Medical Evaluation: Part 1 — Preoperative Evaluation of the Dental Implant Patient

The medical evaluation of patients considering dental implant treatment is an important and vital aspect of the treatment planning process. The primary goal of the preoperative medical evaluation is to assess the risks associated with the dental implant treatment. Patients presenting for implant treatment may appear to be in a healthy state when they actually have serious underlying systemic diseases or are on medications that could predispose them to complications and increased treatment morbidity. Older patients today, even those with life-threatening diseases, are more socially active and have a better quality of life because of advancements in medical care. Therefore, these higher risk patients are increasingly seeking rehabilitation for edentulous areas with implants because of the high success rate and increase in dental function.
Numerous studies have been conducted evaluating the relationship between patients’ medical condition and dental implant morbidity. Scully concluded that 30% of patients seeking dental treatment have some type of relevant medical condition.1 Silverman et al. evaluated dental patient medical histories and reported 15%–25% were described as “medically complex,” which includes a history of systemic diseases, multiple medications or age-related health issues.2,3 Medically compromised patients with diseases such as diabetes, osteoporosis and hypothyroidism have been reported through various studies to have significantly lower dental implant survival rates compared to healthy subjects.4,5
In addition to evaluating systemic diseases, clinicians must also take into consideration the relationship of prescription and over-the-counter (OTC) medication. For patients aged 60 and over, approximately 40% are taking five or more prescription medications, 15% are taking 10 or more prescription medications, and 67% are taking a combination of five or more prescription and OTC medications.6 Many of these medications have a direct impact on the healing and success of dental implants.
Because many of our patients have underlying medical conditions and are taking medications that may impact dental implant treatment, it is imperative that implant clinicians have a thorough understanding of the medical evaluation process. This article is the first of three on the topic of the medical evaluation of dental implant patients. Part 1 will discuss the significance of the medical history, the differences between relative and absolute contraindications, and the importance of obtaining proper medical consultation/clearance for medically complex patients. Part 2 of this series will include a detailed overview of various systemic diseases that directly have an effect on the implant treatment, and Part 3 will discuss medications that directly impact the surgical and healing phases of implant treatment.

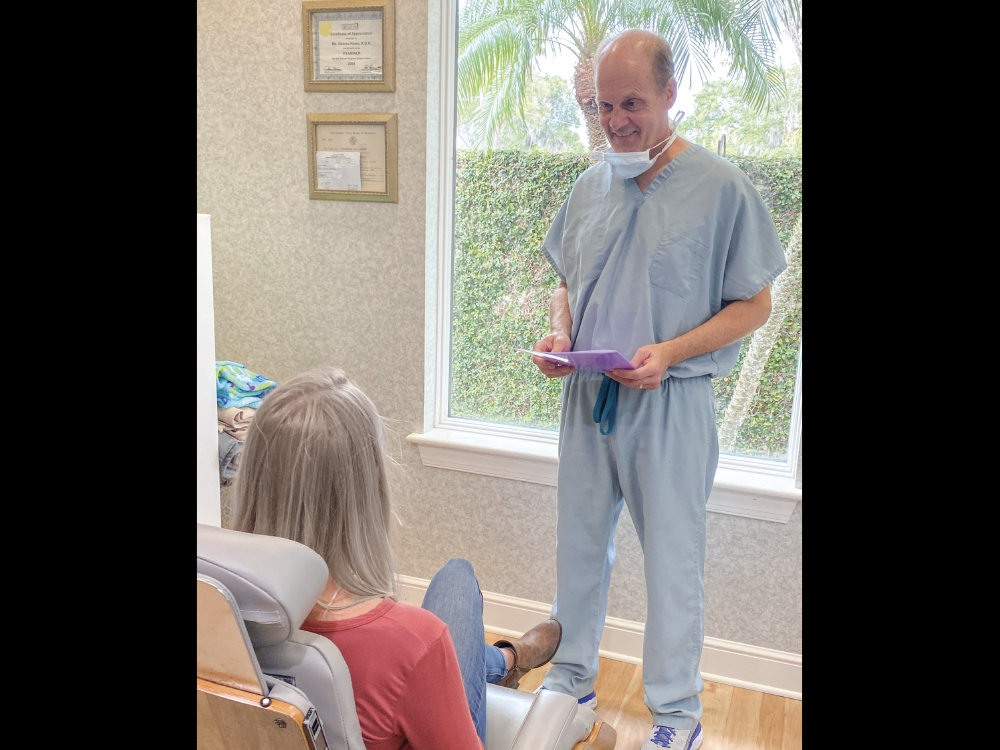
For patients considering dental implant treatment, medical evaluation is an important part of the treatment planning process.
