Photo Essay: Utilizing No-Prep Veneers with Zirconia Crowns to Complete a Smile
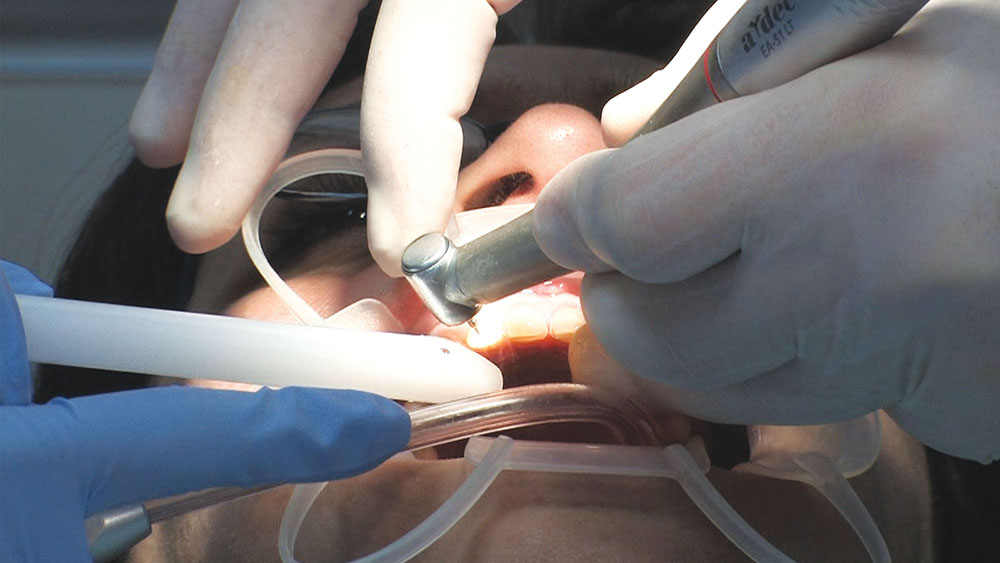
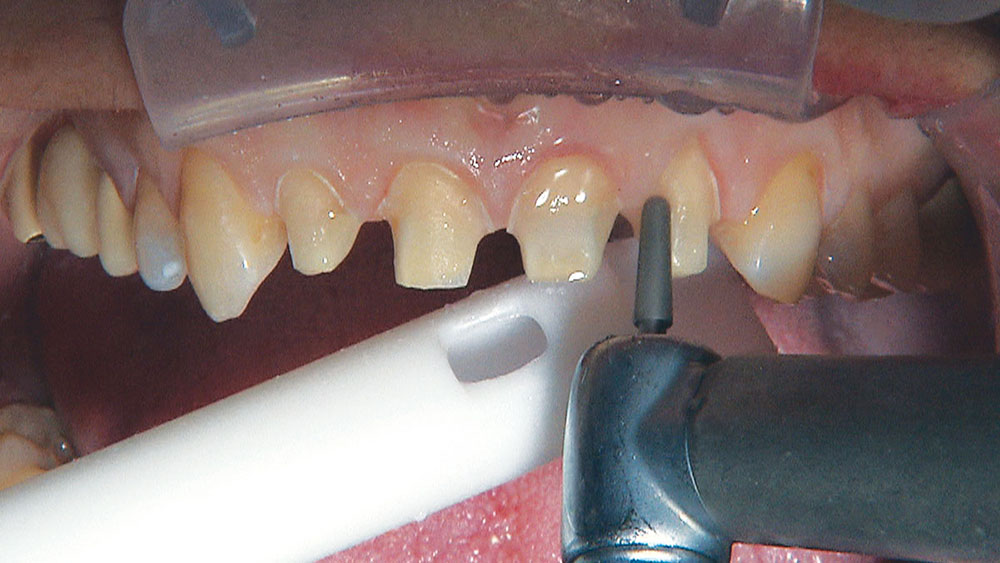
These maxillary anterior infiltrations can be exquisitely sensitive for many patients, so I just talk to my assistant to distract the patient, and let the computer do its thing.
