Using a Screening Device to Incorporate Sleep Dentistry Into Your Dental Practice

According to the American Academy of Sleep Medicine and the Sleep Research Society, adults require seven or more hours of sleep each night to promote optimal health. Routinely sleeping less than seven hours a night can be detrimental to overall health and lead to far more serious health issues, including depression, diabetes, heart attacks, hypertension, strokes and obesity.1 Unfortunately, nearly a third of U.S. adults report getting less than the recommended amount, and roughly 39 percent of adults in my state of Georgia have reported insufficient sleep.2
This story is not all gloom and doom. As dentists, we are in a unique position to screen for and treat a number of sleep-related disorders, including obstructive sleep apnea (OSA) with a physician’s diagnosis, and get our patients to sleep longer and better to avoid adverse health risks. A decade ago, I adopted dental sleep medicine as well as other services into my practice, like BOTOX® (Allergan, Inc.; Irvine, Calif.) and dermal fillers, to address a whole host of issues that patients typically have. Dental sleep medicine has become such an integral part of my practice that every patient I see is screened for airway issues at the dental chair. My staff is also trained to ask pertinent questions, like, “Are you sleepy during the day?” and “Does your partner say you snore?” which are also on our health history form along with other sleep-related questions.
Dental sleep medicine has become such an integral part of my practice that every patient I see is screened for airway issues at the dental chair.
BEFORT USING THE SCREENING DEVICE
When a patient comes in for a cleaning or my advertised free sleep consult, I begin my examination by inspecting the oral cavity for signs of oral cancer, bruxism and decay, and use the Mallampati scale to determine how likely the patient is to have an obstructed airway (Fig. 1). I have the patient complete an Epworth Sleepiness Scale (ESS) questionnaire and have a conversation with the patient regarding any concerns I may have. I will also tell the patient if I have reason to believe they suffer from bruxism, snoring or another more serious sleep disorder.
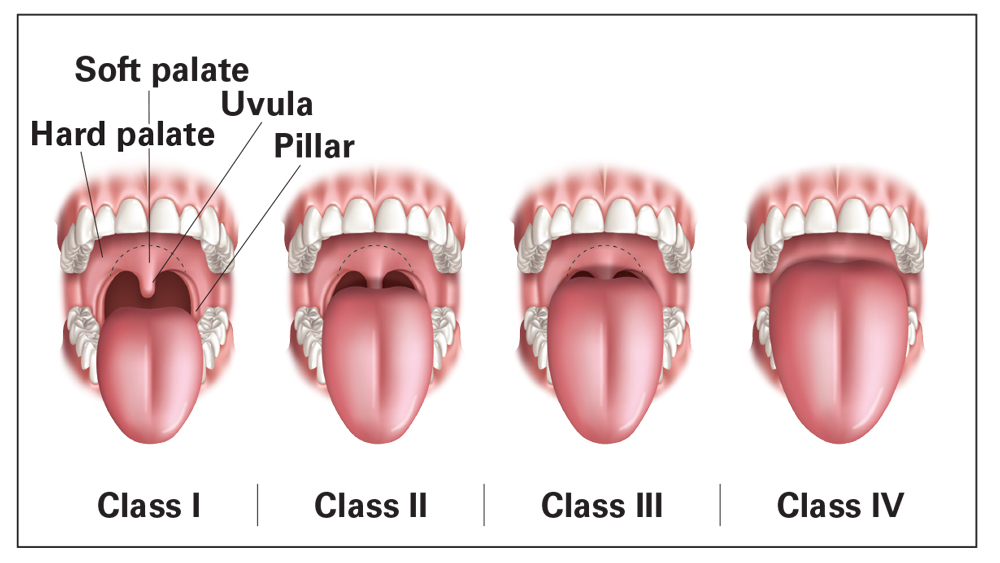
Figure 1: The Mallampati scale is used to determine how obstructed or unobstructed the airway is by visual assessment. The higher the class, the higher the likelihood of an airway issue.
First, I explain what I discovered during my exam. If there are signs of bruxism, we discuss the evidence and I tell the patient an oral appliance is needed. However, before patients are fitted with an appliance, I require them to wear the GEMPro Wellness Monitor (Glidewell Direct; Irvine, Calif.), a screening tool that is used to assist in the detection of airway issues and nighttime bruxism by measuring parafunctional electromyographic (EMG) activity, heart rate, oxygen saturation, body position and snore sounds (Fig. 2). The GEMPro is worn overnight by the patient and gives valuable information that we use to provide the best treatment for each case. It will be able to tell us if they brux or snore, and it can also tell us if they are experiencing oxygen desaturations — an indicator of an underlying airway issue, like OSA. Prescribing an appliance without sending the patient home with the GEMPro or having the patient otherwise screened can potentially worsen other symptoms or create new problems for the patient. It is paramount to understand the full extent of a patient’s sleep-related disorder.

Figure 2: With the GEMPro Wellness Monitor, doctors can screen for the likelihood of obstructive sleep apnea, pinpoint the cause of parafunctional activity, determine the optimal oral appliance and confirm the efficacy of a prescribed appliance. Each kit includes a biofeedback amplifier, a tablet preloaded with a purpose-built screening app, and a pulse oximeter with a finger probe attachment.
GETTING PATIENTS TO ACCEPT THE GEMPro
Once my patients and I agree on the next step, I become more specific in discussing how we will proceed. I inform them that there is a high likelihood they have sleep apnea and oxygen desaturations, based on how they responded to the questionnaire and health history form. I explain how snoring is part of a continuum, with snoring on one end and sleep apnea on the other, and that the information we get from the GEMPro will determine if they are snoring only or if we need to dig a little deeper and continue in the direction of a physician-prescribed lab sleep test. I also explain that the GEMPro uses two simple, small, noninvasive sensors — a fingertip pulse sensor and an adhesive pad on their jaw muscle — to summarize the quality of their sleep and guide our decisions.
