Management of Incision Line Opening (1 CEU)

Achieving successful soft-tissue closure is crucial for success in dental implant and grafting procedures. Allowing the soft-tissue to heal unimpeded will promote primary intention healing and prevent complications, such as incision line opening (ILO). ILO, or surgical wound dehiscence, is defined as the development of a separation of the tissue layers of a surgical wound, resulting in a lack of primary coverage.1
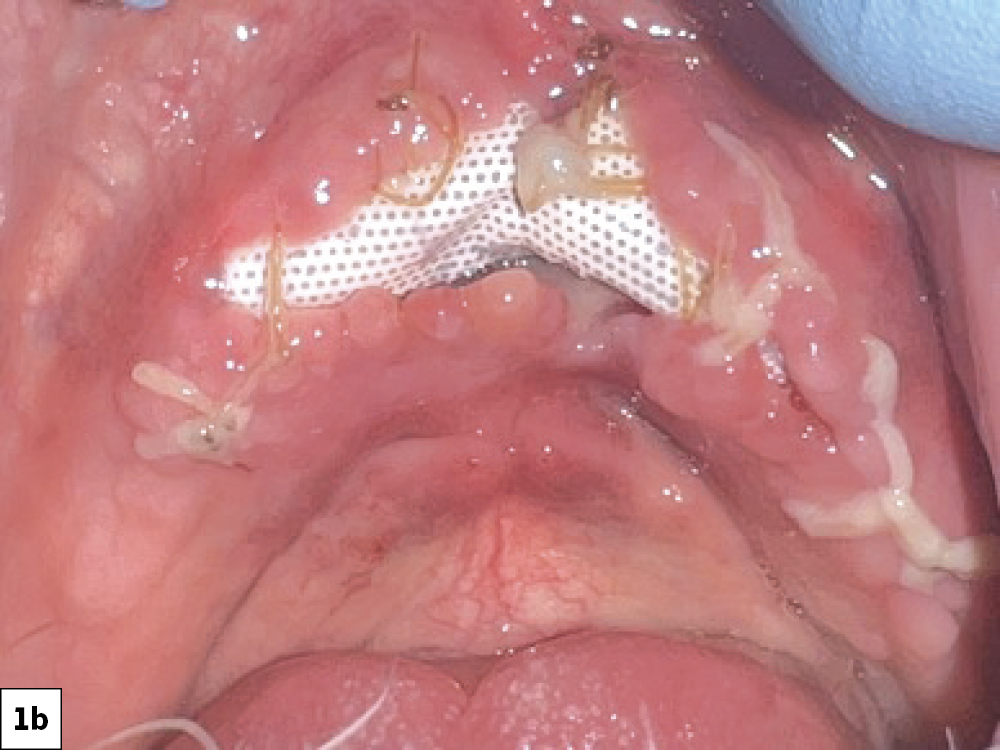
When this wound breakdown occurs, an increased morbidity for dental implant surgery and bone grafting may result because of bacterial contamination (Figs. 1a, 1b). In this article, various techniques and protocols will be discussed to prevent ILO and manage this complication.
