Freehand Placement of Dental Implants: A Recipe for Success (1 CEU)
Dental implantology is a predictably successful treatment when the established principles are followed. Similar to a chef following a recipe, deviations from this methodology can result in lower success rates and suboptimal outcomes. In this case report, we will illustrate a set of rules and principles that together constitute a recipe for success with dental implants.
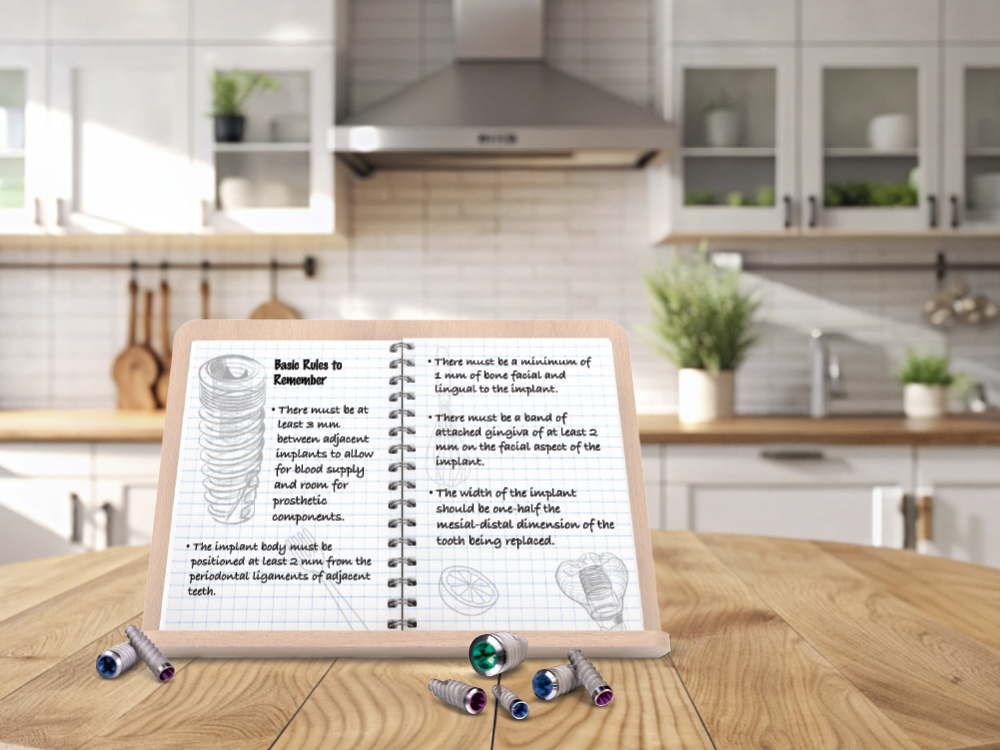
Basic Rules to Remember
