Implant Treatment for Older Patients (1 CEU)

Implant treatment is implant treatment, no matter the age of the patient. Right? Wrong, especially when treating older patients. Older patients require unique precautions and treatment modifications, due to the normal changes associated with aging as well as common systemic diseases and the medications used in their treatment.
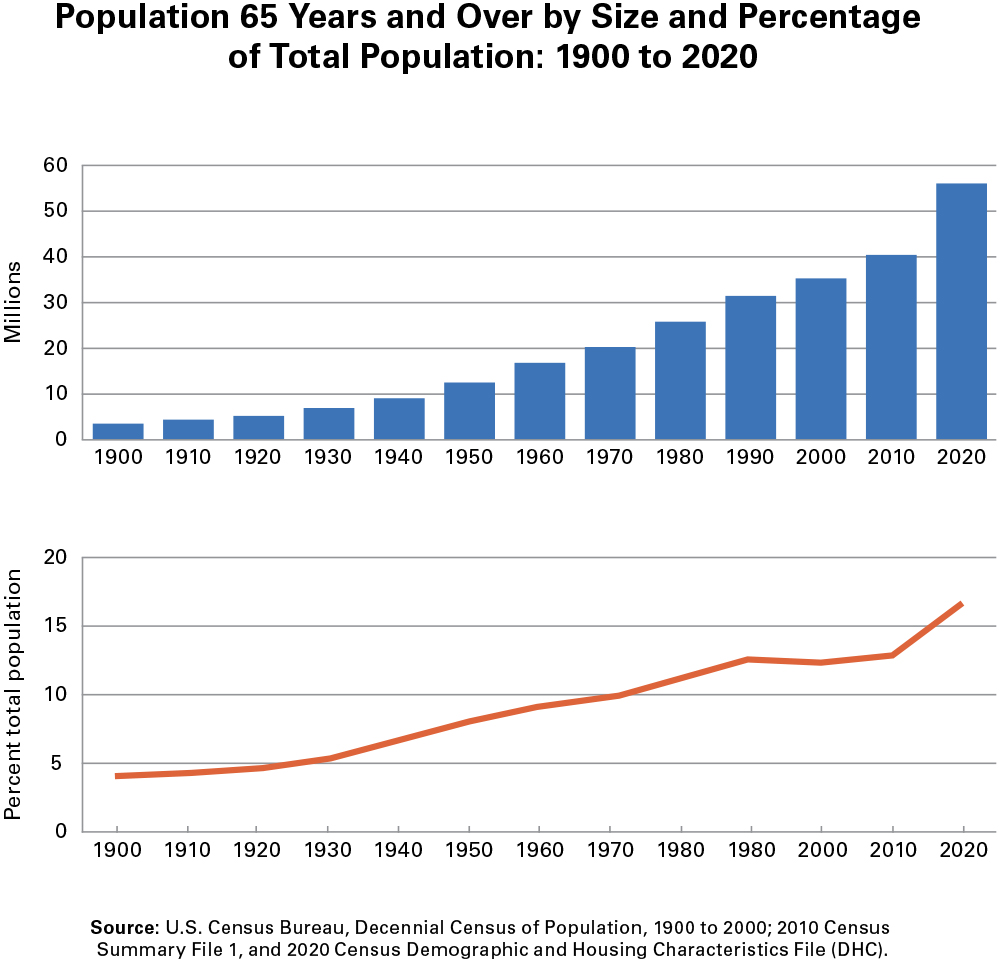
In the coming years, the segment of the population 65 years of age and older will continue to grow and will comprise the largest pool of candidates for implant treatment, making this a high-priority demographic for all dentists. Understanding how to treat seniors, and why they deserve priority, is crucial for successful dental practices in the coming years.
As a clinician in private practice for 35 years, I realized that my patients are getting older with me. And as these patients get older, much has changed for them regarding their health.
Studies show my experiences are reflective of a much larger global shift. A National Institute on Aging and National Institutes of Health (NIH) study estimated the worldwide population of people 65 and older would triple from 2010 to 2050 to make up a remarkable 1 in 5 of the entire populace.1
Consider these numbers a wake-up call to our profession. An increase in older patients seeking implant treatment is a virtual certainty based solely on the aging of the overall population. And there is no patient group where the connection between oral health and overall well-being is more important than among older adults.
IMPLANTS AS PREVENTIVE HEALTHCARE
Studies suggest that poor oral health may be closely related to the development of diabetes, cognitive impairment and overall longevity.2
Having fewer natural teeth has been associated with diminished chewing capacity, as well as a reduced quality of life. In fact, one study found an association between reduced longevity and tooth loss.3 Similarly, studies have demonstrated parallel trends between tooth loss and increased risk of cognitive impairment. One such report found seniors with multiple missing teeth having a 55% higher risk of developing dementia.4
We are also seeing potential positive preventive results with periodontal treatment and diabetes, as shown by hemoglobin A1C [HbA1c] levels.5 The more correlations found between dental health and prevention of ailments that impact seniors, like dementia and diabetes, the more attractive implant treatment will be for this age group.