DENTAL IMPLANT PATIENT EVALUATION
In implant dentistry, case selection is paramount in obtaining proper wound healing and metabolic stability after implant and bone grafting procedures. Some medical conditions may predispose the patient to compromised responses to surgical procedures, which may lead to infection, impaired healing or possible failure. Therefore, these disease states must be carefully evaluated by the clinician preoperatively.
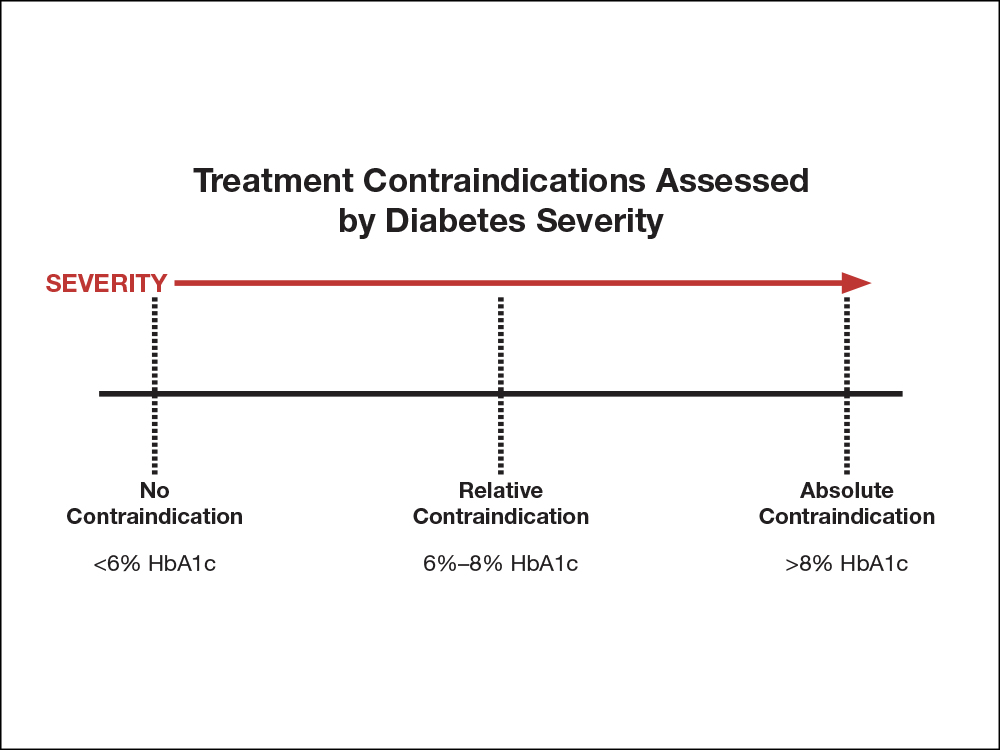
Figure 1: Example of relationship between disease severity and treatment contraindications for diabetic patients.