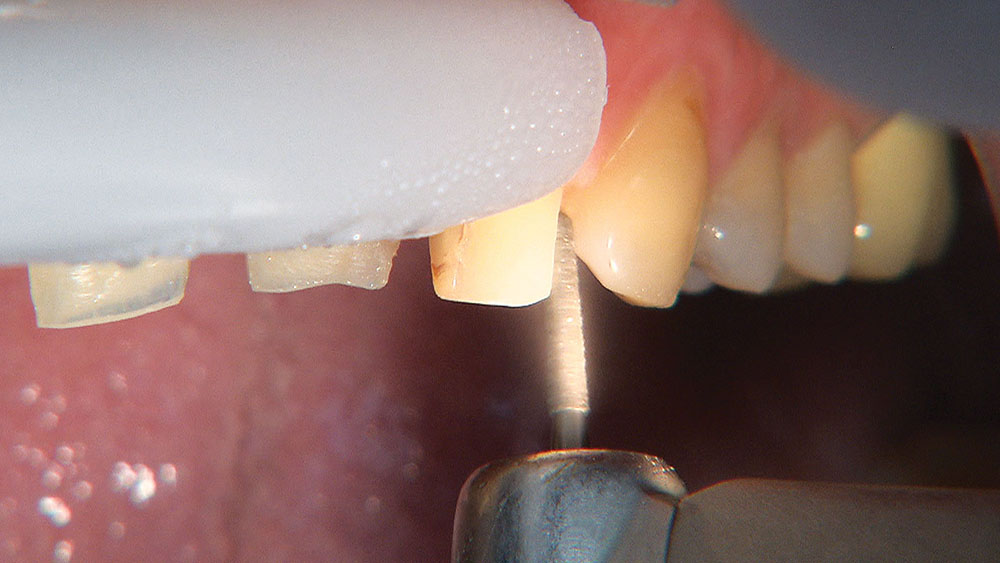
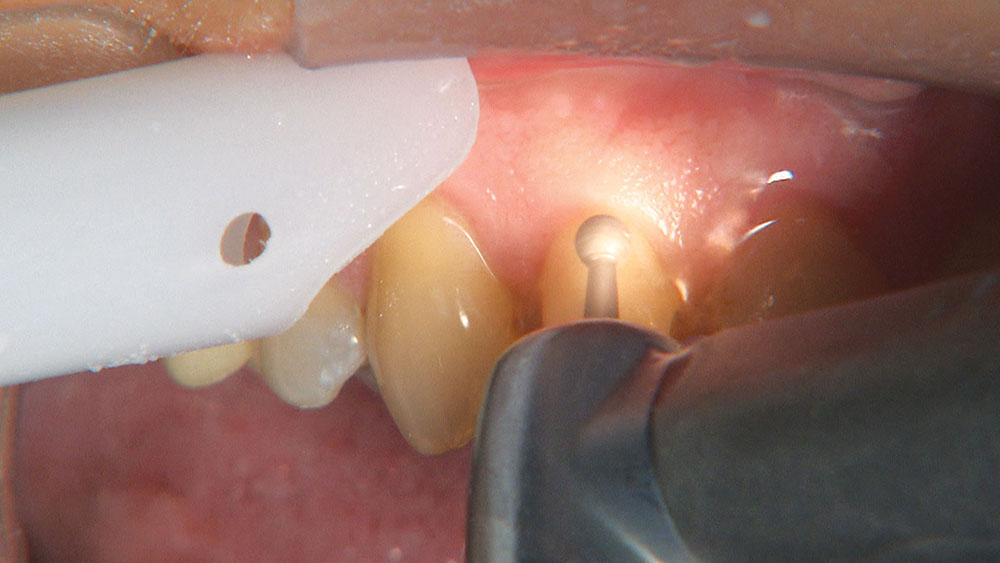
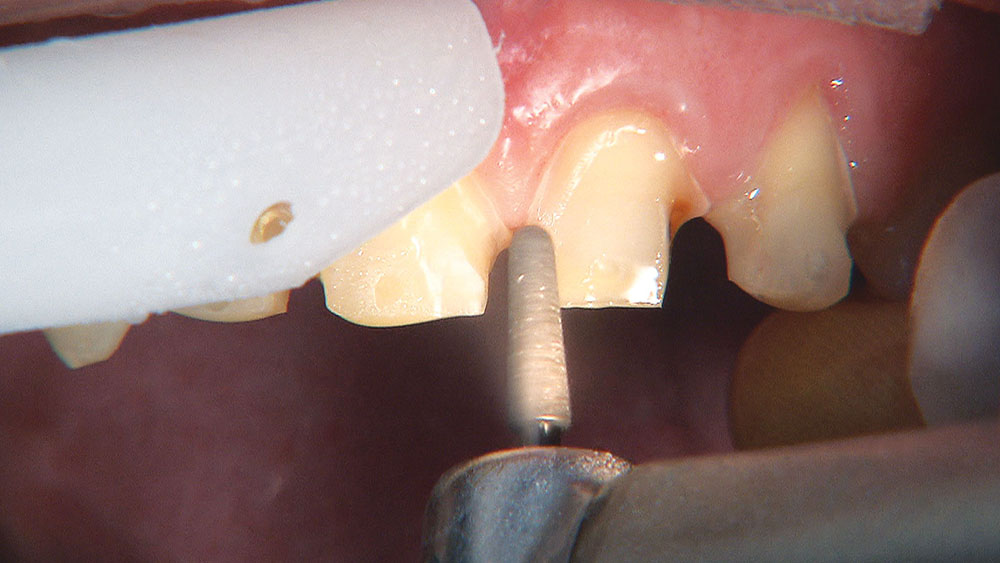
