Immediate Implant Placement in the Anterior: A Case Study (1 CEU)

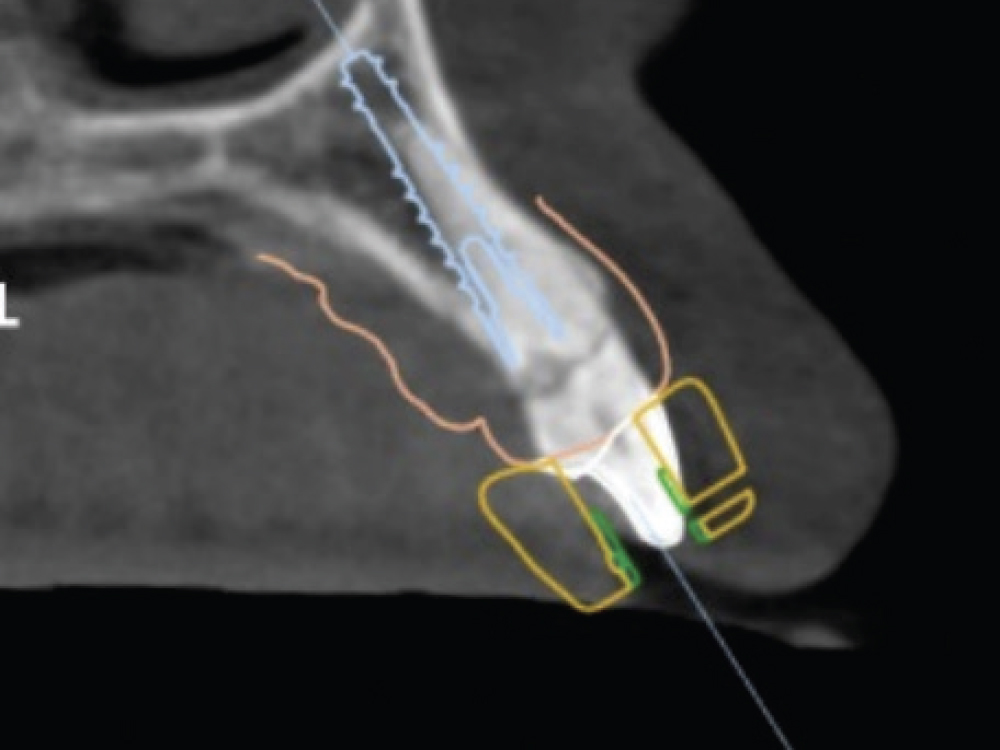
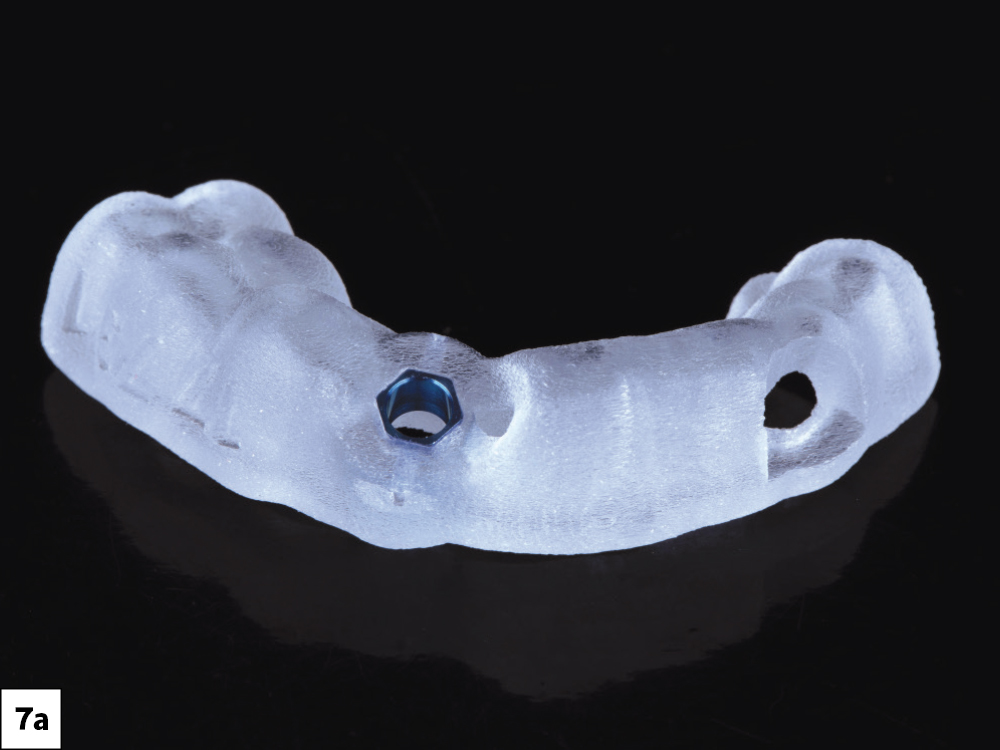