TABLE 1: FACTORS FOR ASSESSING HEALTH STATUS AND RISK
- Present and past medical history
- Present and past dental history
- Present and past medication use
- History of allergies
- Social history and use of recreational drugs
- Type of intended treatment
- Length of treatment
- Invasiveness of treatment
- Psychological status
- Degree of treatment urgency
- Use and type of sedation
There are many factors associated with assessing the patient’s health status and risk, including the patient’s current and past medical and dental history, current and past use of medications, history of allergies, and social history (Table 1). When evaluating systemic diseases, a wide range of direct effects to dental implant treatment may be present depending on the severity of the disease. For example, a diabetic patient with a hemoglobin A1c (HbA1c) of less than 6% has no limitations to treatment and is considered to be in the category of “no contraindication.” If this patient had an HbA1c of 6%–8%, this would be classified as a “relative contraindication.” If the same patient had an HbA1c of greater than 8%, then the patient is considered to be in the category of an “absolute contraindication.” Therefore, in a general sense, one can see how the severity or degree of control of a disease has a direct effect on treatment contraindications (Fig. 1).
TABLE 2: AMERICAN SOCIETY OF ANESTHESIOLOGISTS (ASA) CLASSIFICATION
ASA1: Normal, healthy patient
ASA2: Patient with mild systemic disease with no functional limitations (e.g., controlled hypertension, controlled diabetes, chronic obstructive pulmonary disease with mild symptoms)
ASA3: Patient with severe systemic disease with definite functional limitations (e.g., uncontrolled hypertension, uncontrolled diabetes, chronic obstructive pulmonary disease with exercise intolerance)
ASA4: Patient with systemic disease that is a constant threat to life
ASA5: Moribund patient who is not expected to live less than 24 hours
In 1941, the American Society of Anesthesiologists (ASA) adopted a physical status classification system based on the severity of the patient’s underlying conditions (Table 2).7 This system is universally used in medicine today. Although the classification was originally designed to estimate the medical risk for a patient receiving general anesthesia for a surgical procedure, it is now utilized as a general evaluation for medical risk. Weyant et al., in a retrospective analysis of the Veterans Affairs registry data, found that the medical status of patients (i.e., medical history, ASA category and medication history) correlated with dental implant failure.8 Ideally, dental implant patients should be classified as ASA1 or ASA2 for dental implant treatment. In some cases, ASA3 patients may be treated, but only after medical consultation and clearance.
MEDICAL HISTORY
The two basic categories of information addressed during the review of the patient’s medical history are the following: 1) medical history; and 2) systemic health. In most cases, dental offices use a medical evaluation form to obtain the majority of this information. A review of the body systems via a patient interview should be completed, and any positive answers should be further investigated.
In addition, a history of medication usage — including prescribed medications, over-the-counter medications, herbs and supplements — and systemic and drug allergies should be detailed. The specific medications being used to treat any medical condition should be noted along with a history and dosage information collected. It is of utmost importance that all information on the medical forms be reviewed with the patient to ensure all questions are answered accurately and truthfully.
SYSTEMIC DISEASE AND ORAL IMPLANTS
Systemic diseases play a vital role in treatment planning and implant therapy for patients. The effects of systemic disease on wound healing, bone metabolism and implant success are well documented in the literature. The implant clinician should utilize the specific systemic disease information obtained in the medical history in the planning and management of all phases of dental implant treatment. It is the responsibility of the implant clinician to understand the interrelationship of systemic diseases and the various treatment phases of implant dentistry.
As stated prior, the severity and degree of the systemic disease may be far more significant than the nature of the disorder itself. Therefore, a comprehensive evaluation should be completed in the decision process prior to implant therapy. For many of these patients, the increased quality of life and functional benefits from dental implants may outweigh the risks involved in performing the procedure. To assist in making these decisions on a patient’s treatment, the various types of contraindications must be understood.

All information on the medical forms should be reviewed with the patient to ensure each question is answered accurately.
CONTRAINDICATION CLASSIFICATION
In traditional medicine today, a contraindication is defined as a condition or situation that potentially makes the procedure in question inadvisable. There are two types of contraindications:
- Absolute contraindication is a condition that may result in major and significant medical problems with a high incidence of implant or bone graft failure. The risk of performing the procedure clearly outweighs any possible benefit. Undertaking procedures when these conditions are present is inadvisable.
- Relative contraindication is a condition that necessitates caution and is acceptable as long as the benefits outweigh the risks. In most cases, precautions need to be taken and the intended procedure may require some degree of modification to ensure safety and success.