SURGICAL WOUND HEALING PHASES
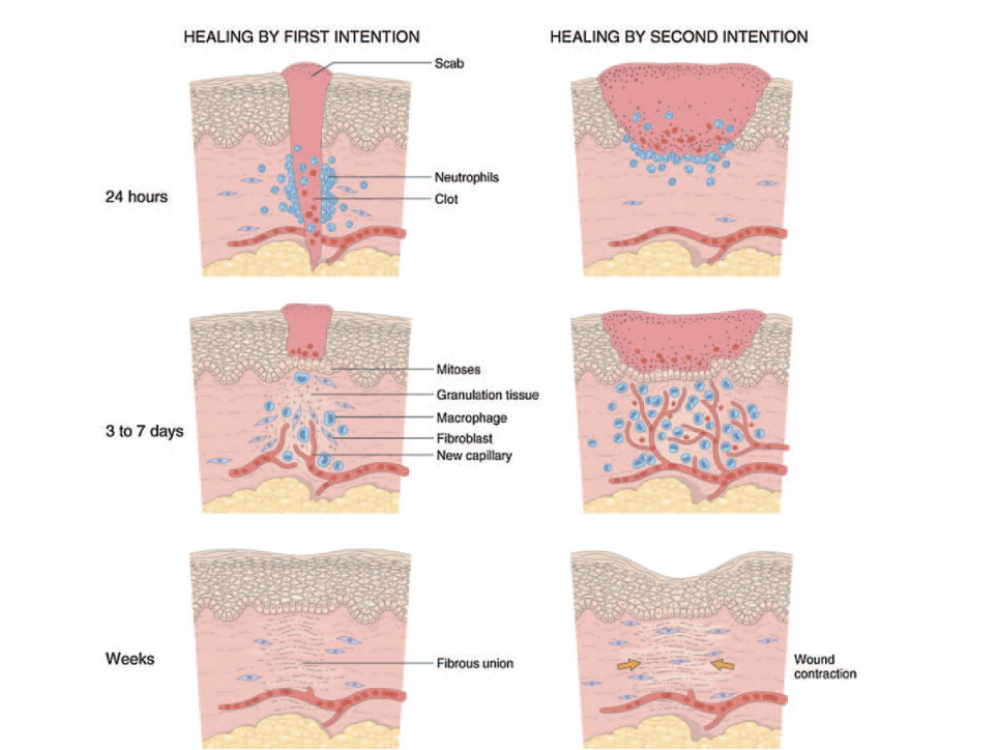
Surgical wound healing, whether by normal or delayed healing, occurs in three phases, (1) the inflammatory phase, (2) the proliferation phase, and (3) the maturation phase.
1. Inflammatory Phase
The inflammatory phase is the body’s natural response to a surgical injury. It is characterized by a vascular and inflammatory response, including local vasoconstriction for the first five to 10 minutes followed by a local vasodilatory response. This phase normally takes place the first few days after injury.
2. Proliferation Phase
The proliferation phase is characterized by the formation of new granulation tissue, which is comprised mainly of collagen and extracellular matrix. The proliferation phase begins within 24 hours after injury and may last three to 12 days. It is characterized by angiogenesis, collagen deposition, granulation tissue formation and wound contraction. In addition, epithelial cells will begin to resurface on the surgical wound, which is termed epithelialization.
3. Maturation Phase
The maturation phase is the final phase in the healing process and occurs when the wound has closed. The remodeling of collagen from type III to type I will occur. During wound contraction, myofibroblasts decrease the size of the wound by gripping the wound edges and contracting, using mechanisms that resemble smooth muscle cell contraction. The wound scar gains strength and volume, and erythema decreases. Generally, complete scar maturation and final tensile strength will take approximately 12 to 18 months.
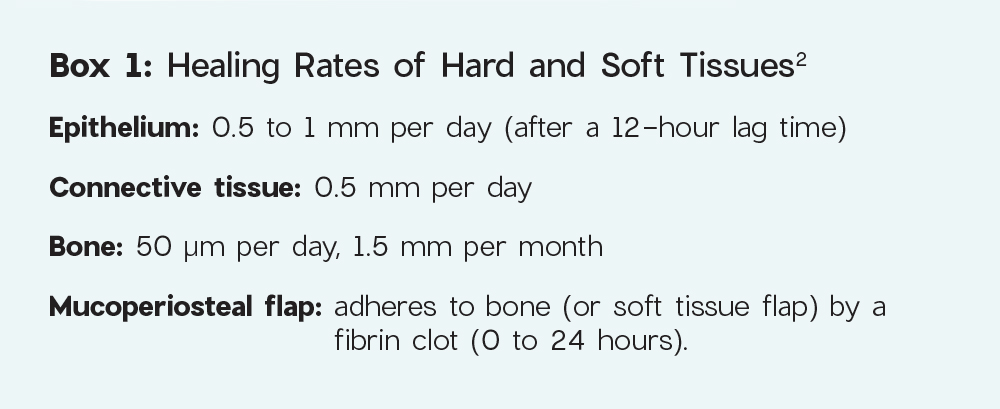
The healing rates of the soft and hard tissues may be used to determine if a patient is healing on schedule. The time for wound repair subsequent to surgery is tissue specific (Box 1).