WHAT YOU NEED TO KNOW
Geriatric dentistry aims to provide evidence-supported methods of dental treatment for seniors with systemic and cognitive limitations. All dentists should consider the following factors when treating older patients.
UNDERSTANDING PATIENTS’ MEDICATIONS
Knowing a patient’s complete health history and pharmaceutical regimen is crucial. Open lines of communication are vital, particularly with patients who may see multiple specialists who prescribe different medications.
Whenever we perform surgery, including implant surgery, we must be able to navigate all the patients’ prescriptions to prevent adverse reactions and drug interactions. The following are common medications prescribed for older adults that can affect implant treatment.
1. Proton pump inhibitors (PPIs)
PPIs are prescribed for gastric acid suppression for the treatment of acid-related problems such as gastroesophageal reflux disease (GERD).6 PPIs reduce calcium availability by increasing the pH in the small intestine.7,8 This results in a negative calcium balance that leads to accelerated bone mineral loss, and could eventually affect bone health and the osseointegration of dental implants.8
Use of PPIs increases with age, with over 30% of persons over 80 years of age taking PPIs for more than one year.6 A large, retrospective study9 that found a higher implant failure rate for PPI users, with 6.8% failure in PPI users compared to 3.2% failure in non-PPI users.
Determining if an implant patient needs to be on a PPI is the first step in mitigating possible failure associated with using these medications. Review why the patient is taking a PPI, for how long, and how recently the prescribing physician updated the recommendation.
2. Antidepressants
Although actual mechanism of action of commonly prescribed antidepressants, such as selective serotonin reuptake inhibitors (SSRI) and serotonin and norepinephrine reuptake inhibitors (SNRI) on bone tissue is not completely understood, several studies have reported the detrimental impact of SNRIs on bone metabolism.10,11
A retrospective study12 of 771 patients found patients on antidepressants experienced implant failure rates exceeding 30%, while those not taking antidepressants experienced a 5.2% failure rate.
Increasing awareness about the possibility for implant failure among patients taking antidepressants is important as we continue to learn more. Dentists should be proactive in communicating this possibility both with the patient and the prescribing physician.
3. Anticoagulants
These are commonly prescribed for older adults with cardiovascular conditions. Besides Coumadin, novel oral anticoagulants (NOAC) such as Eliquis®, Xarelto® and Pradaxa® are increasingly prescribed by physicians in recent years because they reduce the need for constant monitoring, have fewer interactions with other medications, and have more rapid onset (2–5 hours) and offset (5–17 hours).
For any implant surgical procedure, medical consultation is essential before interrupting the medication. Typically, the physician will not interrupt the use of anticoagulants, in which case you will want to perform a minimally invasive procedure and other modalities that result in as little bleeding as possible. The least invasive surgery possible in these cases is best for patients on anticoagulants.
MEDICATION-CAUSED DROWSINESS, FATIGUE OR LOSS OF BALANCE
There are also many categories of medications common among seniors that can cause drowsiness, fatigue or a loss-of-balance. Fall prevention is vital when treating patients who are taking these medications.
A serious fall can be devastating to an older patient. Ensure all staff recognizes the seriousness of preventing falls, which can be as simple as someone being assigned to walk patients to and from their transportation. Be sure that your facility is optimized for these patients with good lighting and seamless flooring to prevent tripping.
DRY MOUTH DUE TO MEDICATION
Over 700 medications are known to cause different degrees of xerostomia, including antihypertensives, antidepressants, antipsychotics, antihistamines and sedatives.
Diminished lubrication from saliva can lead to food impaction around teeth and prostheses, contributing to a higher rate of caries and periodontal disease. If a patient presents with severe dry mouth, aggressive home-care monitoring is crucial. Proactive measures like hydration, specially designed oral rinses, and sugar-free chewing gum may be recommended to mitigate the complications.
STRESS REDUCTION
Although older adults may appear healthy, they do not have the same functional reserve to handle stress as younger adults. Routine dental procedures may be a source of excessive stress for some older adults.
Stress in older adults can lead to unexpected cardiovascular events. Minimally invasive surgical techniques should be considered to minimize trauma and reduce the risk of postoperative complications.
IMPLANT SURGICAL CONSIDERATIONS
- If the patient has type 2 diabetes, prevent hypoglycemic and hyperglycemic events by ensuring that patient had adequate food intake and anti-diabetic medications before starting the surgery; have a glucose source available chairside.
- Monitor vital signs throughout treatment.
- Administer excellent and profound local anesthesia to reduce anxiety.
- Limit amount of vasoconstrictor in local anesthetic if coexisting hypertension and cardiovascular diseases are present.
- Exercise caution to prevent patient falls especially if sedation is used or if patient is subject to orthostatic hypotension due to medications.
- Schedule shorter surgical appointments, in late morning or early afternoon.
- Provide written post-op instructions and review with patient (and with driver or caregiver).