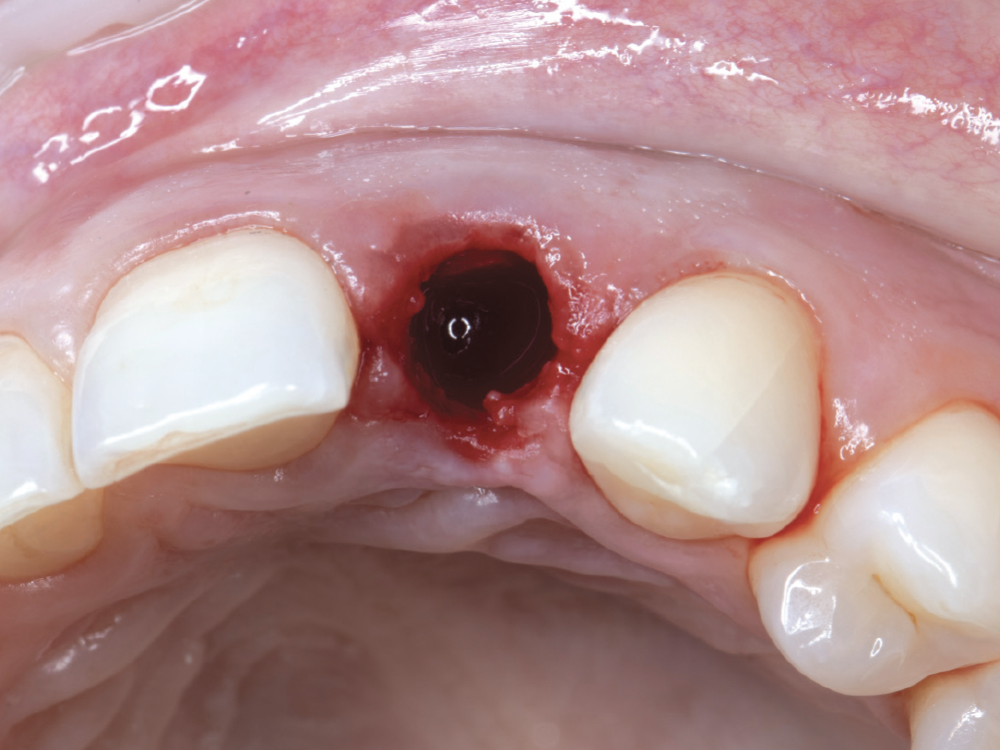
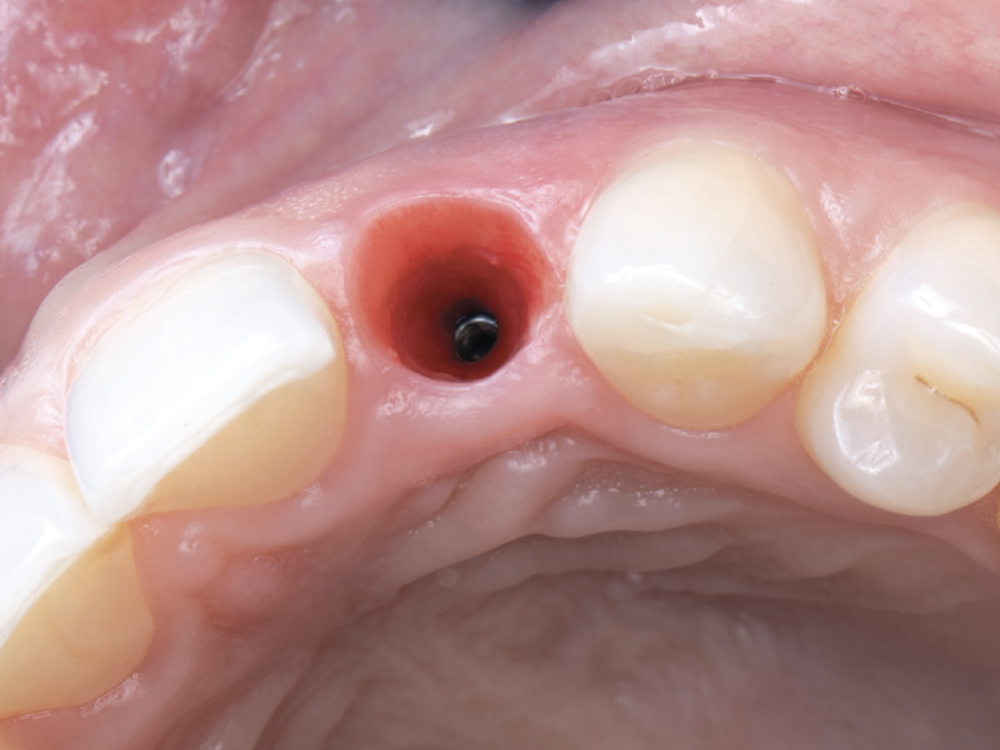
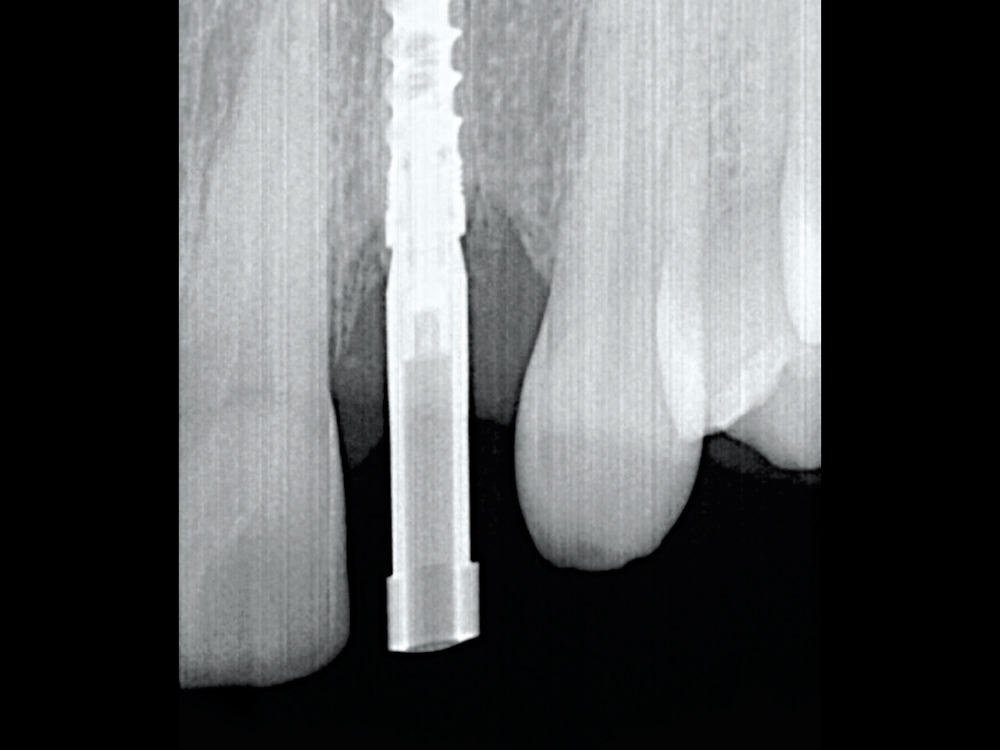
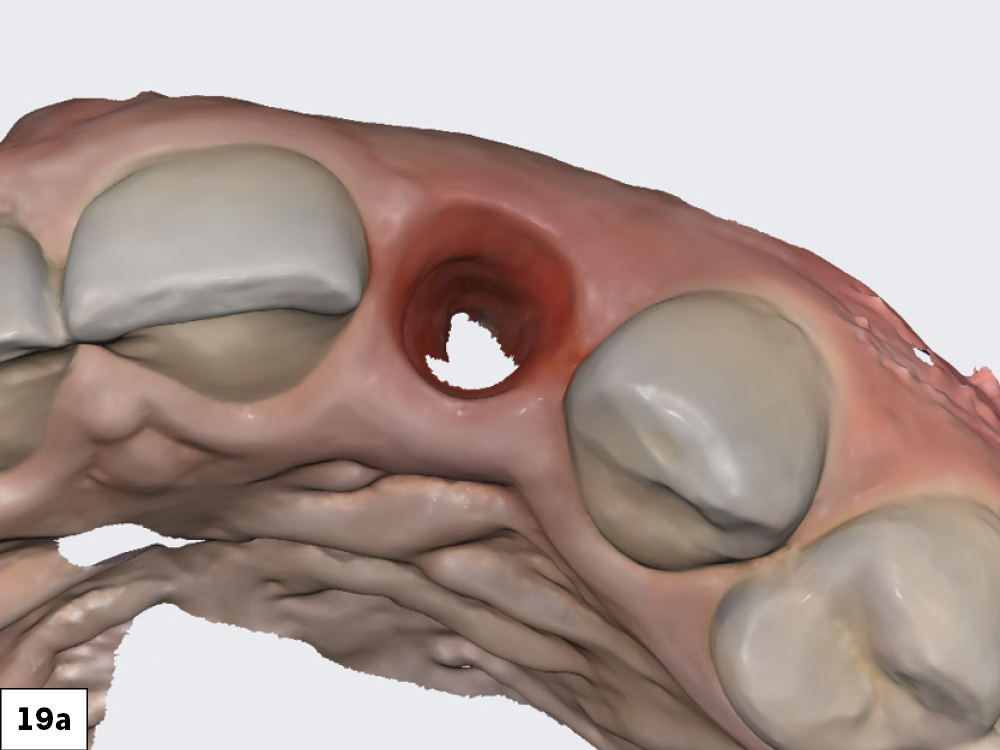
