Rapid Anesthesia Photo Gallery
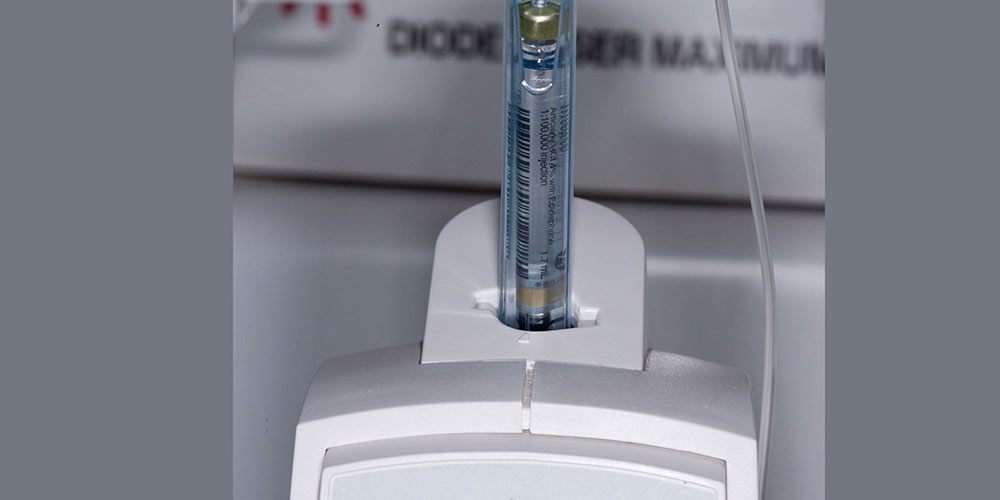
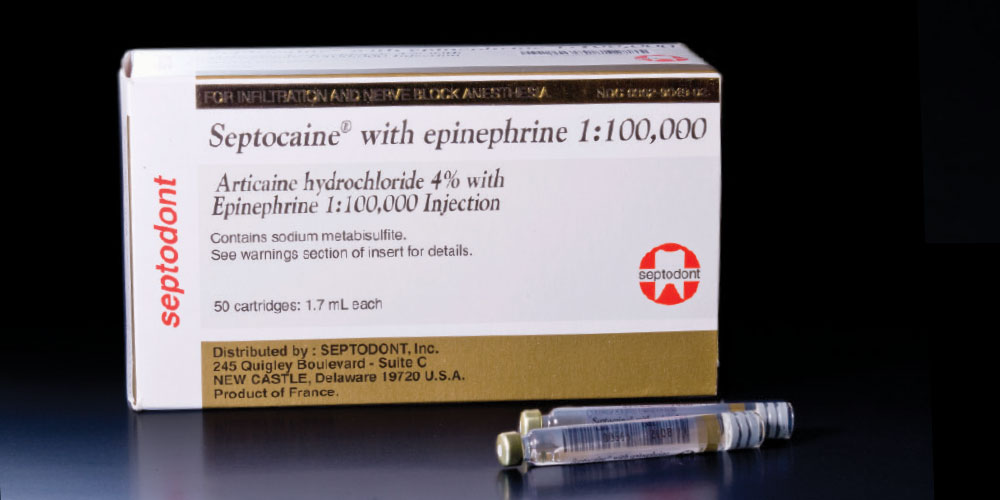
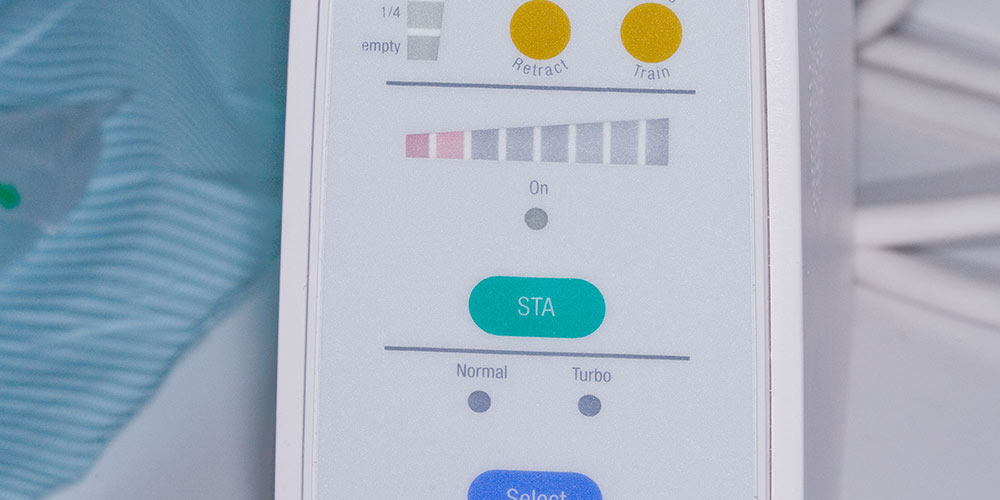
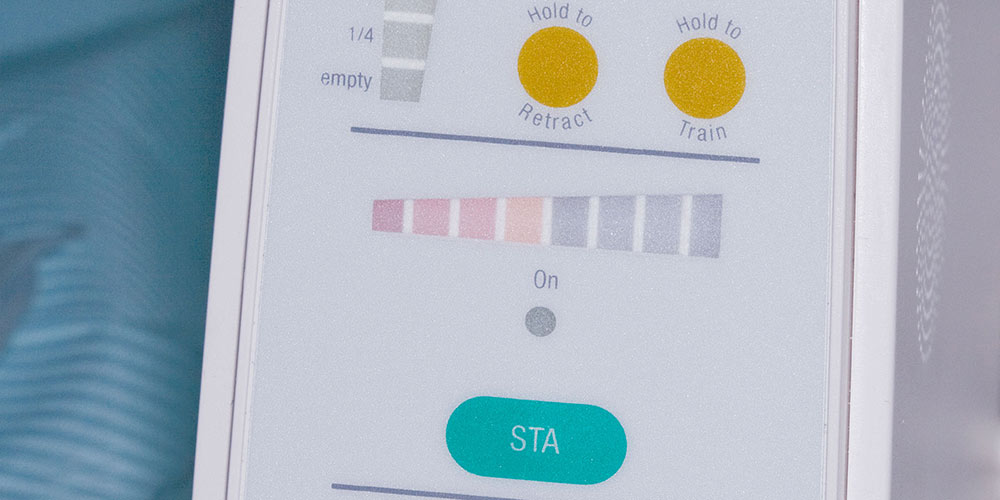
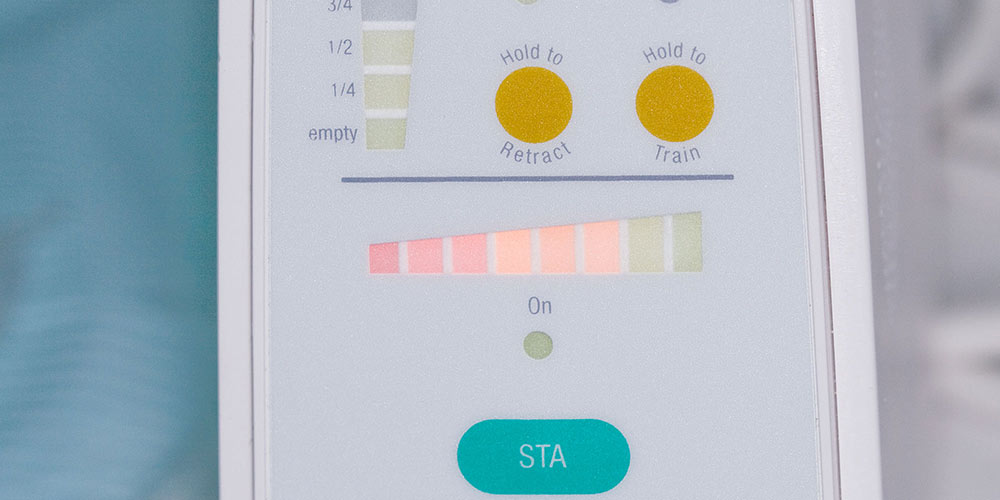
I get more questions about the Rapid Anesthesia Technique than any other topic I talk about, so I thought it would be good to demonstrate it step by step. I have stopped giving lower blocks for single mandibular molars. It is a painful injection for the patient, it takes a while before the anesthesia is profound, and the block is missed approximately 20% of the time by dentists. A couple of years ago I was prepping tooth #19 for a crown and the patient still had some sensitivity. I stopped and gave the patient a PDL furcation injection and was able to finish the prep without any more sensitivity. After the patient was dismissed, my dental assistant asked me, if that furcation injection is the one that finally provided pulpal anesthesia on many cases, why didn’t I just start with that injection? I now use the Rapid Anesthesia Technique for all single mandibular molars and some occasions where I am working on two mandibular teeth. For full mandibular quadrants I still give a lower block, but the STA™ System (Milestone Scientific; Livingston, N.J.) you will see demonstrated in this article makes lower blocks less painful and more effective. Patients who hate injections don’t mind the Rapid Anesthesia Technique, making it a great way to deal with the dental phobics in your practice as well.
Profound Lite is the strongest topical anesthetic I have ever used, and it allows me to brag to patients that I can give them a painless injection.