SURGICAL WOUND HEALING CLASSIFICATION
Surgical wounds may heal by either primary or secondary intention. Clinicians should strive for primary intention as this results in more predictable healing. In most cases of ILO, the surgical wound will heal via secondary intention (Fig. 2).3
1. Primary Intention
Primary intention is the ideal healing process, which occurs when the two wound edges are approximated and stabilized via sutures. Soft tissue flaps are strategically positioned in “passive” and tension-free configurations, which allows for a rapid and efficient healing process. Achieving primary intention closure is crucial for hemostasis, minimizing infection risk, preventing bone necrosis and enhancing patient comfort.
2. Secondary Intention
Secondary intention is typically observed in wounds where the two wound edges are separated. Healing by secondary intention follows clot formation, granulation, collagen deposition and delayed epithelialization. Epithelial cells located at the wound margin must migrate across the granulation tissue, eventually covering the wound surface. In most cases of ILO, the wound may only heal through secondary intention, potentially increasing morbidity.
CONSEQUENCES OF INCISION LINE OPENING
The sequalae of ILO can vary depending on the specific implant or bone grafting procedure completed. When ILO occurs after implant placement, crestal bone loss or failure of the implant may result. The occurrence of ILO may produce a bacterial smear layer on the implant body, potentially hindering optimal bone formation. If the bone resorption process progresses, infection may result, necessitating the removal of the implant.
When ILO occurs following guided bone regeneration procedures, increased risk of delayed healing, lack of bone formation and increased susceptibility to infection may occur. In addition, the premature exposure of membranes further amplifies the risk of infection and resultant poor bone formation.
PREVENTION OF INCISION LINE OPENING
During oral implantology procedures, many factors may predispose surgical wounds to ILO. Therefore, to minimize the risk of ILO, adherence to certain surgical principles is essential.
1. Incision in Keratinized Tissue
Whenever feasible, the primary incision should be positioned in keratinized tissue. Keratinized tissue contains the protein keratin, which results in greater strength and resiliency of the tissue. This tissue enhances vascularity and minimizes the possibility of tissue flap tearing due to the increased tensile strength compared to mucosa.
2. Broad-Based Flap Design
A broad-based incision consists of a flap design which has a base that is larger than the apex (ridge). This incision design allows for better preservation of blood supply to the surgical site, which is crucial in preventing ischemic necrosis and decreasing the likelihood of ILO (Figs. 3a, 3b).
3. Allow for Adequate Access
The flap design should allow for proper visualization of the surgical site and accommodate instrument insertion and manipulation. Inadequate flap size may lead to excessive retraction pressure, which may result in increased inflammation and compromised incision line healing.
4. Clean, Concise Incision
A precise, well-planned incision should be completed with a sharp surgical blade that minimizes trauma to the surrounding tissue. Refrain from making repeated passes along the incision line, as this may lead to increased bleeding and inflammation. If required, repeated incisions should be made in the same plane, which results in less bleeding and tissue trauma.