To further clarify the contraindications in the field of implant dentistry, they may be classified into three categories (Table 3):
- Surgical contraindication: A condition that places the patient at medical risk during the surgical procedure (e.g., advanced cardiovascular disease) that potentially could result in a medical emergency. However, the condition does not directly impact morbidity or success of the implant procedure.
- Implant contraindication: A condition that places the endosseous implant healing at risk (e.g., IV bisphosphonate use), which may result in a decreased success rate and increased morbidity. However, the condition does not impact the intraoperative medical condition of the patient or place the patient at a medical risk.
- Surgical/implant contraindication: The combination of a surgical procedure risk with a risk for the success of implant healing or longevity. For example, with uncontrolled diabetes: 1) a patient may be predisposed to medical complications because of associated cardiovascular disease; and 2) implant healing may be impaired because of the uncontrolled diabetes.
TABLE 3: EXAMPLES OF SURGICAL VS. IMPLANT CONTRAINDICATIONS
Surgical Contraindications
- Uncontrolled hypertension
- Advanced chronic obstructive pulmonary disease (COPD)
- Unstable angina
- Class 4 congestive heart failure
- Recent myocardial infarction
- Bleeding disorders
Implant Contraindications
- IV bisphosphonate use
- Uncontrolled diabetes
- Immunosuppressive medications
- Heavy tobacco habit or alcohol use
- Uncontrolled hypothyroidism
- Past radiation therapy to the surgical site
- Titanium allergy
MEDICAL CONSULTATION AND CLEARANCE
Obtaining a medical consultation/clearance is a necessity with patients who present with complicated systemic conditions, medications and predisposing factors that may lead to treatment complications. Collaboration and coordination with the patient’s health care provider is paramount in meeting the goal of safety and improving the patient’s health.
Clinicians must have a clear understanding of the difference between a “medical consultation” and a “medical clearance.” A medical consultation is defined as a procedure that is requested by one healthcare provider to another, which involves reviewing the patient’s medical history, examination of the patient, and recommendations for care and treatment. In contrast, a medical clearance is an official authorization, usually in writing, to allow a procedure to proceed. This is often troublesome to many physicians, as a potential liability situation may result. In addition, dentists may believe that because they have clearance, they are free of liability because they obtained permission and authorization to proceed with the procedure. This is often misleading and may place the dentist in a compromised medicolegal situation. In general, the dentist is ultimately responsible for any decisions and treatment he or she provides to the patient, as no patient is completely free of risk when undergoing a procedure.
Therefore, to protect the dentist and patient, a hybrid medical consultation/clearance form was designed by the author and Francis J. DeLuca, DMD, J.D. The intent of this form is to fully educate the physician on the intended procedure, protect the dentist medicolegally, and provide the dentist with sufficient information to make an informed decision on whether to proceed with treatment (Figs. 2a, 2b).
PART 1: COVER LETTER
A cover letter should always be provided to the physician with the following information:
- Introduction of the dental provider and the patient in question
- Intended procedure (e.g., placement of two implants in the maxillary posterior region)
- Date of the intended procedure
- The type of anesthesia (local) and sedation (oral, conscious or general)
- Duration of procedure (e.g., two hours)
- Anticipated blood loss (e.g., minimal,moderate, severe)
- Contact information
PART 2: INFORMATION PROVIDED BY THE PATIENT
The clinician should relay any of the following information that was provided by the patient: 1) medical history; 2) current medications; and 3) allergies. The reason for this is to allow the physician to evaluate what information the patient has provided so the physician may make any additions or modifications (i.e., in some cases, patients may not provide a complete and accurate medical history). Patients are not always forthright in providing medical information. It is not uncommon for a patient who has been denied care elsewhere because of a medical issue to omit critical information.