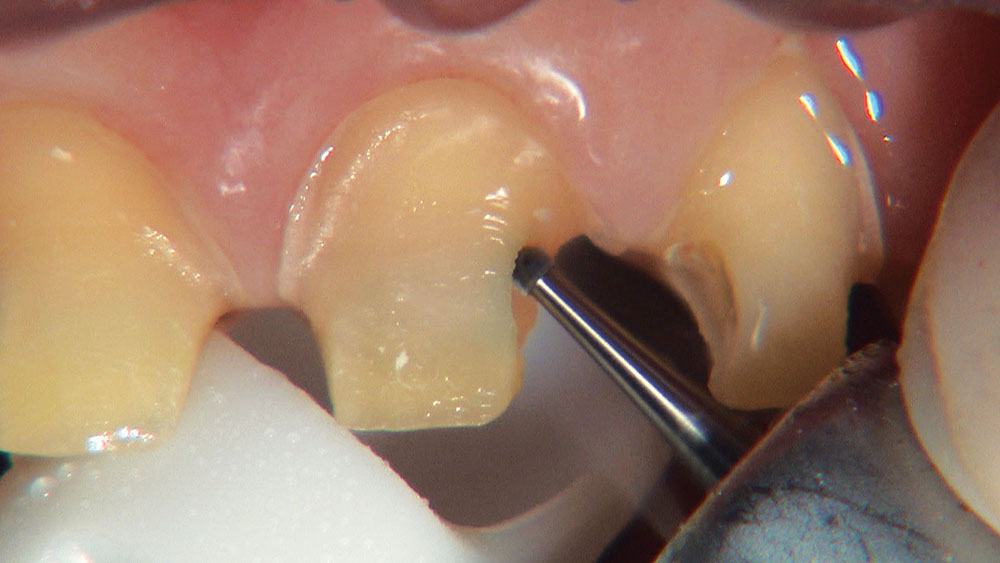
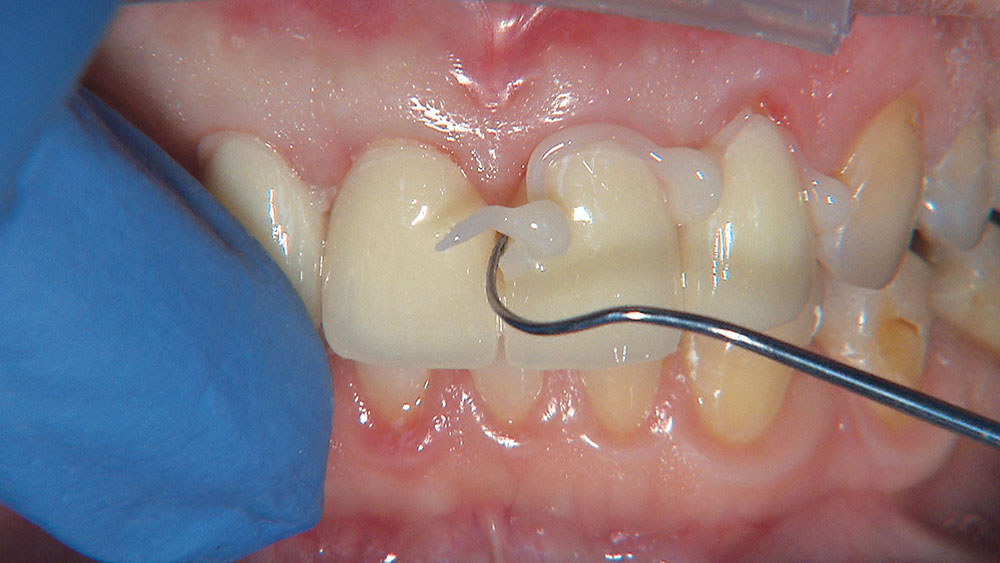