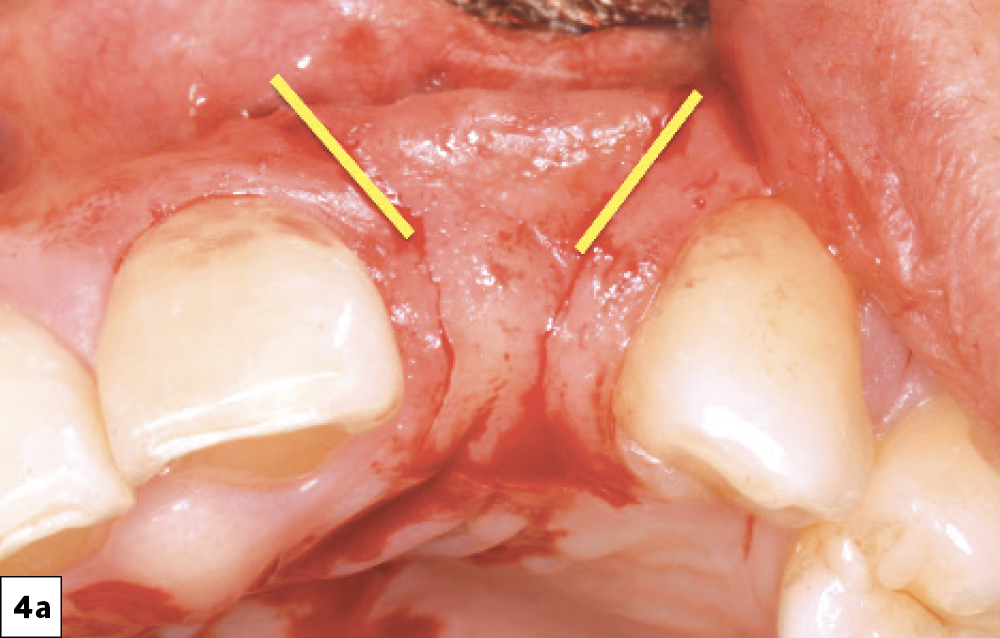
5. Papilla-Sparing Incisions
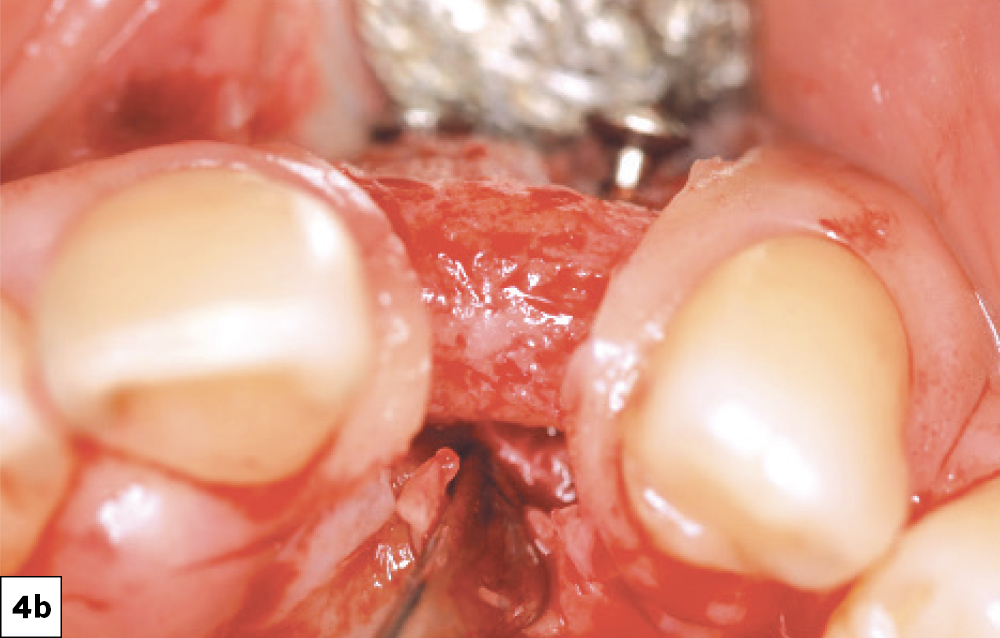
When incisions are made near adjacent natural teeth, “papilla-sparing” incisions should be incorporated. These incisions are designed to allow for 1.0 to 1.5 mm of the interproximal papilla adjacent to each tooth to remain, thereby minimizing tissue recession. The purpose of this incision design is to ensure primary closure with no voids and minimal scarring, promoting optimal healing and maintaining the integrity of the interproximal tissues (Figs. 4a, 4b).
6. Full-Thickness Reflection and Atraumatic Flap Elevation
Ideally, the surgical flap should be full thickness, including surface mucosa, submucosa, and periosteum. Careful elevation minimizes trauma to the soft tissue, and meticulous handling with appropriate tissue forceps will contribute to improved flap management.