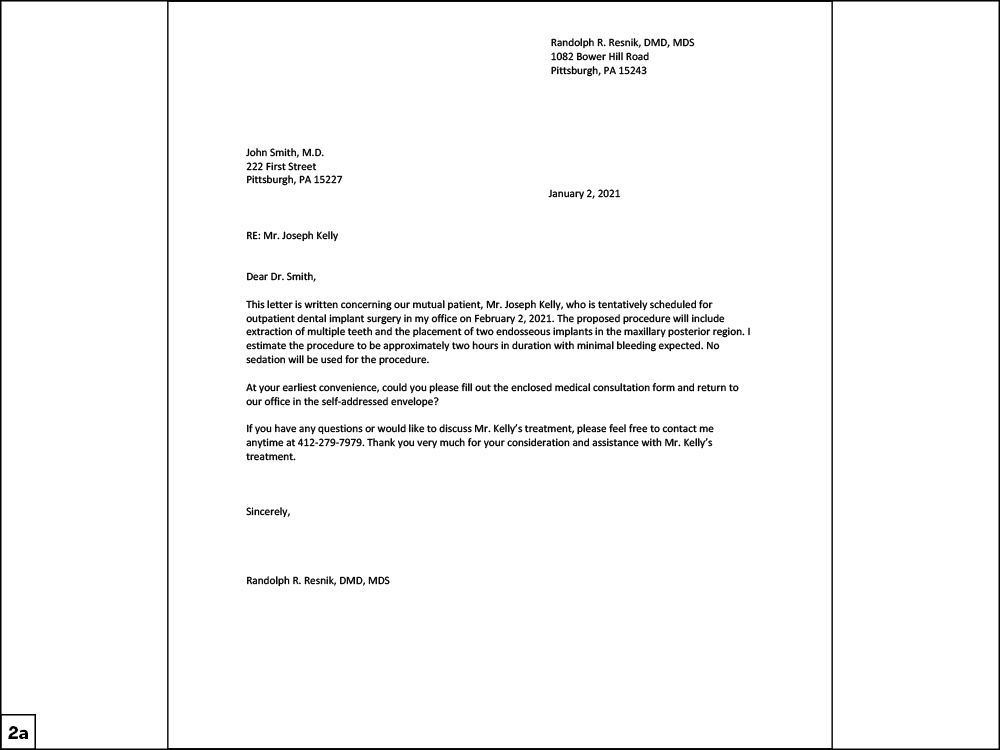
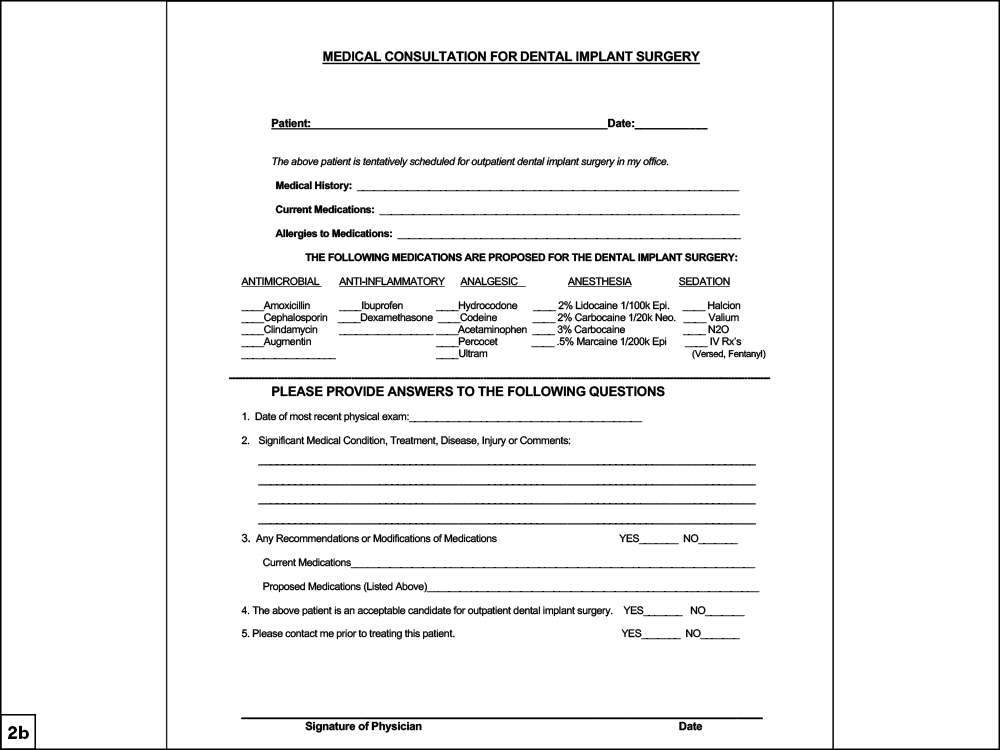
Figures 2a, 2b: Developed by Dr. Randolph Resnik and dentist-attorney Dr. Francis DeLuca, the medical consultation/clearance form educates the physician on the intended procedure, protects the dentist medicolegally, and provides the dentist with sufficient information to make an informed decision on whether to proceed with treatment.