To help nudge patients toward acceptance, I offer the use of the GEMPro at no charge. In addition, most patients do not like the thought of having to spend the night in a lab to determine whether they have any sleep issues. In most cases, the GEMPro eliminates an overnight visit and an out-of-pocket fee, and I receive the results within 24 hours.
After the initial discussion and review of the documentation, health and family history, and pictures of the patient’s airway, most patients agree to wearing the GEMPro. From there, our patient coordinator schedules a night to send the patient home with the GEMPro, instructs them on how to initiate the sleep screening in the comfort of their own home, and explains that the results of the screening will influence the next steps toward treatment.
USING THE GEMPRO DATA: YOUR NEXT STEPS
After the patient completes his or her sleep study, the data is automatically emailed to my office, where I use a simple flowchart to guide my recommendation (Fig. 3). This is where the GEMPro really shines as a practice screening tool. The results from the GEMPro will lead me in one of four diagnostic directions: (1) bruxing or clenching; (2) snoring and grinding; (3) snoring only; and (4) oxygen desaturations with or without a secondary or tertiary issue. If only bruxing or clenching is found, I can prescribe a nightguard, like a Comfort H/S™ Bite Splint. If snoring and grinding are found, I can prescribe an appliance to treat both issues, like an EMA®, dreamTAP™ or Silent Nite® sl (Glidewell Laboratories). If only snoring is found, I can prescribe an appliance or device, like the EMA, dreamTAP, Silent Nite sl or aveoTSD® (Glidewell Direct). But, if oxygen desaturations are found, I will refer the patient to a sleep physician or to their primary physician to evaluate and possibly order a sleep test. A lab sleep test will determine the extent of their oxygen desaturation, and their physician can either prescribe continuous positive airway pressure (CPAP) therapy, or refer the patient back to my office for delivery of an appliance that treats OSA. I deliver an appliance to every patient who completes the process and exhibits the appropriate symptoms; the only difference is the type of appliance that is prescribed. It’s a win-win for everyone.
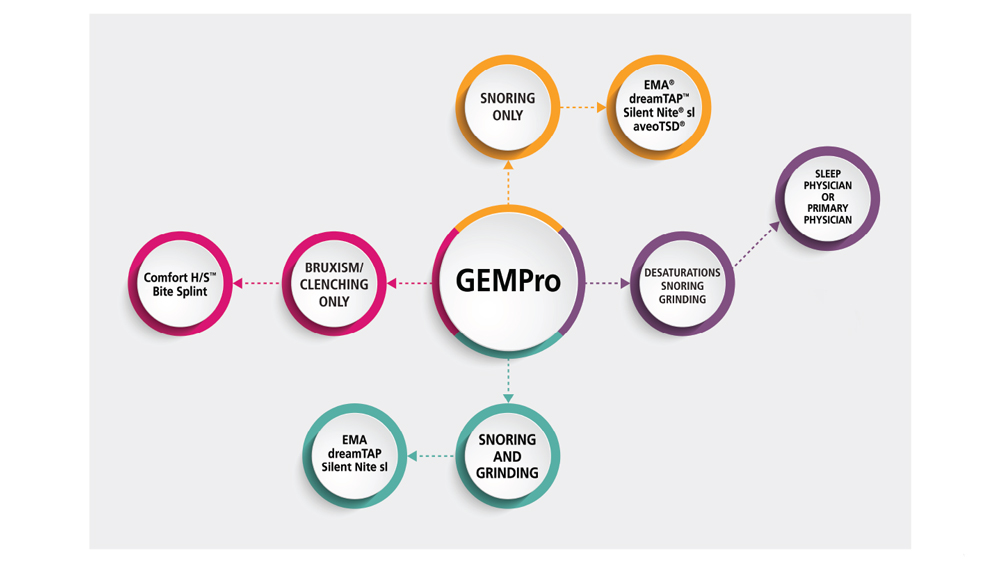
Figure 3: This chart represents the treatment routes I take after receiving a patient’s results from the GEMPro Wellness Monitor.
RECOMMENDATION
Dental sleep medicine has been an incredibly rewarding addition to my practice, and I believe every dentist should be thinking outside the box and screening for sleep-related disorders. Clinicians already have patients in the chair and examine their oral cavity; it takes only a few extra steps to diagnose and treat existing sleep disorders. By utilizing tools like the GEMPro, which brings with it a simplified workflow to systematically diagnose patients effectively and accurately, the adoption of dental sleep medicine into a practice is even easier than before. To get a better idea of the number of patients in your practice who can benefit from this service, simply add a section to your health history form focused on snoring and daytime sleepiness. Once you see how many patients you can help, you will understand how widespread this problem is and just how important our role is in providing treatment. Commit yourself to screening patients, test the extent of their sleep-related disorders with the GEMPro, and deliver a potentially life-saving appliance.
Dental sleep medicine has been an incredibly rewarding addition to my practice and I believe every dentist should be thinking outside the box and screening for sleep-related disorders.
References
- ^ Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015 Jun 15;11(6):591-2.
- ^ Sleep: sleep and health among adults in Georgia [internet]. Department of Health & Human Services: National Center for Chronic Disease Prevention and Health Promotion: Division of Population Health; 2016 Nov [cited 2017 Oct 10]. Available from: https://www.cdc.gov/sleep/pdf/states508/FS_ShortSleepByState_GA_508tagged.pdf.