7. Relieving Tissue (Tension-Free)
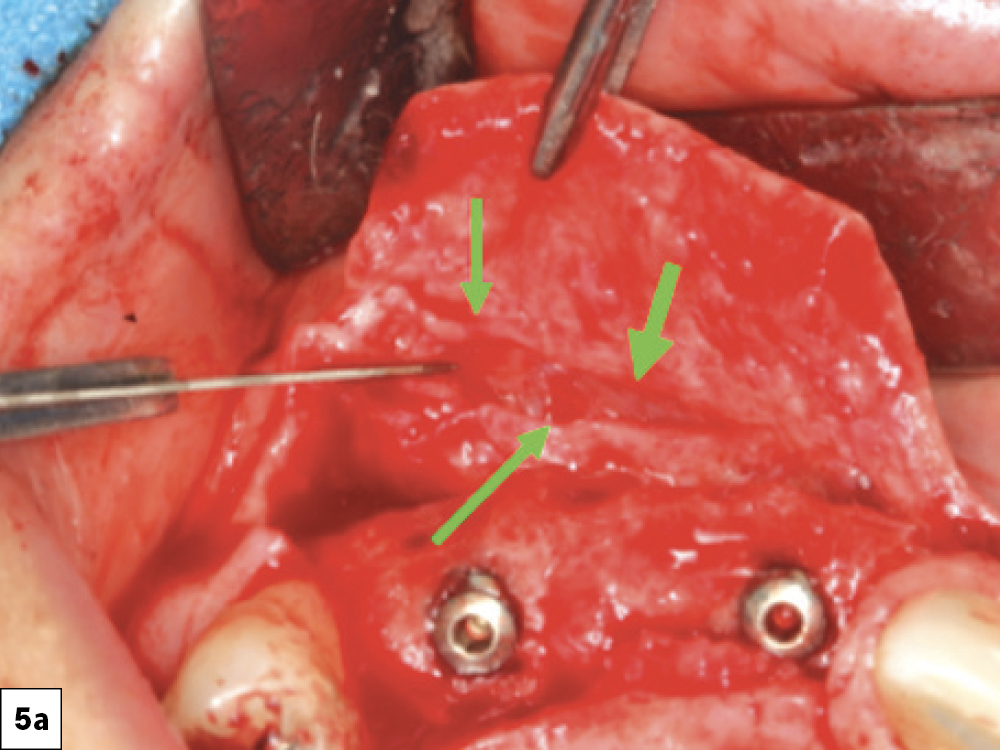
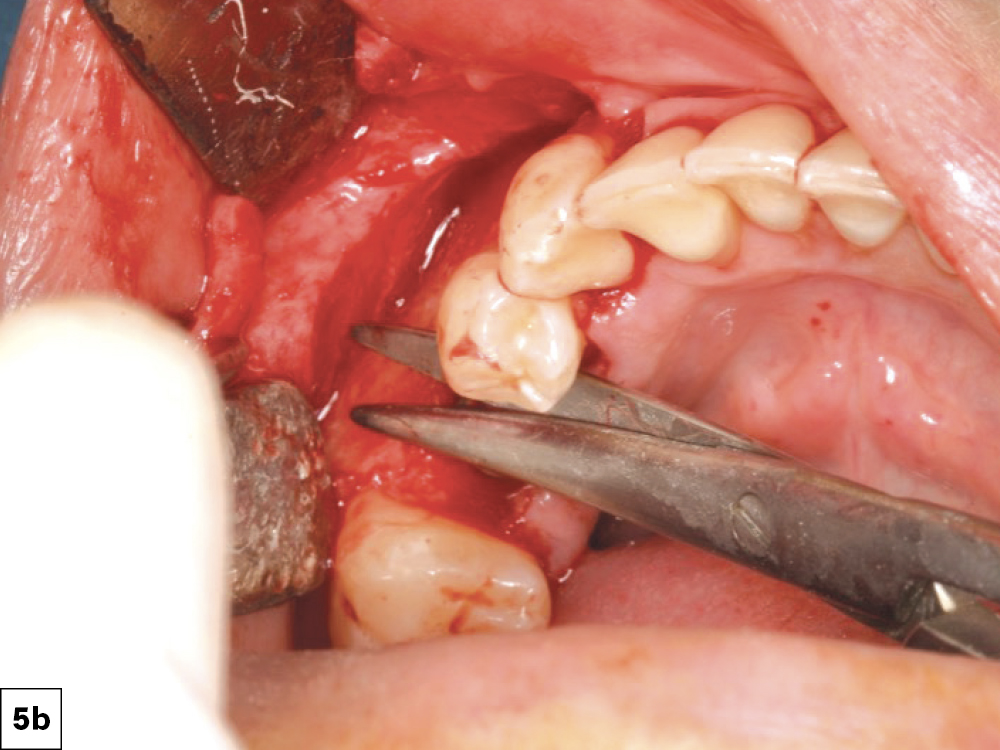
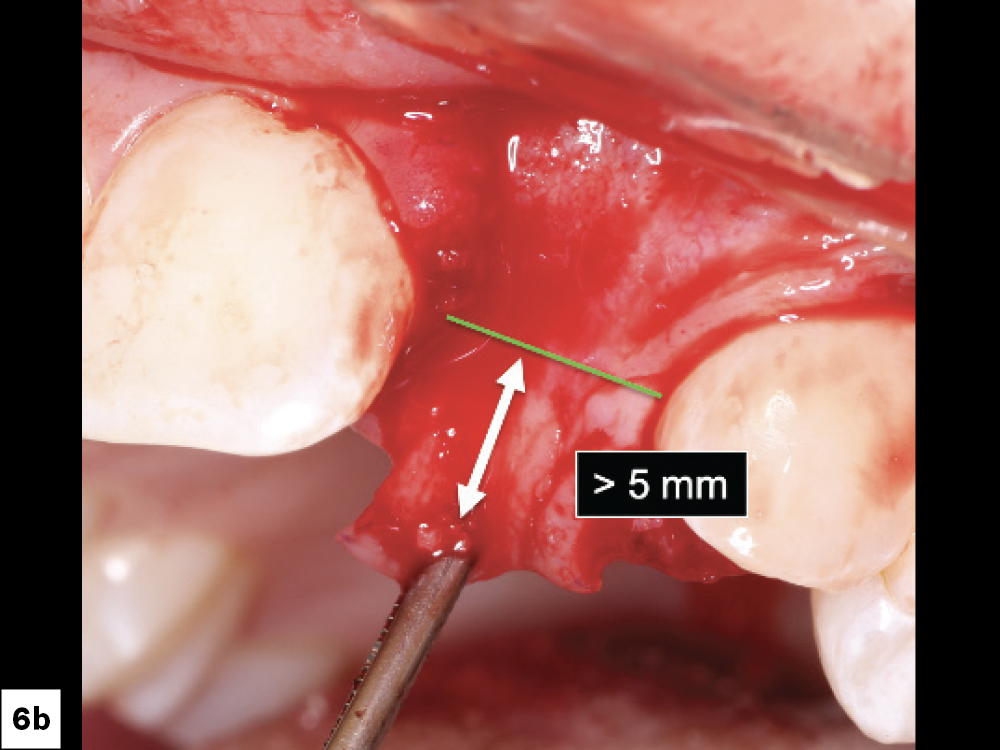
Excessive flap tension is a leading cause of ILO. This can be prevented by appropriate incision and flap design and periosteal releasing incisions. Clinicians should utilize relieving procedures (i.e., periosteal and blunt dissection) in order to reduce the tension on the incision line. Ideally, the flap should be able to be stretched a minimum of 5 mm past the incision line. Insufficient soft tissue mobility or excessive tension on the tissues during the healing phase may lead to loss of approximation of the tissue margins (Figs. 5a, 5b, 6a, 6b).
Excessive flap tension is a leading cause of ILO.
