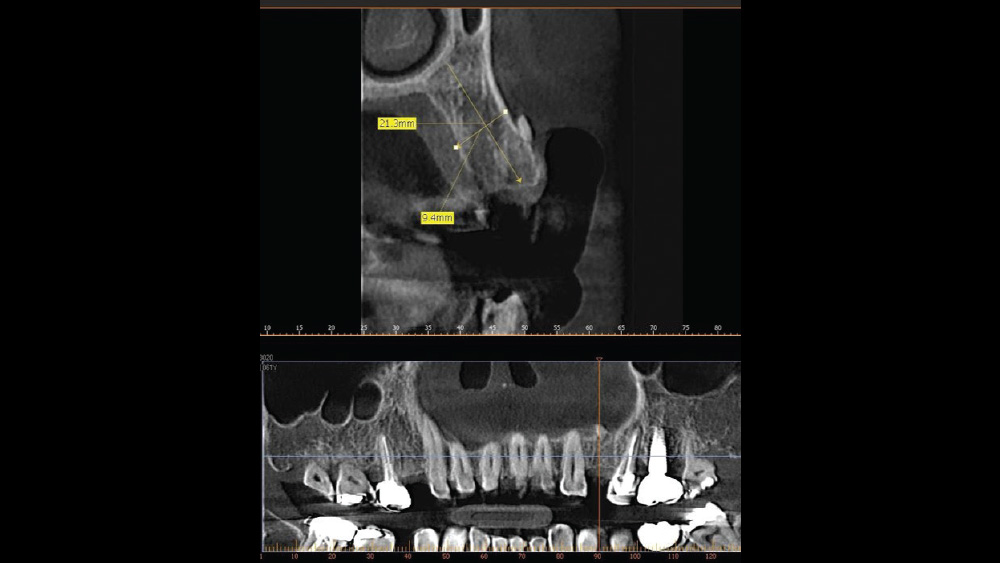
After gaining a clear understanding of the available hard and soft tissue through intraoral evaluation, radiography and — when possible — CBCT scanning, the clinician can determine whether flap reflection or a flapless surgical procedure is ideal for the individual patient. Both of these surgical techniques offer advantages, and the approach should be determined based on the amount of attached tissue present at the implant site, as well as the volume of bone.
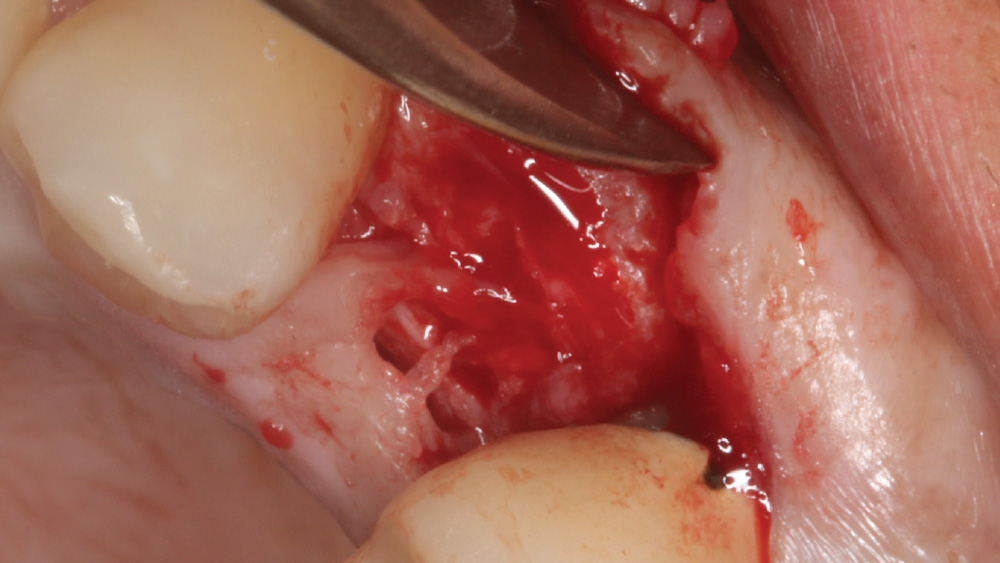
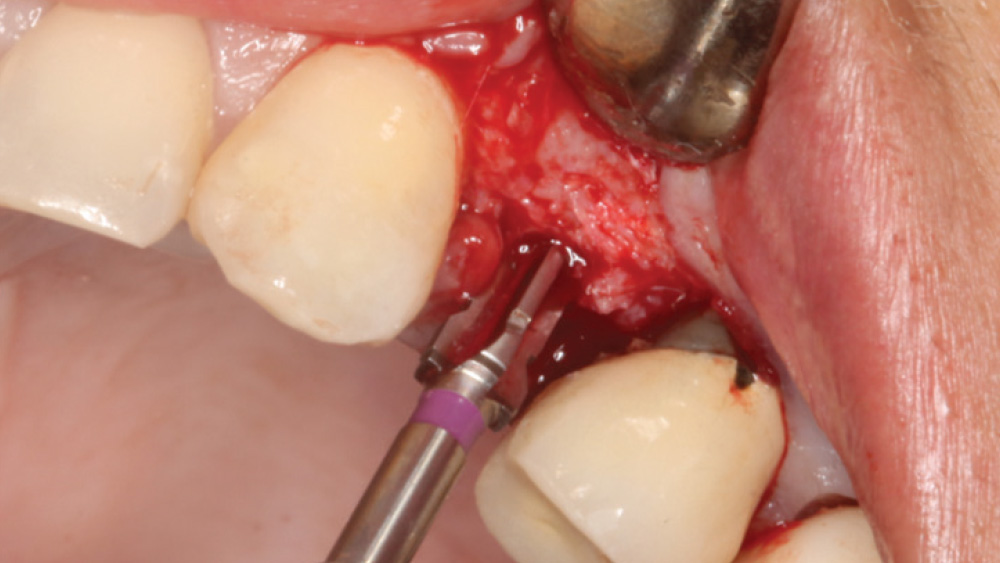