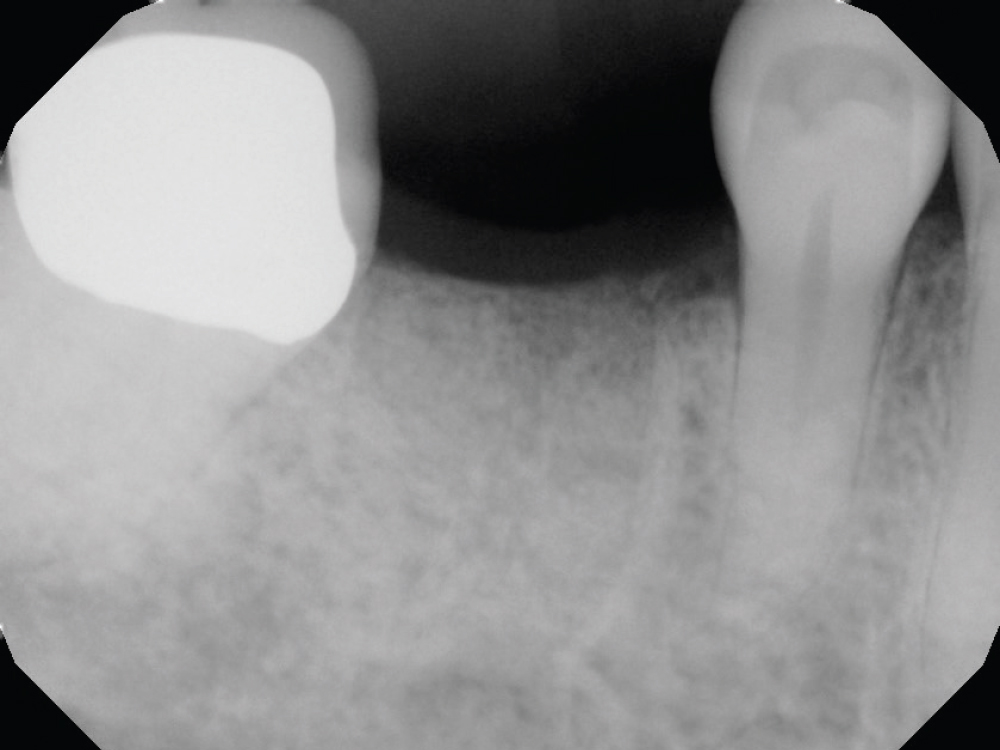
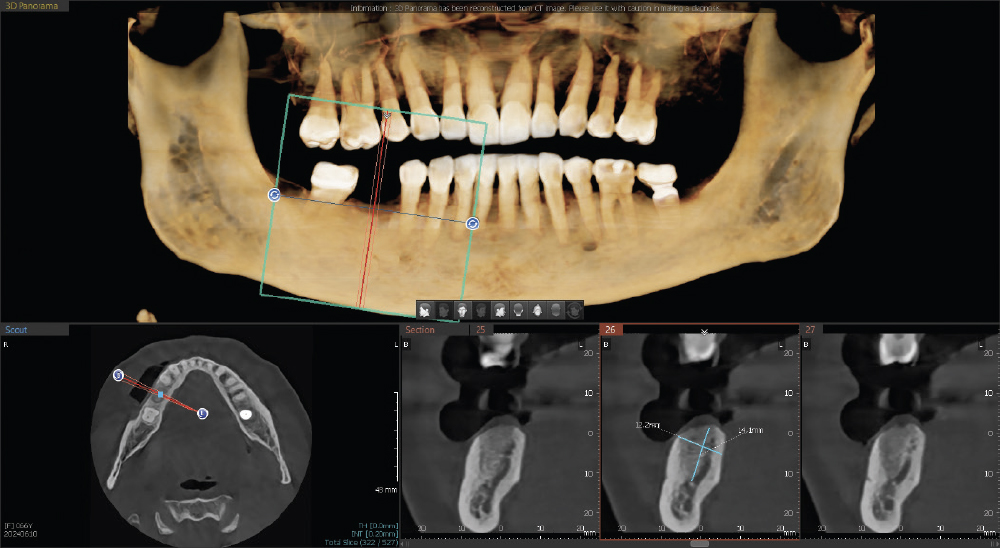
- There must be at least 3 mm between adjacent implants to allow for blood supply and room for prosthetic components.
- The implant body must be positioned at least 2 mm from the periodontal ligaments of adjacent teeth.
