Minimizing Complications in Dental Implant Patients Who Use Tabacco and Cannabis (1 CEU)

Use of tobacco and cannabis, whether through traditional cigarettes, cigars, vaping, or waterpipes (hookahs), is associated with a range of systemic and oral health issues, including cardiovascular disease, respiratory conditions, and compromised oral healing. For patients undergoing dental implant and bone graft procedures, these products present unique challenges. The physiological, biochemical, and immunological effects of tobacco, nicotine, and related toxins interfere with healing, increase complications, and significantly heighten the risk of implant or graft failure. As a result, clinicians must fully understand the impact of these products and establish protocols to mitigate legal and clinical risks when treating patients who use them (Fig. 1).




Figures 1a–1d: Habits that negatively affect dental implant outcomes include (a) cigarette smoking, (b) vaping, (c) waterpipe (hookah) use, and (d) cannabis use.
DIRECT EFFECTS ON OSSEOINTEGRATION AND BONE REGENERATION
Compromised Angiogenesis
Nicotine, carbon monoxide, and other harmful substances in cigarettes, e-cigarettes, waterpipes, and cannabis impair angiogenesis by reducing blood flow and oxygenation. This disruption slows the formation of new blood vessels and adversely affects tissue repair and remodeling. Tobacco use also suppresses the expression of angiogenic markers such as vascular endothelial growth factor (VEGF), leading to decreased blood supply and impaired vascularization, which are crucial for bone healing.1
Altered Bone Metabolism
Nicotine and toxins from tobacco and cannabis alter bone metabolism by disrupting the balance between osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells). These changes reduce bone density, delay healing, and compromise bone regeneration and implant stability. Inhalation from waterpipes and vaping devices, often perceived as less harmful, has similar cytotoxic effects on bone cells due to the presence of nicotine and other volatile compounds.
Impaired Healing
Tobacco and cannabis use increases platelet adhesiveness, leading to microvascular occlusion and tissue ischemia. Carbon monoxide in smoke reduces oxygen availability in the blood, further delaying epithelial proliferation and soft tissue healing. Vaping liquids with high nicotine concentrations can similarly impair healing by mimicking these effects. Consequently, users experience delayed wound healing, increased inflammation, and a higher likelihood of infection, all of which contribute to implant failure. A controlled clinical study published in the Journal of Clinical Periodontology concluded that a single cigarette can reduce peripheral blood velocity by 40% within one hour, thereby compromising the healing process.2
CANNABIS EFFECTS ON OSSEOINTEGRATION AND BONE REGENERATION
Cannabis use, whether through smoking or edibles, may negatively impact dental implant success. Smoking cannabis exposes the oral tissues to heat and harmful chemicals, leading to dry mouth (xerostomia), reduced salivary flow, and an increased risk of peri-implantitis and implant failure. Additionally, tetrahydrocannabinol (THC) in cannabis affects cannabinoid receptors (CB1 and CB2), potentially impairing immune function and delaying healing by reducing the body’s ability to fight infections.3,4 Edible cannabis, while avoiding the harmful effects of smoke, still contains cannabinoids that may alter vascular responses and immune function, potentially interfering with the integration process and increasing the risk of complications.
SEQUELAE OF TOBACCO USE
Postoperative Complications
Smoking, vaping and cannabis use significantly impair postoperative healing following dental implant therapy by disrupting essential physiological processes involved in tissue repair and osseointegration. Nicotine and other toxic compounds induce vasoconstriction, reducing capillary blood flow and impairing oxygen and nutrient delivery to healing tissues, which diminishes angiogenesis and delays wound healing. The immunosuppressive effects of smoking and vaping further increase susceptibility to bacterial colonization, elevating the risk of post-op infection, peri-implant disease, and subsequent implant failure. Although vaping and cannabis are often perceived as less harmful alternatives to tobacco smoking, they still expose oral tissues to cytotoxic chemicals such as formaldehyde and acrolein, which contribute to oxidative stress, inflammation, and DNA damage, further delaying healing (Fig. 2).
