Interview with Donald E. Frantz, DDS: Inventor of the EMA® Appliance

In 1993, Houston, Texas-based orthodontist Dr. Donald Frantz invented the EMA® (Elastic Mandibular Advancement) appliance, a device that treats snoring and obstructive sleep apnea by advancing the mandible and opening the bite to allow for less restricted airflow during sleep. The custom appliance provides gradual mandibular advancement by using elastic straps, available in nine strap lengths and four different elastic tension options. In this interview, Dr. Frantz discusses how his own experience with sleep apnea led to the development of the EMA, his shift in practice focus from orthodontics to dental sleep medicine, and what he recommends to clinicians who are just getting started in treating sleep-disordered breathing.
DR. NEIL PARK: Tell me a little bit about the beginning of the EMA appliance.
DR. DONALD FRANTZ: Back in the mid-1980s, my wife pointed out to me that I would stop breathing when I slept. At this point, I had been practicing orthodontics for decades, yet I was completely ignorant about dental sleep medicine. My son Michael had an orthodontic lab, and he made all the retainers I used in my orthodontic practice. I told Michael, “We need to come up with a comfortable sleep appliance.” And he said, “Well, if I’m going to be involved, it needs to be easy to make and relatively low in price.” So I decided, if I was going to be part of it, the appliance needed to be comfortable to wear. As an orthodontist, I had many patients who wore retainers after I straightened their teeth, so I knew about the importance of having a very comfortable and minimal appliance. Michael said the two orthodontic retainers were easy for a lab to make, and he suggested that we connect he two retainers with elastic straps — which was a great idea because elastic ensured that the patient’s mandible would not be locked in any one place. From there, we worked on firm straps so that once clinicians titrated their patients and found their mandibular “sweet spot,” they could provide firm elastic without having their patients continuously stretch out straps and pay for new ones.
NP: Were the results immediate? Who were the first patients you tried the EMA appliance on?
DF: I was practicing in the Houston- Galveston, Texas, area, where Dr. Sam Kuna had a sleep lab. I went to the lab, and I said, “We’ve got a new mandibular advancement appliance, and we would like to conduct a product trial on your patients to see how effective the appliance is.” Fortunately, not only did the lab give their OK to offer their patients the appliance on a trial basis, but Dr. Kuna also got a $1.58 million NIH grant to study the appliance. That’s how we got our foot in the door.
NP: Now, at that point, CPAP (continuous positive airway pressure) was the established standard of care.
DF: Yes. In fact, my other son Joe and I went to both dental and medical sleep meetings. At one medical sleep meeting we went to, a couple of physicians walking down the aisle said, “Look at those snake oil salesmen over there thinking they can treat obstructive sleep apnea.” Now, at the physicians’ meetings, they ask us, “Do you know a good dentist who can treat sleep apnea?” So it’s changing.

Available through Glidewell, the EMA appliance noninvasively treats snoring and obstructive sleep apnea by both advancing the mandible and opening the bite to allow for less restricted airflow during sleep. The EMA appliance is offered with a range of strap sizes and multiple elastic tension options to suit the individual needs of patients and maximize comfort.
NP: It really is. So how is the EMA different from other appliances that are on the market?
DF: For our technique, Michael and I decided to use the “KISS” method: “Keep it simple, sweetheart.” For example, you can now use a George Gauge™ (Great Lakes Orthodontics, Ltd.; Tonawanda, N.Y.) to determine how far the mandible can come forward, but before the George Gauge came along, I would look at the patient and say, “The maxilla and mandible may be coming 12 mm apart, so let’s set the buttons 25 mm apart so that a 21 mm strap will advance your mandible 4 mm.” That’s where we started. And fortunately, the EMA appliance was working on the patients in Dr. Kuna’s lab.
NP: We all know the statistics: There are so many people who suffer from snoring and obstructive sleep apnea, yet only a small percentage of those patients are being treated. How do we get this moving? If we know about the many health consequences that can result from snoring and sleep apnea, how do we get more people treatment?
DF: I don’t understand why more dentists aren’t jumping on this. Those clinicians are missing out on additional opportunities for rewarding connections with their patients — I’ve had so many sleep patients lift me off the ground with a big hug and say, “You’re my favorite guy.” Those experiences really make life worth living for me.