- There must be a minimum of 1 mm of bone facial and lingual to the implant.
- There must be a band of attached gingiva of at least 2 mm on the facial aspect of the implant.
- The width of the implant should be one-half the mesial-distal dimension of the tooth being replaced.
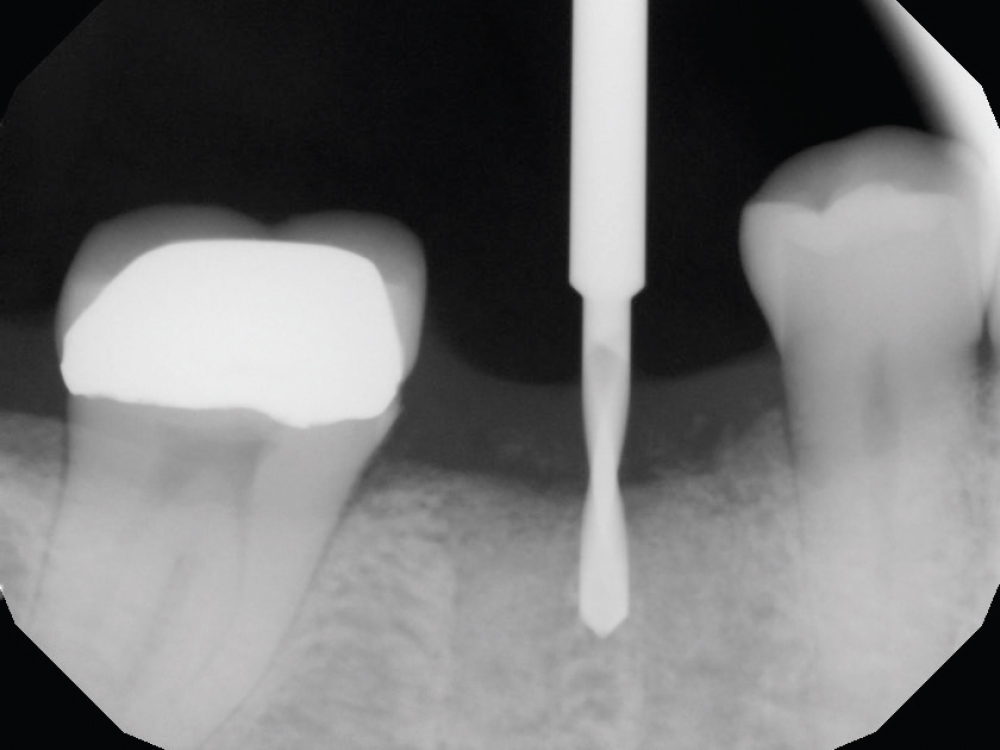
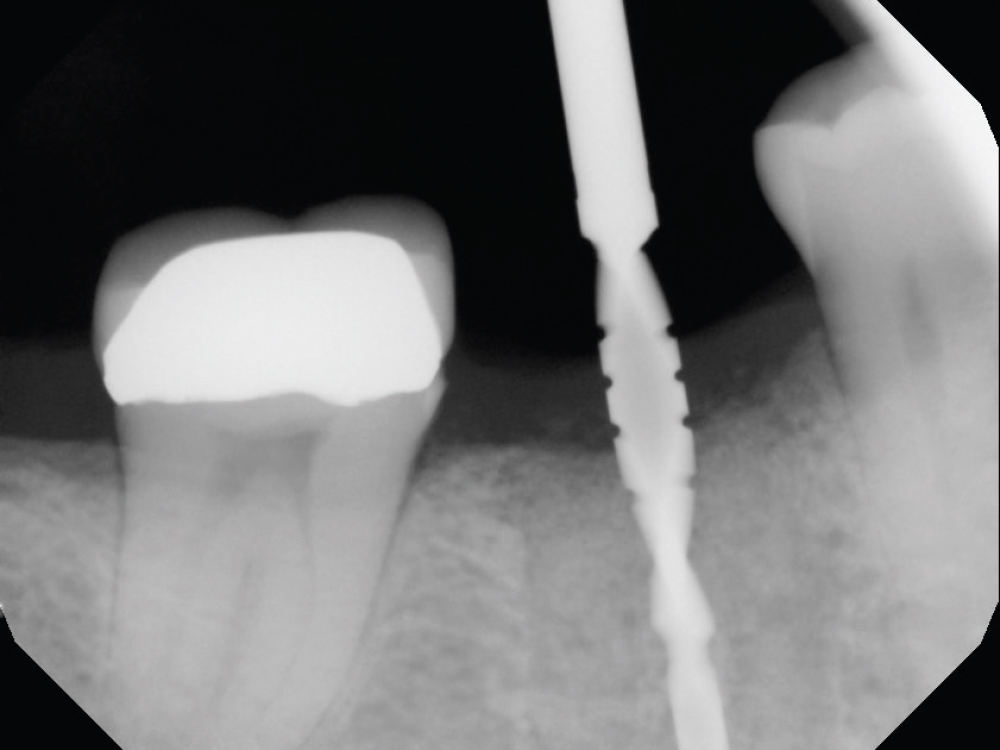
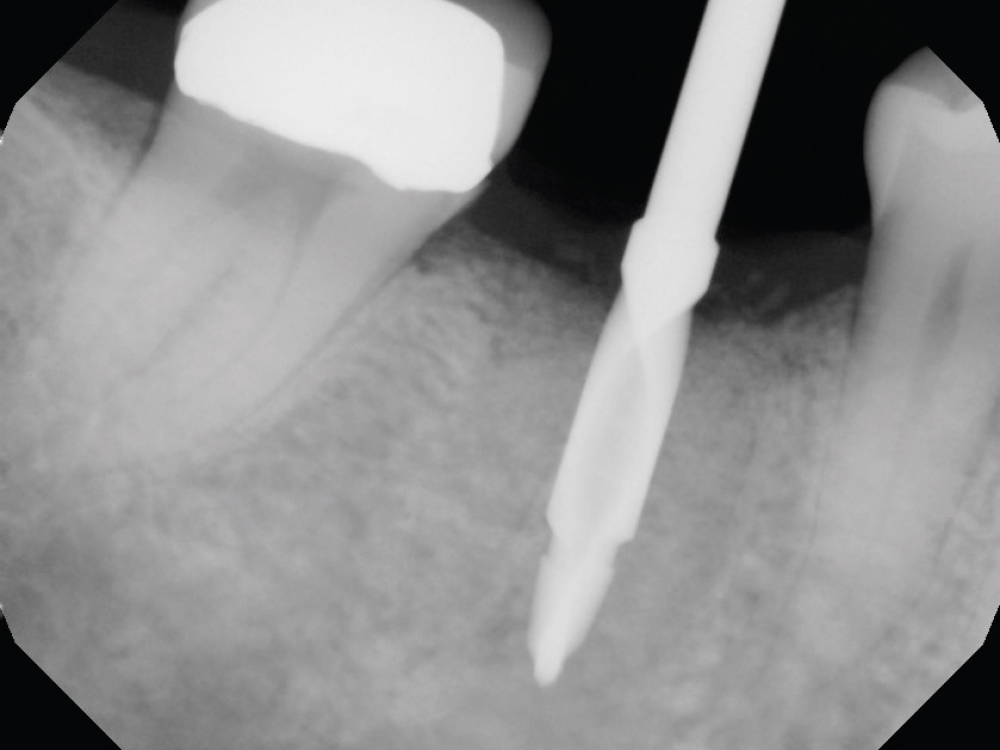
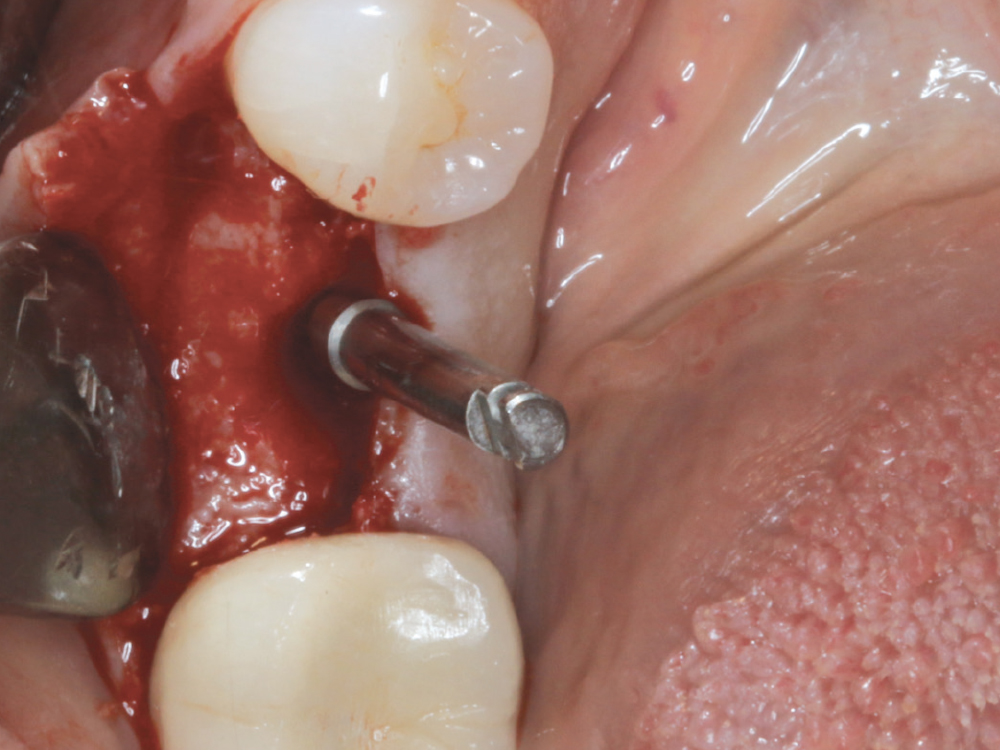
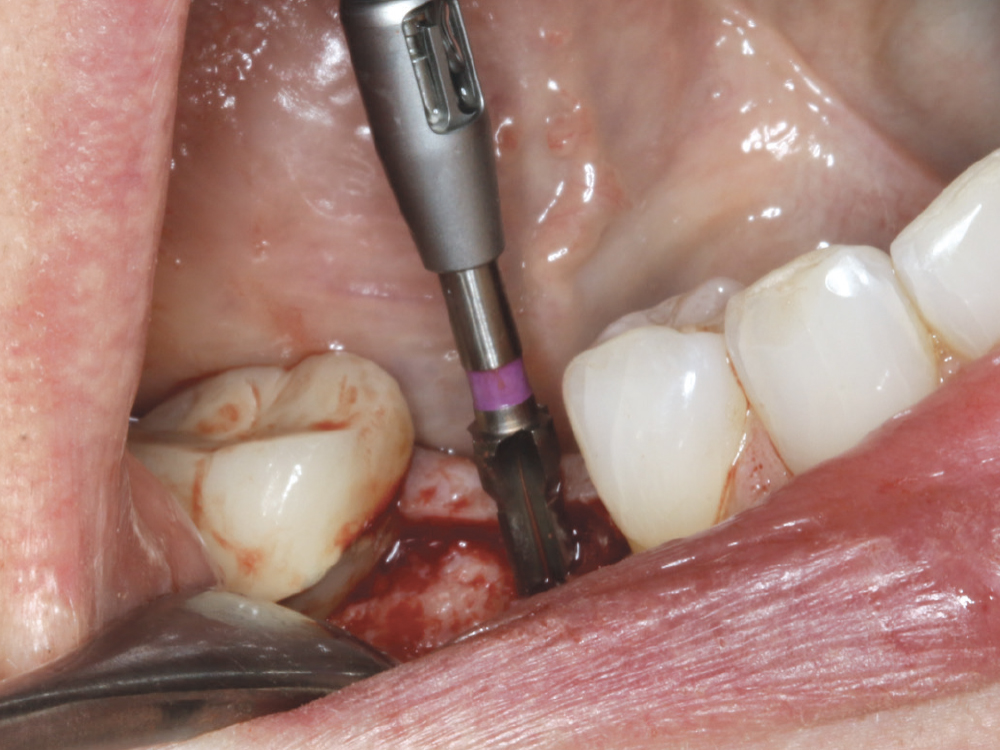