Increased Risk of Infection
Tobacco products and cannabis result in suppression of the immune system as the function of neutrophils (white blood cells) is impaired and the production of antibodies is reduced. Therefore, a decrease in chemotactic response, phagocytic activity, and the ability to produce antimicrobial agents will result, which significantly weakens the host defense against opportunistic pathogens. In addition, the oral and systemic biome is altered, leading to an increase in harmful bacteria. This results in patients having a decreased ability to combat pathogens, and the impaired immune response may result in an increased susceptibility to post-op infections, peri-implantitis, and implant and graft failure.
Peri-implantitis
Several studies confirm a direct relationship between the use of tobacco products and peri-implantitis by increasing bacterial colonization. The resultant inflammatory and impaired immune responses reduce the immune cellular activity and exacerbate peri-implantitis. Research has shown that the prevalence of peri-implantitis is higher in smokers (26%) compared to non-smokers (12%). Additionally, studies on marginal bone loss indicate greater bone loss in smokers (2.5 mm) than in non-smokers (1.1 mm).5
Increased Implant Failure Rate
Recent meta-analyses and systematic reviews have reported a significantly higher risk of implant failure in smokers compared to non-smokers. A Medicina (Kaunas) study published in 2021 reported that implants placed in smokers had a 140% higher risk of failure than those placed in non-smokers, with a failure odds ratio of 2.4 for smokers.6 Similarly, a study published in the Annals of Palliative Medicine concluded that smoking patients have a 40% higher probability of implant failure compared to non-smoking patients (Fig. 3).7