Dr. Donald Frantz (left) with Dr. Neil Park (right), vice president of clinical affairs at Glidewell.
NP: After you started working in dental sleep medicine, did it change the nature of your orthodontic practice?
DF: Absolutely. Over a decade ago, I stopped seeing orthodontic patients and started treating only sleep apnea patients. Treating those patients has brought me such joy.
NP: And what advice do you have for dentists just getting started in treating sleep-disordered breathing?
DF: Don’t be afraid — fear motivates so much more of what we do than we’d like to admit. Don’t let fear interfere with stepping out there and treating people in need. We have dentists who were excited to begin practicing dental sleep medicine two years ago yet still haven’t treated a patient because they’ve been too afraid. As a result, at least 50% of their patients are still suffering. A lot of dentists are intimidated by the number of straps that EMA offers. I always recommend starting with the 21 mm yellow strap. Even if the buttons are set 25 mm apart, unless the patient has TMJ pain, then you can set the buttons even further apart so that 2 mm mandibular advancement can take place. It may not seem like it, but you’re actually helping the patient by pulling their jaw forward.
NP: So what do you say to dentists who are nervous about TMJ responses?
DF: I tell dentists who treat patients that have temporomandibular joint disorders (TMD) to go slowly. Have your office call the patient the morning after you first put the appliance on, and find out if the patient has TMJ pain on one side or both sides. If they have TMJ pain on both sides, you take the straps off. If they have TMJ pain on one side, you need to reduce the pain side a little bit.
NP: What is your standard protocol, then? When a clinician is just starting with a patient who’s a snorer yet has no TMD symptomatology, how do you suggest they treat that patient?
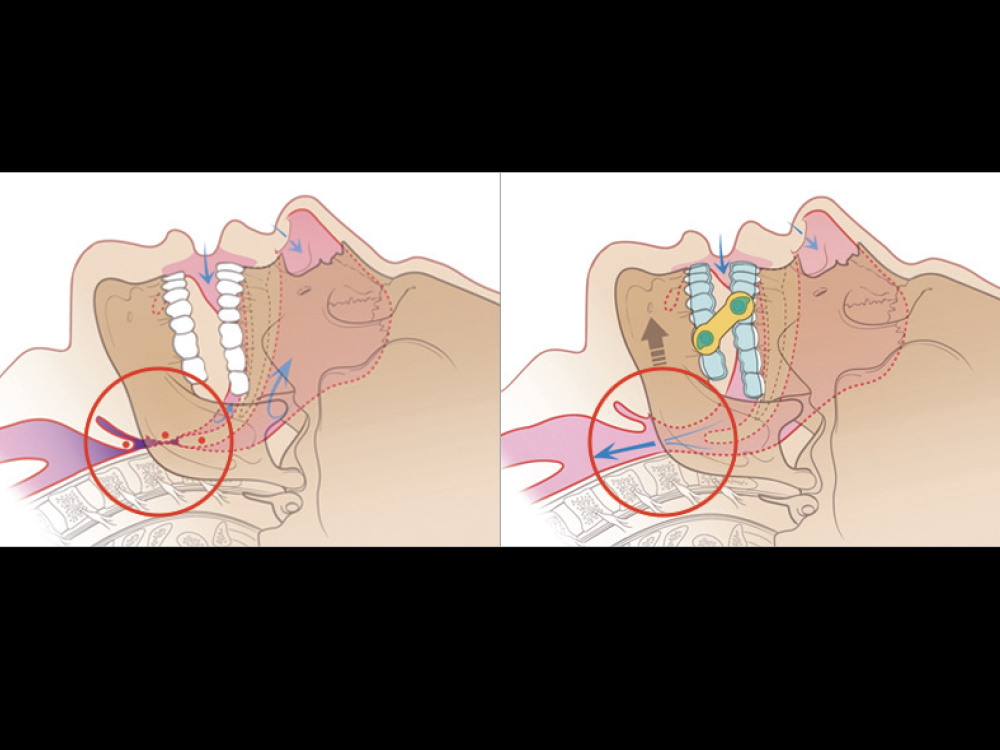
Without the EMA, the patient’s airway is obstructed by soft tissues (left). With the EMA, air is able to flow freely through the patient’s airway (right).
DF: You’ll want to put the standard occlusal bite pads on so that you have maybe 8 mm of vertical space. Set the buttons 25 mm apart and start the patient on a 21 mm yellow strap, and if the following week the patient has no TMJ pain, shift to a 19 mm strap. No TMJ pain after three or four nights? Transition from the 19 mm strap to the 17 mm strap, then maybe use a 15 mm yellow strap. Still no improvement? Go back and increase the vertical space. These are the signs of improvements you should be looking for in your patient: No reports of snoring, waking up feeling rested, and lack of daytime sleepiness.
NP: This is great practical advice. Thanks so much for your time.
DF: Thank you.