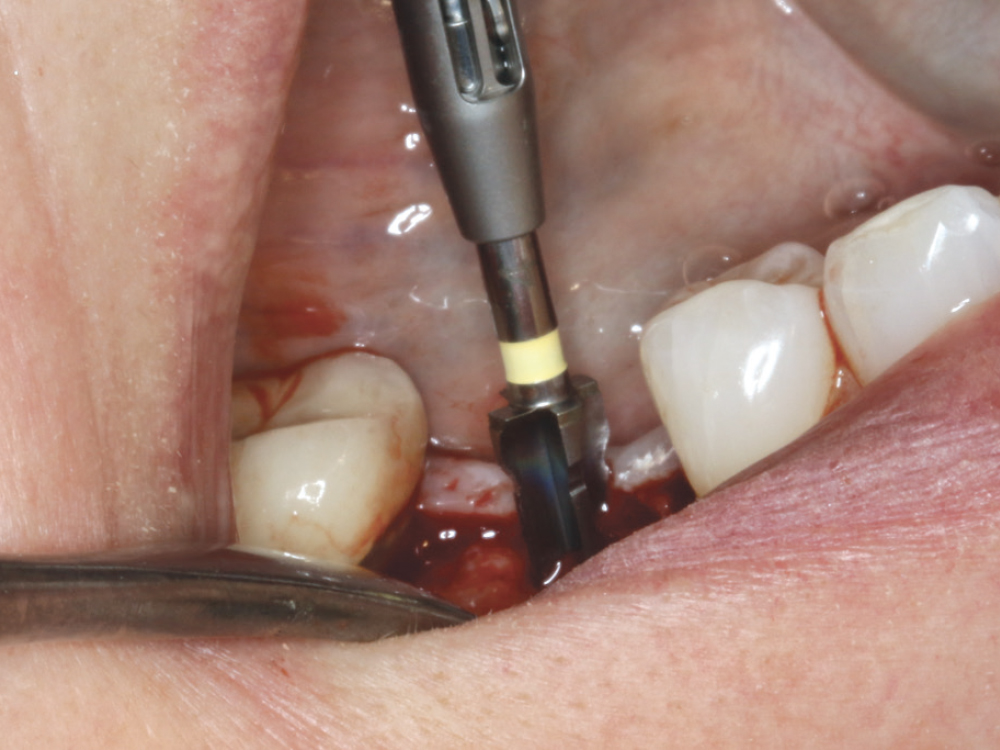
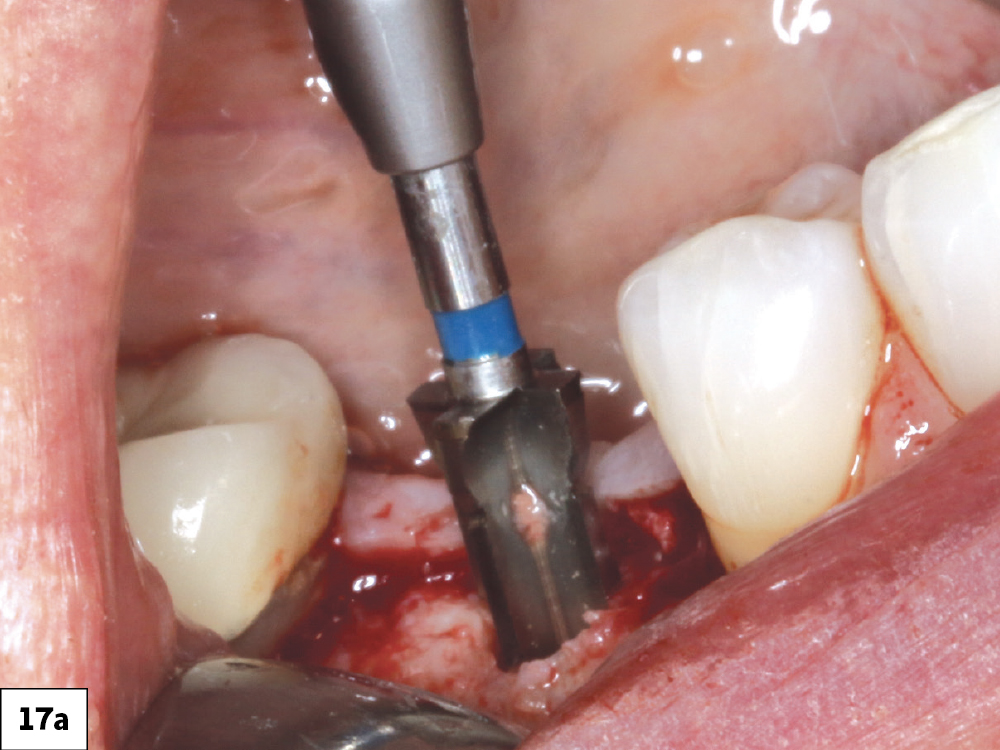
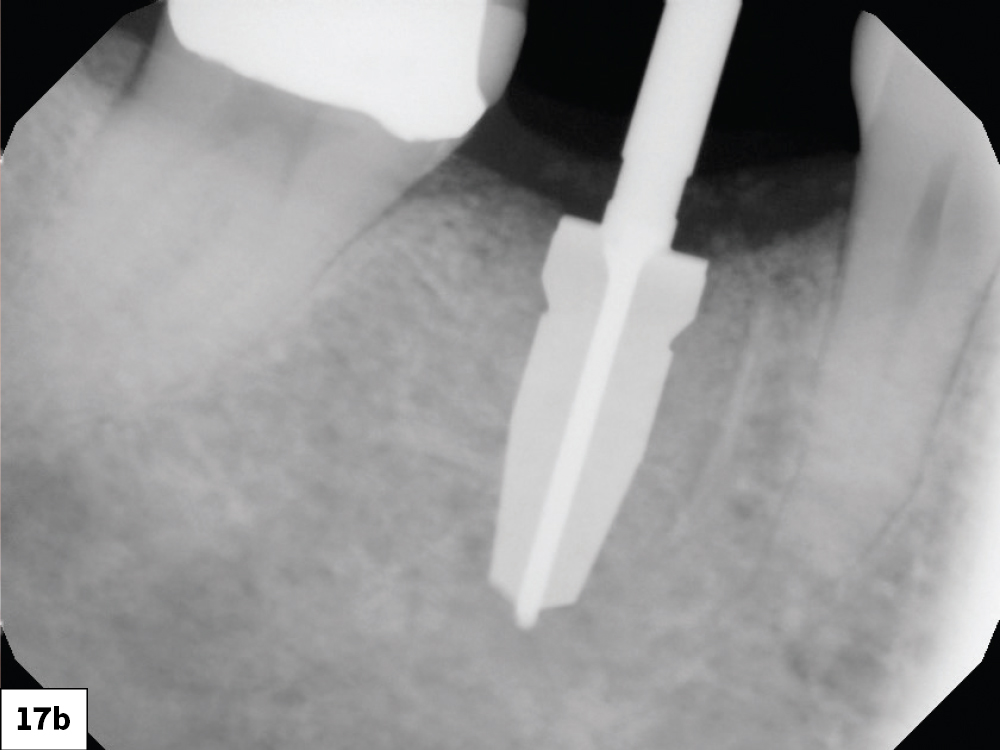
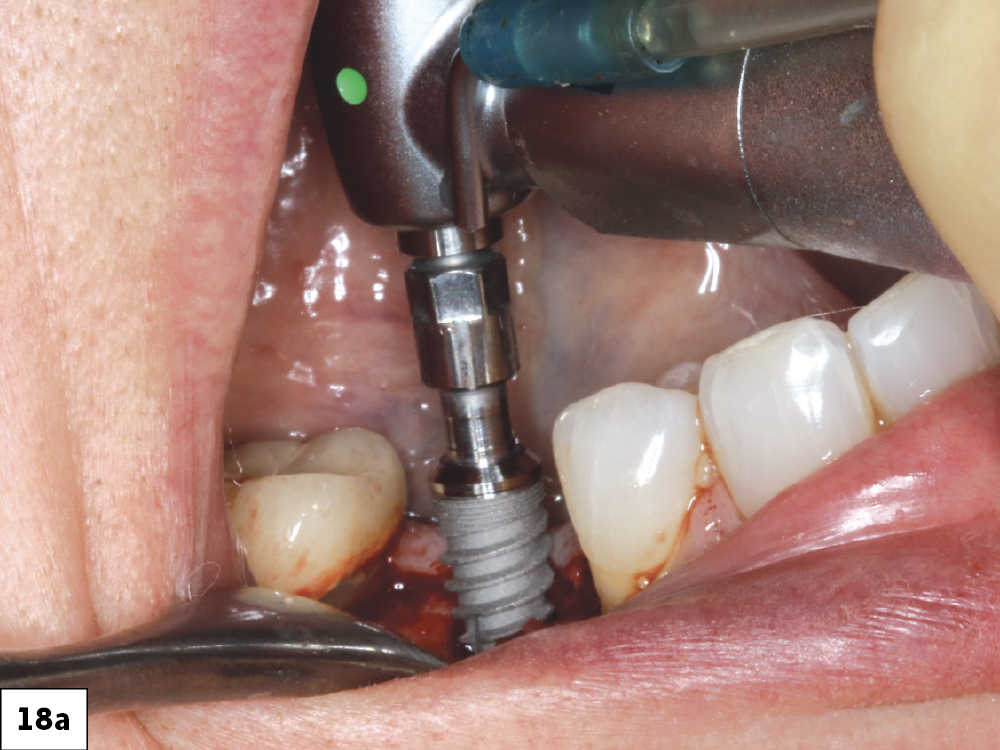
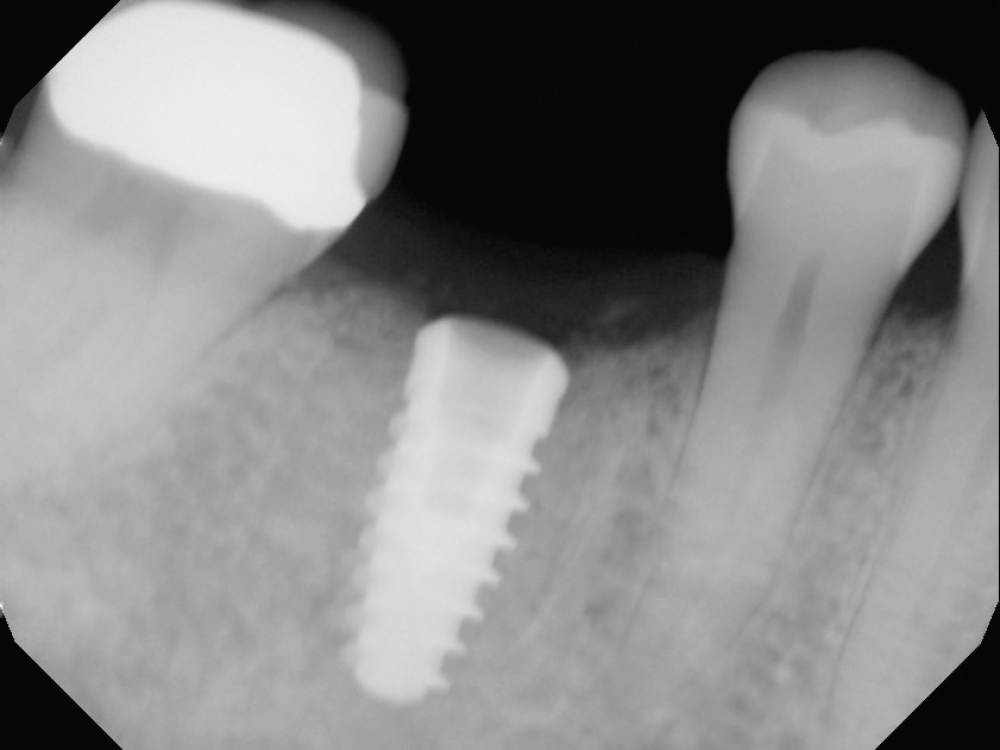
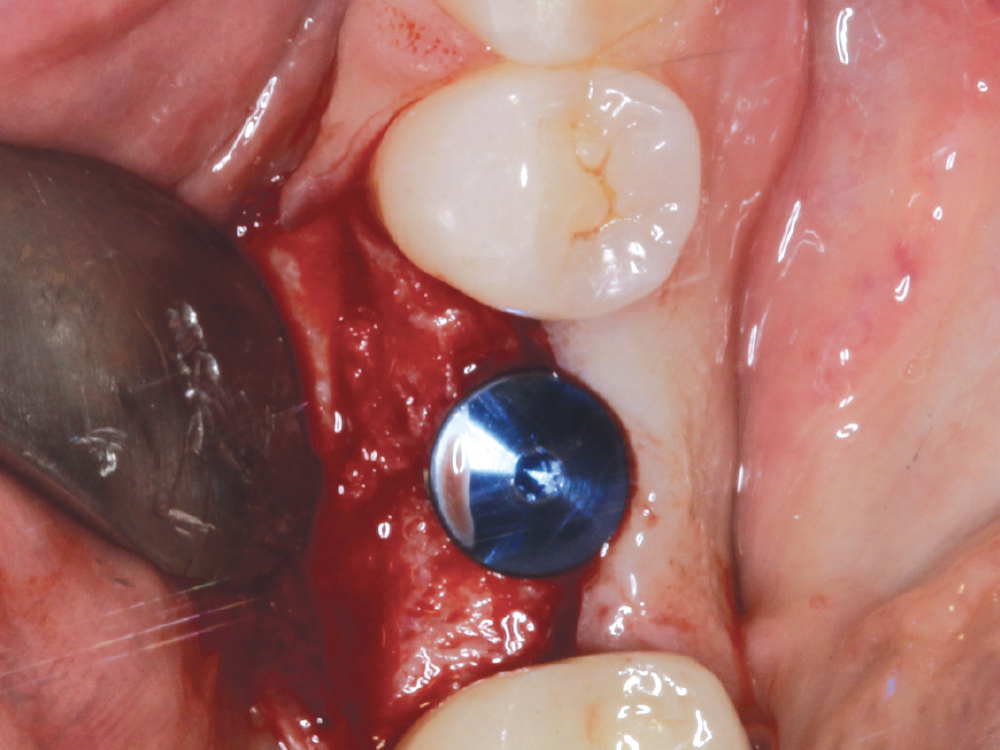