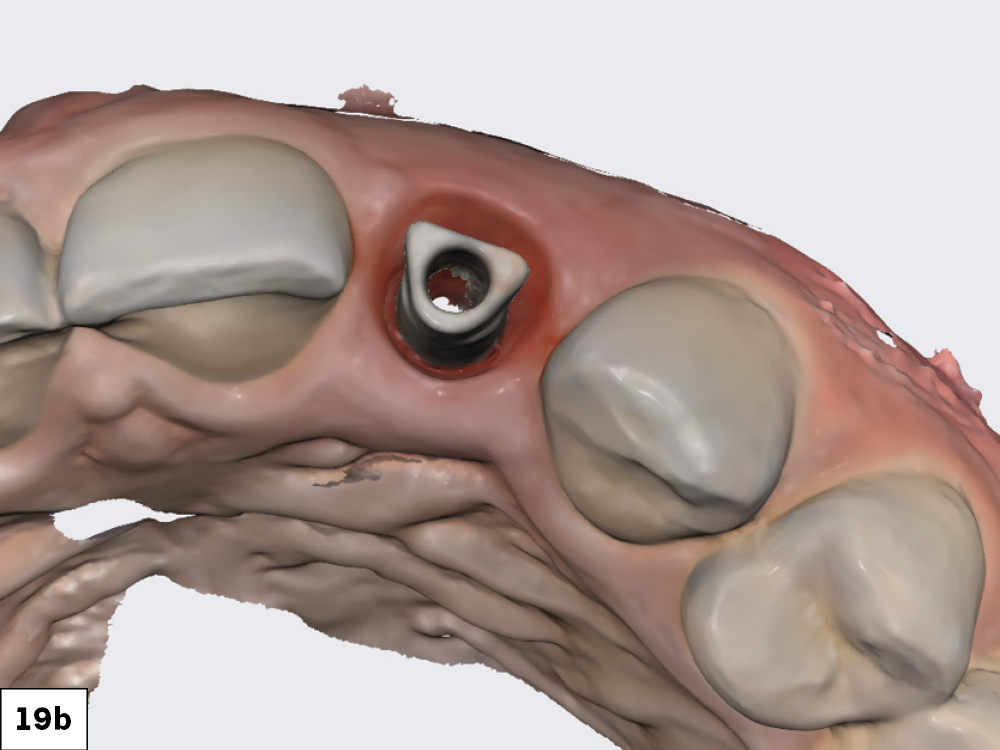
In this case study, the immediate placement of an implant after extraction is demonstrated as a technique for maintaining soft tissue contours. The case study outlines the criteria for immediate loading as well as the methods and tools used for treatment planning with a restorative-driven approach.