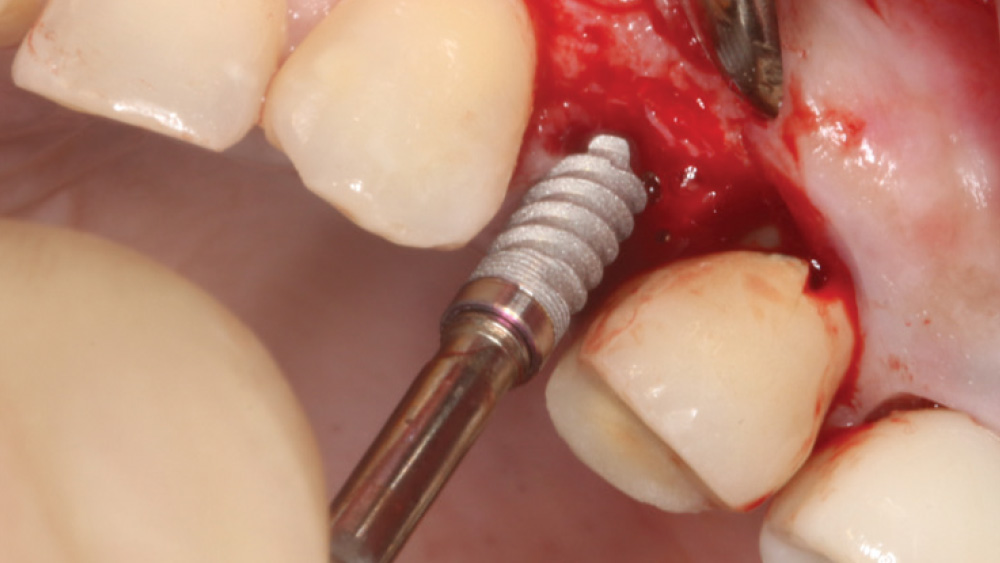
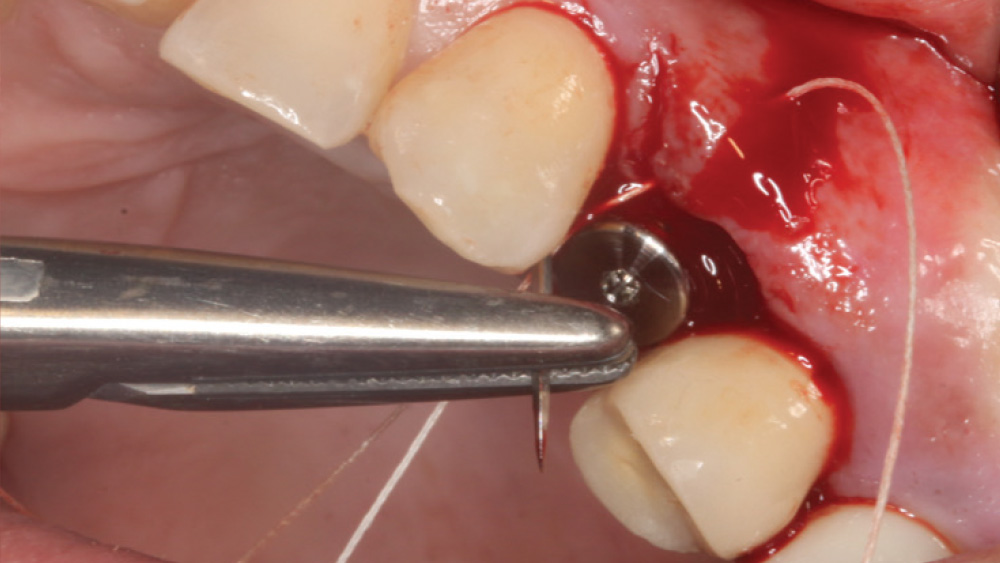
When the attached tissue is minimal, a flap procedure allows the surgeon to reposition the flap to create more attached gingiva and improve the interdental papillae at the implant site. Reflecting a gingival flap also enables the practitioner to more clearly see the final position of the implant at the crest of the bone. If it’s necessary to visualize the bone during the surgical procedure due to uncertain ridge width or height, flap reflection is the safest, most predictable approach.