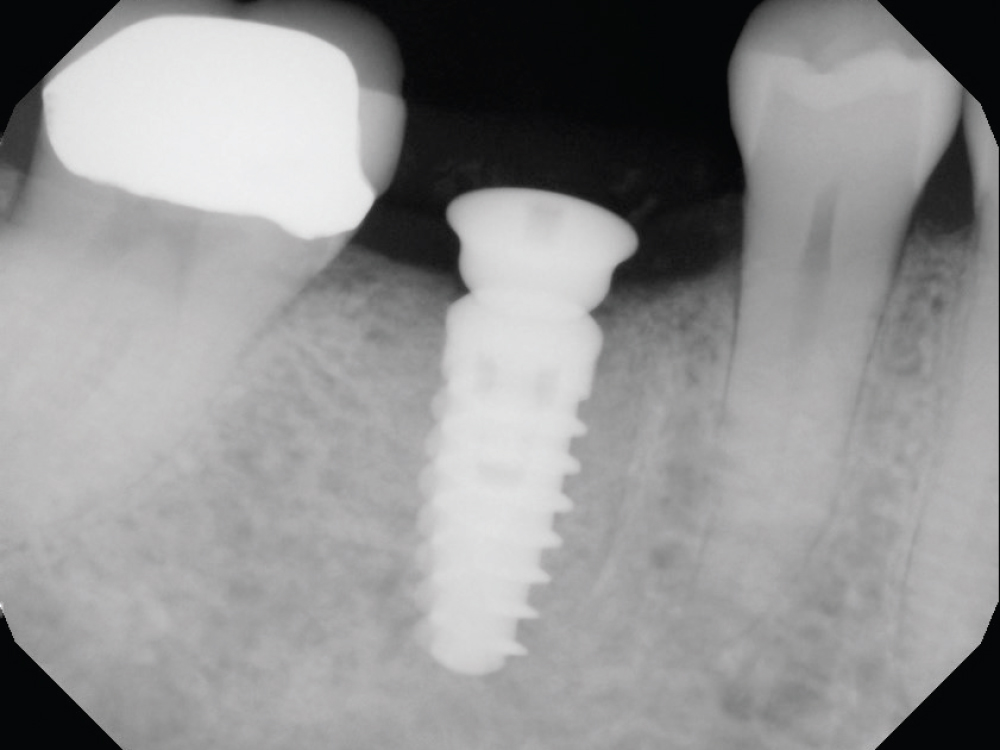
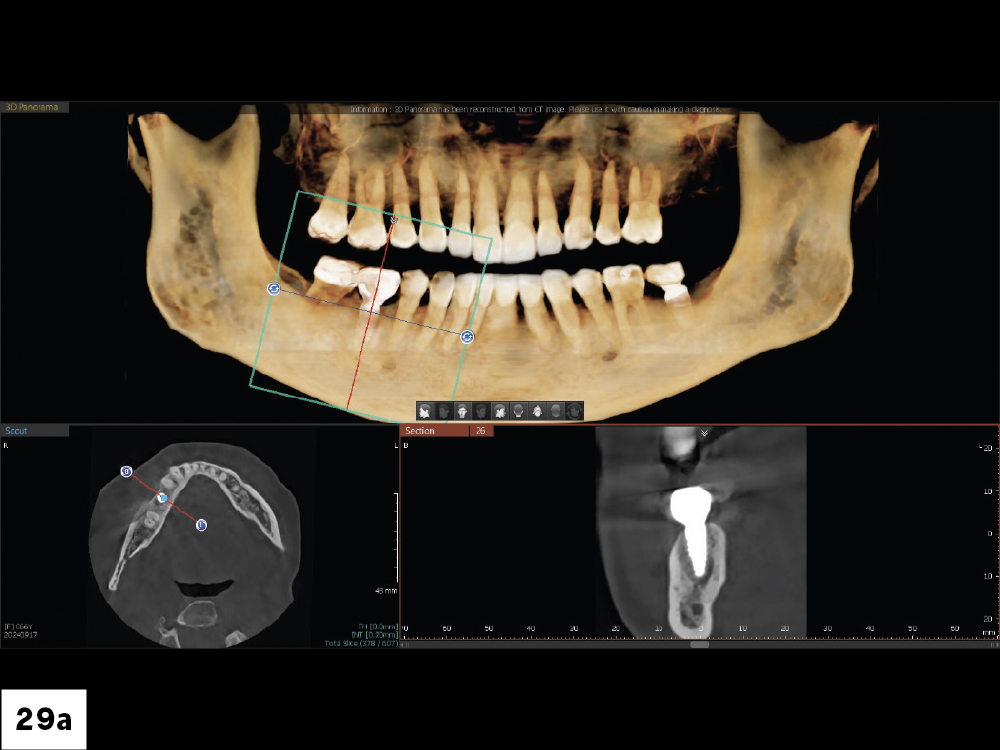
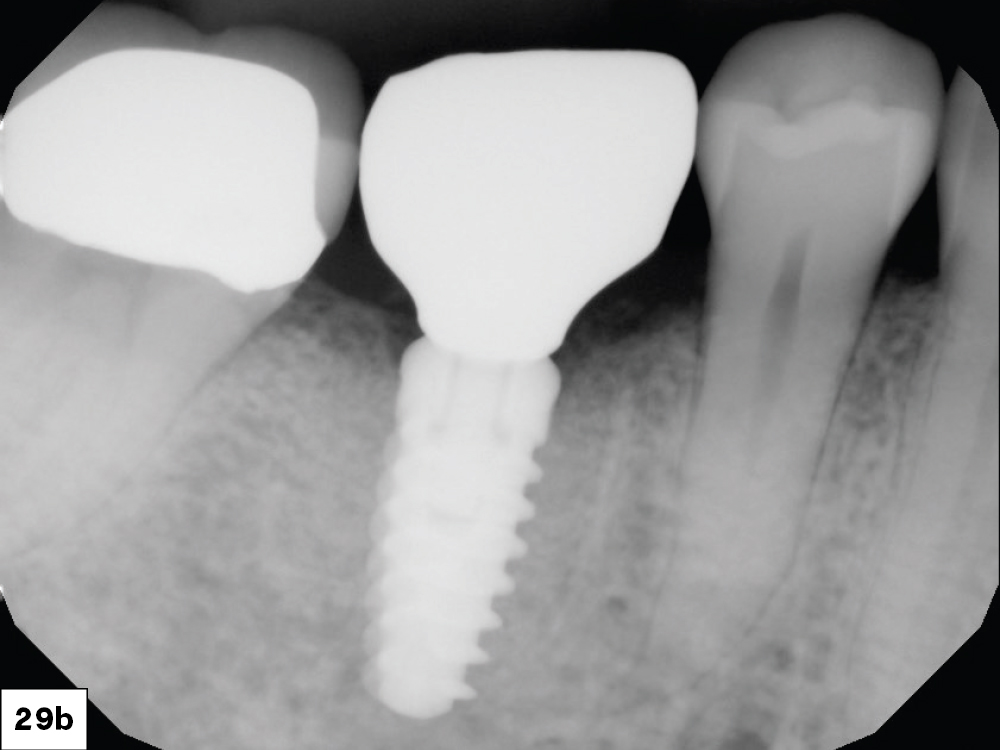
Case Report
CONCLUSION
Following a proven recipe results in higher levels of treatment success. Taking a “crown-down” approach by imagining the final restoration in place helps the practitioner determine implant placement and maximize osteotomy design and emergence profile. The recipe for success includes verifying each step along the way with the ideal end result in mind.
Available CE Course