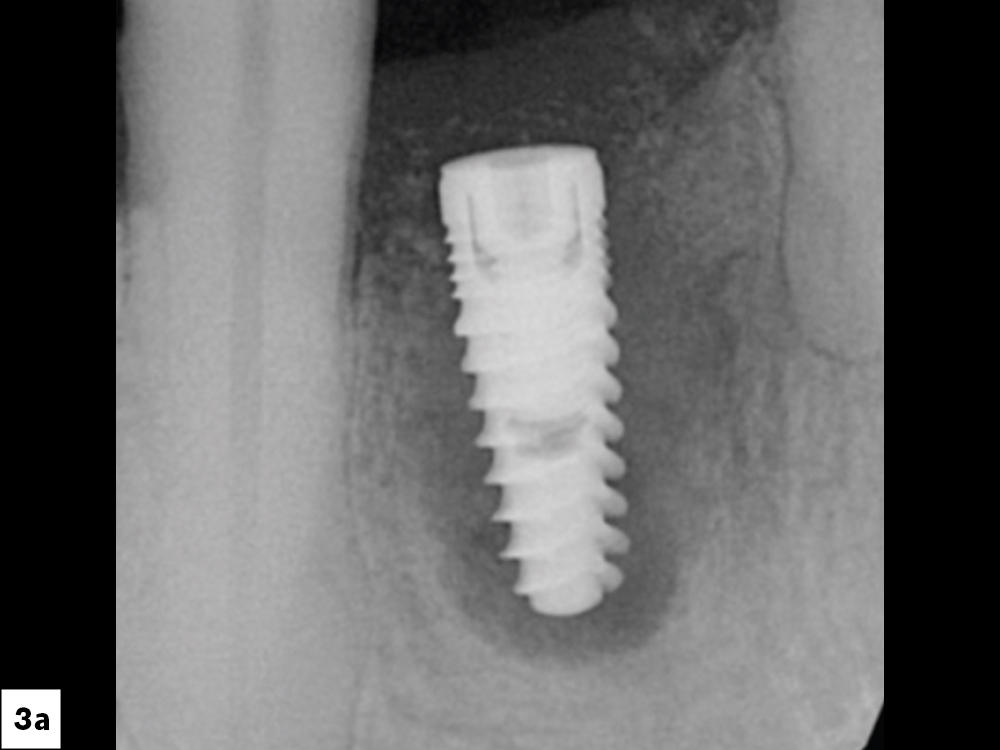
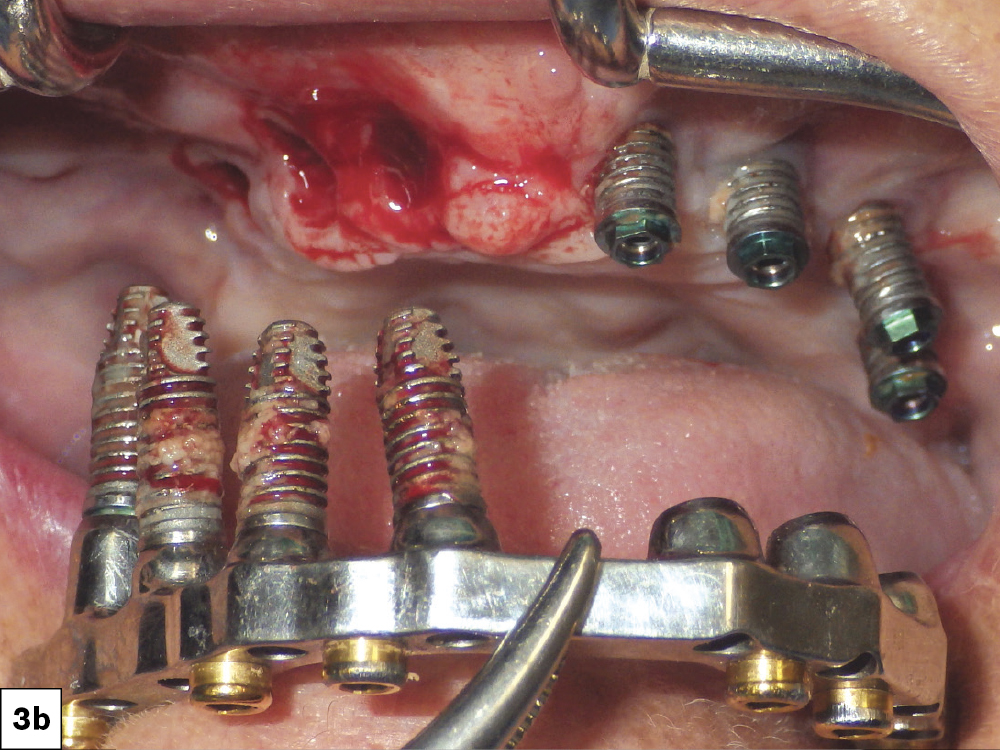
Figures 3a, 3b: Implant failures associated with tobacco use.
Increased Bone Graft Failure
Studies have shown a direct correlation between tobacco use and bone graft failure. A comprehensive meta-analysis reported smokers have a significantly higher failure rate of bone grafts compared to non-smokers. The odds ratio (OR) for graft failure in smokers was found to be approximately 2.5 times higher than that of non-smokers. A study published in Calcified Tissue International concluded that smoking significantly reduces bone mineral density and compromises the bone healing process, leading to higher rates of bone graft failure.8 Additionally, a study from the Journal of International Society of Preventive and Community Dentistry reported that implants placed in grafted maxillary sinuses of smokers have a failure rate twice that of non-smokers.9
STRATEGIES TO MITIGATE RISKS IN PATIENTS USING TOBACCO OR CANNABIS
Patient Education
Clinicians have an ethical responsibility to educate potential dental implant patients about the risks associated with tobacco and cannabis use. Given the substantial risks that these products pose to dental implant and bone grafting success, it is essential for clinicians to incorporate cessation programs into the treatment planning process. Patients must be informed and advised of the potential complications and possible remediation treatment. A benefit-risk profile should be individualized for the patient’s history and specific procedure. Clinicians should document in the patient’s chart the specifics of the patient educational process.