IMPLANT RESTORATIVE CONSIDERATIONS
The implant-supported prosthesis design should consider the functional and esthetic needs of older patients. Prostheses should be designed for easy maintenance to minimize discomfort and facilitate oral hygiene.
Here are recommendations for implant restorative procedures.
- Evaluate patient’s manual dexterity and home care capability before selecting the type of prosthesis.
- Select the type of prosthesis with consideration for future repair and maintenance. For example, with removable overdentures, use the simplest attachment system for ease of maintenance.
- Design fixed prostheses with retrievability (screw-retained rather than cement-retained).
- Allow a longer healing period before prosthetic loading of implants to account for slower healing.
- Keep complete records of all parts and components for future reference.
LONG-TERM HOME CARE AND MAINTENANCE CONSIDERATIONS FOR OLDER ADULTS
This is probably the most crucial phase of implant treatment for older adults since it will be increasingly more challenging to treat and manage complications as patients continue to decline.
Here are recommended suggestions for this phase of treatment:
- Keep frequent intervals for maintenance follow up visits.
- If any peri-implant problems arise, aggressively treat at early onset and closely follow up.
- Review health history at every visit and evaluate any changes in health and medications.
- At every maintenance visit, evaluate any changes in patient’s functional capacity such as activities of daily living (ADL). The beginning of decline in functional capacity generally marks the beginning of decline in home care. Involve family members or caregivers if necessary.
- Focus on patient autonomy in home care as much as possible rather than relying on caregiver or family members.
Review health history at every visit and evaluate any changes in health and medications.
CONCLUSION
The ongoing demographic shift means that seniors will make up a greater proportion of dental patients in the future. Likewise, an evolving understanding of how physical and cognitive health are connected to dental health should drive demand among seniors.
Catering to older patients is more than just smart business. Working with seniors to improve their quality of life is rewarding. However, it is essential to understand the different demands for treating older clientele compared to the younger demographic.
Available CE Course
References
-
Global Health and Aging. National Institute on Aging, National Institutes of Health, NIH Publication no. 11-7737. doi:10.1016/B978-0-12-375000-6.00006-9.
-
Wu B, Luo H, Tan C, et al. Diabetes, edentulism,
and cognitive decline: A 12-Year prospective analysis. Journal of Dental Research. 2023;102(8):879-886. doi:10.1177/00220345231155825. -
Friedman PK, Lamster IB. Tooth loss as a predictor of shortened longevity: exploring the hypothesis. Periodontol 2000. 2016 Oct;72(1):142-52. doi: 10.1111/prd.12128. PMID: 27501497.
-
Fang WL, Jiang MJ, Gu BB, Wei YM, Fan SN, Liao W, Zheng YQ, Liao SW, Xiong Y, Li Y, Xiao SH, Liu J. Tooth loss as a risk factor for dementia: systematic review and meta-analysis of 21 observational studies. BMC Psychiatry. 2018 Oct 20;18(1):345. doi: 10.1186/s12888-018-1927-0. PMID: 30342524; PMCID: PMC6195976.
-
Wang X, Han X, Guo X, Luo X, Wang D. The effect of periodontal treatment on hemoglobin a1c levels of diabetic patients: a systematic review and meta-analysis. PLoS One. 2014 Sep 25;9(9):e108412.
-
Halfdanarson O. Proton-pump inhibitors among adults: a nationwide drug-utilization study. Therap Adv Gastroenterol. 2018;11:1-11. doi:10.1177/https.
-
Ye X, Liu H, Wu C, et al. Proton pump inhibitors therapy and risk of hip fracture: A systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2011;23(9):794-800.
-
O’Connell MB, Madden DM, Murray AM, Heaney RP, Kerzner LJ. Effects of proton pump inhibitors on calcium carbonate absorption in women: A randomized crossover trial. Am J Med. 2005;118(7):778-781. doi:10.1016/j.amjmed.2005.02.007.
-
Wu X, Al-Abedalla K, Abi-Nader S, Daniel NG, Nicolau B, Tamimi F. Proton Pump Inhibitors and the Risk of Osseointegrated Dental Implant Failure: A Cohort Study. Clin Implant Dent Relat Res. 2017;19(2):222-232. doi:10.1111/cid.12455.
-
Shea MLO, Garfield LD, Teitelbaum S, et al. Serotonin-norepinephrine reuptake inhibitor therapy in late-life depression is associated with increased marker of bone resorption. Osteoporos Int. 2013;24(5):1741-1749. doi:10.1007/s00198-012-2170-z.
-
Carvalho RS, De Souza CM, Neves JCS, et al. Effect of venlafaxine on bone loss associated with ligature-induced periodontitis in Wistar rats. J Negat Results Biomed. 2010;9(1):1-8. doi:10.1186/1477-5751-9-3.
-
Hakam AE, Vila G, Duarte PM, et al. Effects of different antidepressant classes on dental implant failure: A retrospective clinical study. J Periodontol. 2020;(April):1-9. doi:10.1002/JPER.19-0714.