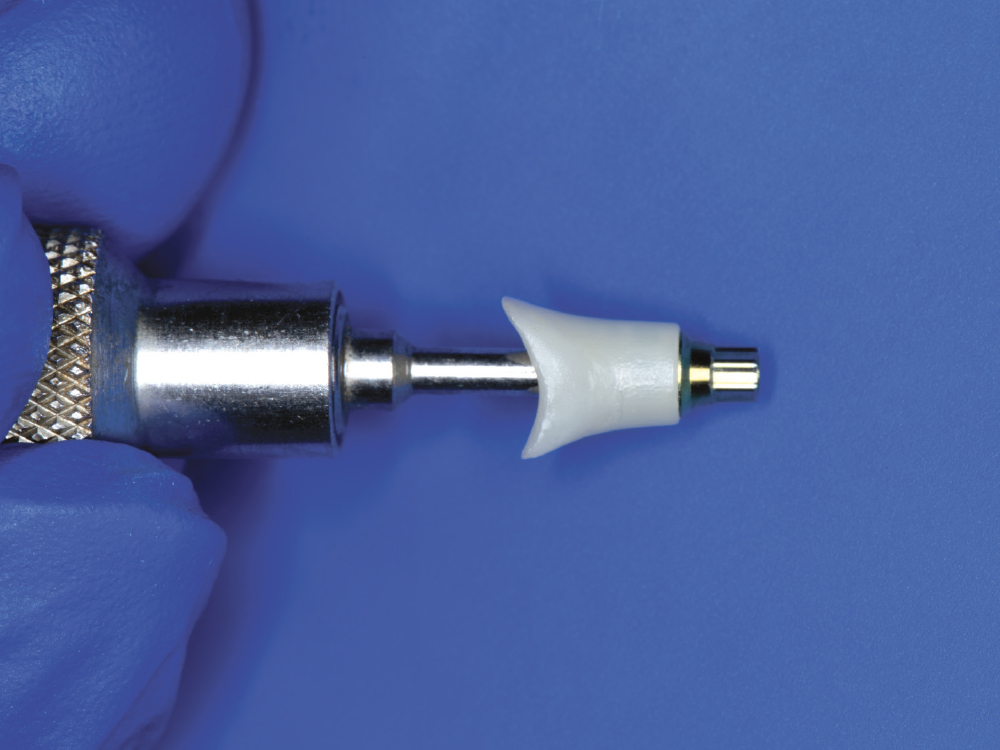
COVER SCREW, HEALING ABUTMENT, OR PROVISIONAL?
Three essential options are available at the time of implant placement. The following chart outlines the criteria used to select the most suitable option for the patient.
CONCLUSION
Treatment does not always unfold as expected. In this case, the implant’s primary stability was insufficient to support the planned immediate load provisional restoration. This common challenge highlights that reality may not always align with desired expectations. The scenario underscores the importance of co-diagnosis, careful planning, and avoiding the rush to finish. Adhering to these principles enabled the maintenance of the patient’s gingival contours and the delivery of an esthetic result.