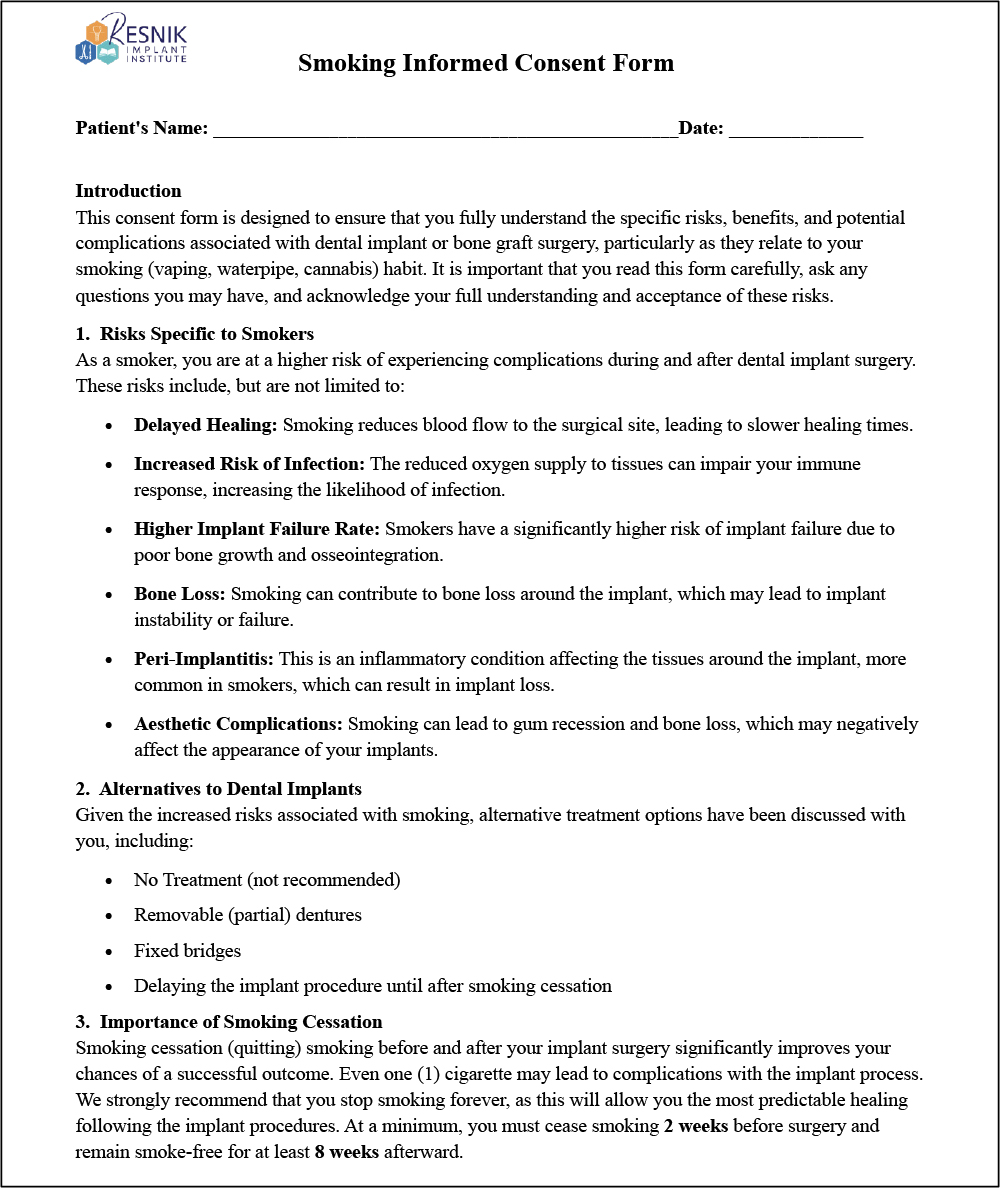
Informed Consent
Informed consent is a critical component of the preoperative treatment planning process to ensure patients understand the risks of the intended procedure. From this specific information, patients must then make an informed decision concerning the treatment. Informed consent should be provided both verbally and in writing, and clinicians should document the process in their clinical notes.
Verbal
- Specific Risks: Clearly explain the increased risks of specific complications with tobacco use, such as delayed healing, higher infection rates, and greater chances of implant failure. Patients should be well informed of how tobacco use negatively impacts bone integration and soft tissue health.
- Customized Risk Assessment: Provide the patient with a personalized assessment based on the patient’s habit history, overall health, and oral condition. A discussion on how these factors specifically affect the outcome of the implant procedure should be provided to the patient.
- Independent Witness Presence: Ideally, a witness (staff member) should be present and document that the patient was fully informed and voluntarily agreed to the treatment.