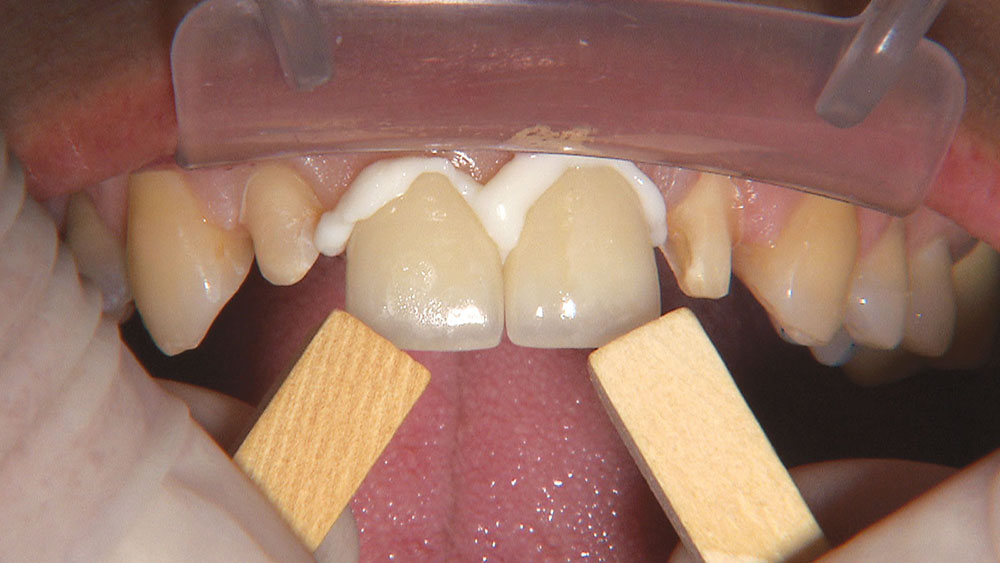
The first thing I want to do is confirm that I have a passive fit of the BioTemps.