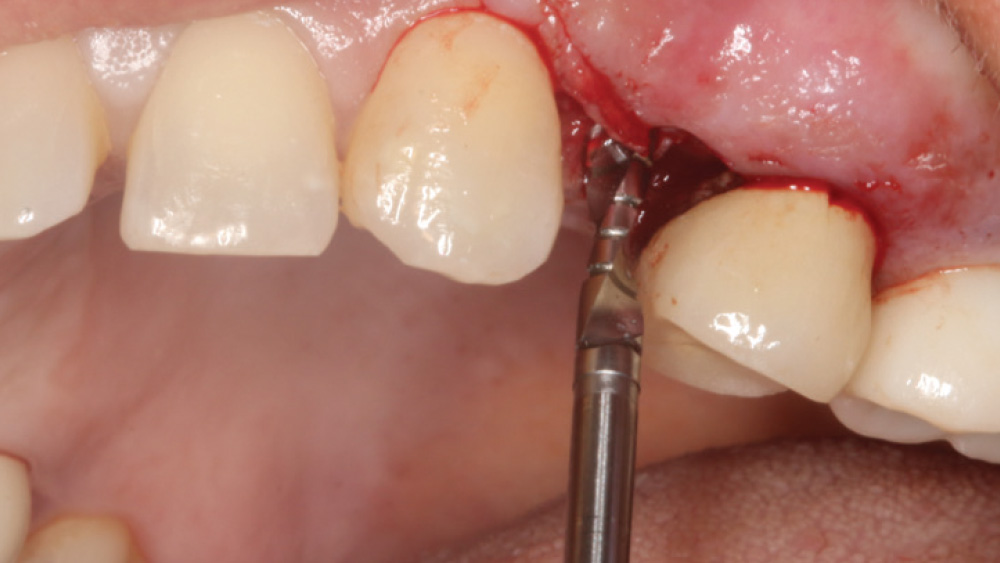
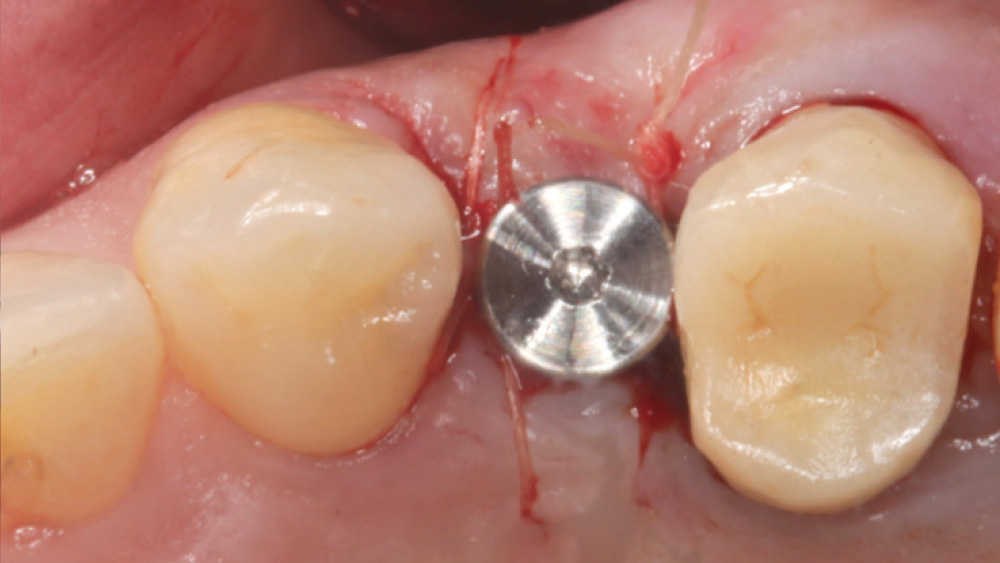
In contrast, with a flapless procedure, a tissue punch is used to gain access to the bone through the gingiva, minimizing postoperative discomfort by eliminating incisions in the mucosal tissue. Whenever mucosal tissue is incised, prostaglandin and histamine are released, resulting in potential postoperative swelling and pain. Therefore, when there is an adequate width of attached gingiva on the facial aspect of an implant site, a flapless procedure may be indicated, eliminating any suturing requirements.
Advantages of Flap Procedure
- Flap can be repositioned to create more attached gingiva
- Visualization of, and access to, the underlying bone
- The final positioning of the implant platform can be observed
Advantages of Flapless Procedure
- Simple, efficient access to the implant site
- Postoperative swelling and discomfort are minimized
- No suturing required
CASE REPORT
The following case, which I performed alongside Dr. Stephanie Tilley of Pensacola, Florida, illustrates the use of both surgical techniques for the same patient, who presented with edentulous spaces in the areas of both right and left maxillary first bicuspids. Due to varying soft-tissue volume on each side of the arch, implant surgery was performed using a flapless procedure for one site, while the attached gingiva was reflected to expose the available hard tissue for the other. As a result of proper site evaluation, treatment planning and restorative-driven implant placement, both surgical techniques led to successful outcomes for the patient.