Written
A comprehensive written consent form should be obtained, explicitly detailing the specific risks that tobacco and cannabis pose to the dental implant process. This document must clearly outline the potential complications associated with these products, including impaired osseointegration, increased risk of implant failure, and delayed healing. To ensure informed decision making, patients must review and sign the consent form (documenting patient acknowledgment) prior to the scheduled procedure. This process allows sufficient time for the patient to fully comprehend the associated risks and obtain clarification on any concerns (Fig. 4).
Smoking Cessation
Ideally, patients should have complete cessation prior to dental implant procedures to avoid the above-mentioned complications as well as systemic issues. For patients who are unable to discontinue use of these products, alternative strategies may be considered, such as reduced consumption or the use of nicotine replacement therapies to minimize the harmful effects on bone healing.
Patient education should also focus on the long-term benefits of cessation, not only for the success of the implant procedures, but also for overall health. Providing patients with resources for smoking cessation, such as referrals to support programs or to their physician for nicotine replacement therapy, are crucial for increasing the possibility of smoking cessation.
In some cases, patients may agree to modify their tobacco use but decline complete cessation. In these situations, the following protocol should be followed:
Minimum Cessation Period
Preoperative: Cease smoking approximately 1–2 weeks prior to surgery. This preoperative cessation allows for reversal of the increased levels of platelet adhesion and blood viscosity, as well as the short-term negative effects associated with nicotine and byproducts.
Postoperative: Discontinue the use of tobacco for at least 2 months after implant placement, by which time bone healing would have progressed to the osteoblastic phase and early osseointegration would have been initiated.
Vaping Caution
Although vaping may involve lower nicotine levels than cigarettes, frequent use and high-nicotine liquids can match or exceed the harm caused by smoking. The thermal byproducts from vaping also introduce cytotoxic agents that impair hard-tissue and soft-tissue healing. Educating patients about these risks is essential, particularly for those who use vaping as a perceived “safer” alternative.
CONCLUSION
The use of tobacco products — including cigarettes, cigars, vaping, waterpipes and cannabis — poses significant risks to the success of dental implants and bone grafts. Clinicians must adopt comprehensive strategies to mitigate these risks, including patient education, informed consent, and evidence-based treatment protocols. By addressing the challenges posed by these products, clinicians can optimize outcomes while fulfilling their ethical and medicolegal obligations.
Available CE Course
References
-
Chang CJ, Jou IM, Wu TT, Su FC, Tai TW. Cigarette smoke inhalation impairs angiogenesis in early bone healing processes and delays fracture union. Bone Joint Res. 2020 May 16;9(3):99–107.
-
Mayfield L, Söderholm G, Hallström H, Kullendorff B, Edwardsson S, Bratthall G, Brägger U, Attström R. Guided tissue regeneration for the treatment of intraosseous defects using a bioabsorbable membrane: A controlled clinical study. J Clin Periodontol. 1998 Jul;25(7):585–95.
-
Nogueira-Filho GR, Cadide T, Rosa BT, Neiva TG, Tunes R, Peruzzo D, Humberto Nociti F, César-Neto JB. Cannabis sativa smoke inhalation decreases bone filling around titanium implants: A histomorphometric study in rats. Implant Dentist. 2008 Dec;17(4):461–70.
-
Rutkowski JL. Marijuana – Clinical concerns for implant dentistry – Part 2. J Oral Implantol. 2023 Feb 1;49(1):1–2.
-
Chinnakutti S, Govind Raj S, Peter C, Shankar PR, GL G. Comparative analysis of dental implant success rates in smokers and non-smokers: A long-term follow-up research. J Chem Health Risks. 2023;13(4).
-
Mustapha AD, Salame Z, Chrcanovic BR. Smoking and dental implants: A systematic review and meta-analysis. Medicina (Kaunas). 2021 Dec 27;58(1):39.
-
Lu B, Zhang X, Liu B. A systematic review and meta-analysis on influencing factors of failure of oral implant restoration treatment. Ann Palliat Med. 2021 Dec;10(12):12664–77.
-
Shah FA, Sayardoust S, Omar O, Thomsen P, Palmquist A. Does smoking impair bone regeneration in the dental alveolar socket? Calcif Tissue Int. 2019 Dec;105(6):619–29.
-
Kasat V, Ladda R. Smoking and dental implants. J Int Soc Prev Community Dent. 2012 Jul;2(2):38–41.