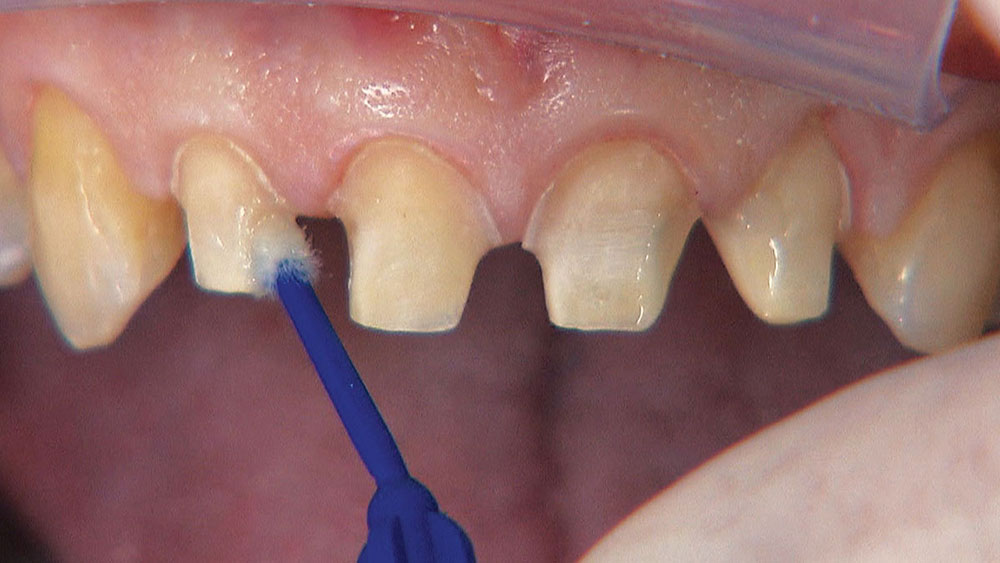
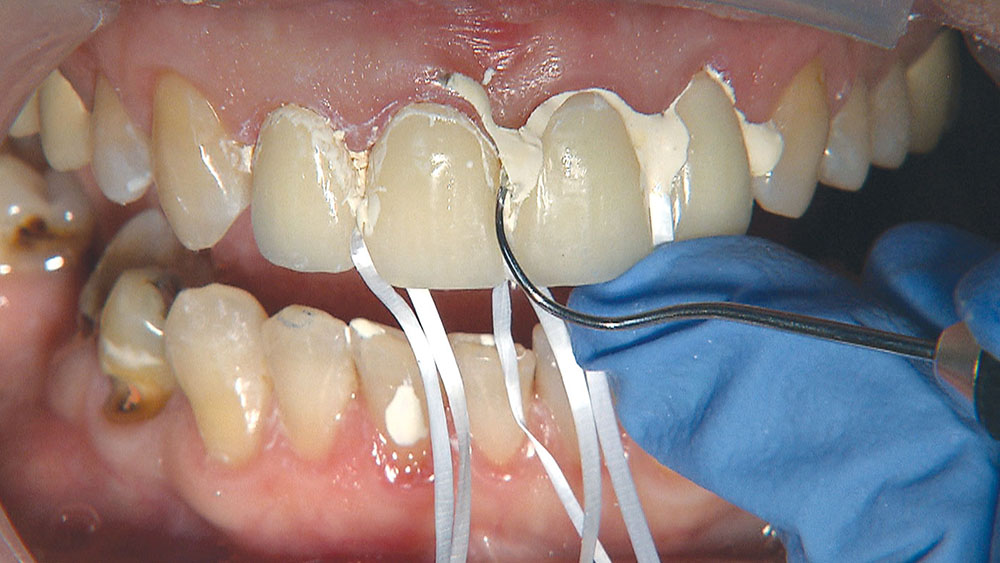
Because the central incisors essentially can make or break the smile, I prefer not to have to deal with the lateral incisors or any possible contact issues.