PART 3: MEDICATIONS TO BE PROVIDED BY THE DENTIST
Clinicians should provide a list of all medications and dosages they intend to administer or prescribe for the patient. This will allow the physician to modify or remove any medications they feel may not be in the best interest of the patient’s treatment (e.g., the physician may recommend no corticosteroid use if the patient is a diabetic).
PART 4: INFORMATION PROVIDED BY THE PHYSICIAN
The physician will provide the following information:
- Most recent physical examination: To determine whether the patient is keeping up with his or her medical health.
- Significant medical condition, treatment, disease or injury: This will allow the physician to make the dentist aware of a particular medical condition that may have a direct impact on the treatment. In addition, the physician may relate a medical condition that the patient failed to divulge.
- Medication modification: The physician will recommend any modifications to current medications (i.e., medications the patient is currently taking that were prescribed by another healthcare provider) or proposed medications (i.e., medications the dentist plans on prescribing as part of the dental implant treatment). A dentist should never modify any medication that was prescribed by another healthcare provider without written authorization by the physician.
- Is the patient an acceptable candidate? The physician will clear the patient for dental implant treatment in writing, which becomes part of the patient’s permanent chart.
- Contacting the physician: The physician will document whether he or she prefers to discuss the treatment of the patient with the dentist.
It’s important for clinicians to obtain medical clearance for patients who have systemic diseases or are taking medications that may affect implant treatment.
SUMMARY
Clinicians should be proactive in obtaining medical clearance for patients who have systemic diseases or are taking medications that may directly affect the implant process. Placing a dental implant is an elective procedure that requires meticulous evaluation of the patient’s past and present medical history. Dentists must understand that not every patient who presents for implant treatment may be a candidate. Many patients have underlying systemic issues and comorbidities that may result in physiologic alterations to the body’s ability to combat procedural stress and allow for proper implant healing. A prudent clinician should possess the ability to disseminate information obtained on the medical history and ensure that the benefits of treatment outweigh the potential risks.
References
- ^ Scully C. Scully’s medical problems in dentistry [e-book]. 7th ed. Edinburgh: Churchill Livingstone/Elsevier; 2014.
- ^ Silverman S, Eversole LR, Truelove EL. Essentials of oral medicine. Hamilton, ON: BC Decker Inc.; 2001.
- ^ World Health Organization. The world health report 2002: reducing risks, promoting healthy life. Geneva, Switzerland: World Health Organization; 2002.
- ^ Pandey A, et al. A retrospective study to assess outcome of dental implants therapy in medically compromised patients. J Adv Med Dent Scie Res. 2019;7(9):16-20.
- ^ Dutt P, et al. A retrospective study of assessment of survival rates of dental implants in medically compromised patients. J Applied Dent and Med Sciences. 2018 Jan-Mar;4(1).
- ^ Landro L. When patients take too many pills, doctors deprescribe. Wall Street Journal. 2016 Oct 10. Available from: https://www.wsj.com/articles/when-patients-take-too-many-pills-doctors-deprescribe-1476122784.
- ^ Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941 May;2:281-4.
- ^ Weyant RJ. Characteristics associated with the loss and peri-implant tissue health of endosseous dental implants. Int J Oral Maxillofac Implants. 1994 Jan-Feb;9(1):95-102.