8. Use of Periosteal Releasing Incisions (PRI)
Periosteal releasing incisions allow for the release or detachment of the periosteum. PRI allows for the controlled release of periosteal attachments, which allows improved mobility of the soft tissues, enhances surgical exposure and reduces tension on the surgical wound edges. Studies have shown that PRI can enhance flap advancement up to 171.3% without excessive tension.4
9. Reduce Bacteria in Incision Line
If local bacteria (most commonly streptococcus and pyogencus) are present within the incision line, epithelization may be inhibited. Local bacterial contamination may result in decreased tissue pH, preventing connective tissue repair and increasing the inflammatory response. This will result in the body responding with an increase in neutrophils (i.e. release lysosomal enzymes), resulting in proteolysis and tissue breakdown.5,6
10. No Interim Prosthesis Pressure
If an interim prosthesis places pressure on the surgical wound the microcirculation may be affected, resulting in compromised blood supply to the wound edges.6 The clinician should modify interim prostheses to avoid force being directed on the surgical site and instruct the patient to avoid direct mastication on the surgical site area (Figs. 7a, 7b).
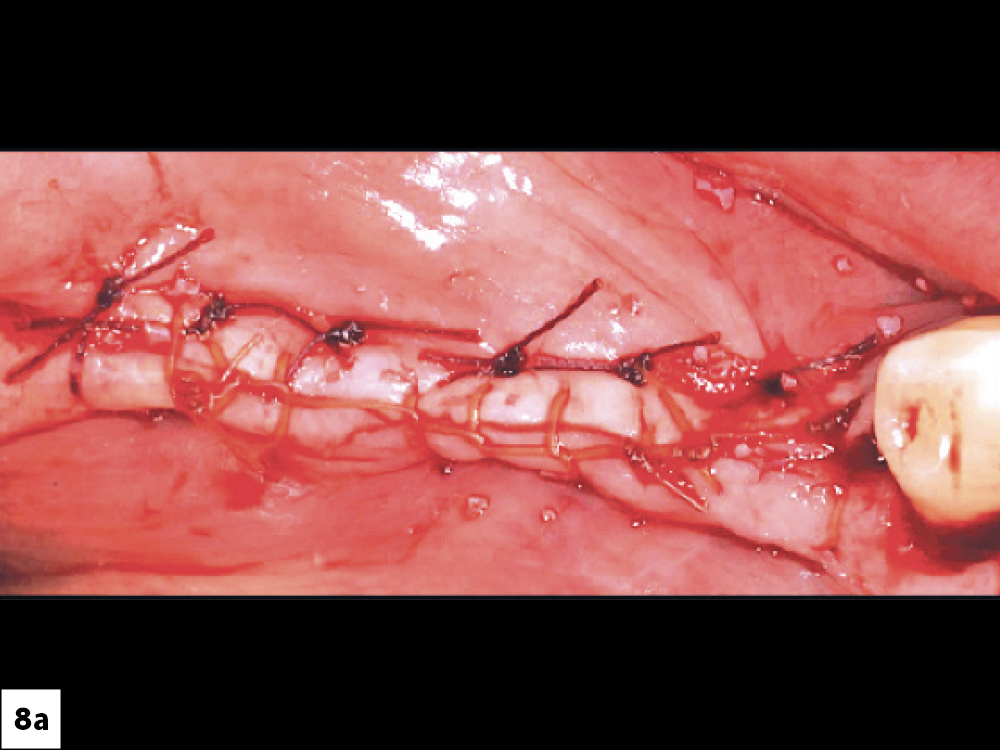
11. Ideal Suturing Technique
The goal of suturing the surgical wound is to approximate the tissue margins to promote hemostasis and allow for unimpeded healing. If the suture fails to secure wound closure, wound dehiscence will result. A suture with a high tensile strength like RELI® REDISORB® PRO Sutures (available through Glidewell Direct; Irvine, Calif.) should ideally be used to maintain primary closure of the incision line. For large flap procedures, a continuous locking suture with secondary horizontal mattress sutures is recommended. This type of suturing technique results in “everted” flap edges, which resist tension from associated muscle attachments (Figs. 8a, 8b).
12. Remove Bone Particles from Incision Line
During grafting procedures, after final suturing, it is not uncommon for bone particles to be incorporated between the flap margins. Clinicians should always verify that no bone is present that may impede the healing process (Fig. 9).
MANAGEMENT OF INCISION LINE OPENING
If ILO after dental implant placement or bone graft surgery occurs, it is imperative the clinician address it promptly to prevent complications and support proper healing. The treatment of ILO includes two options, either (1) resuturing or (2) allowing to heal via secondary intention.
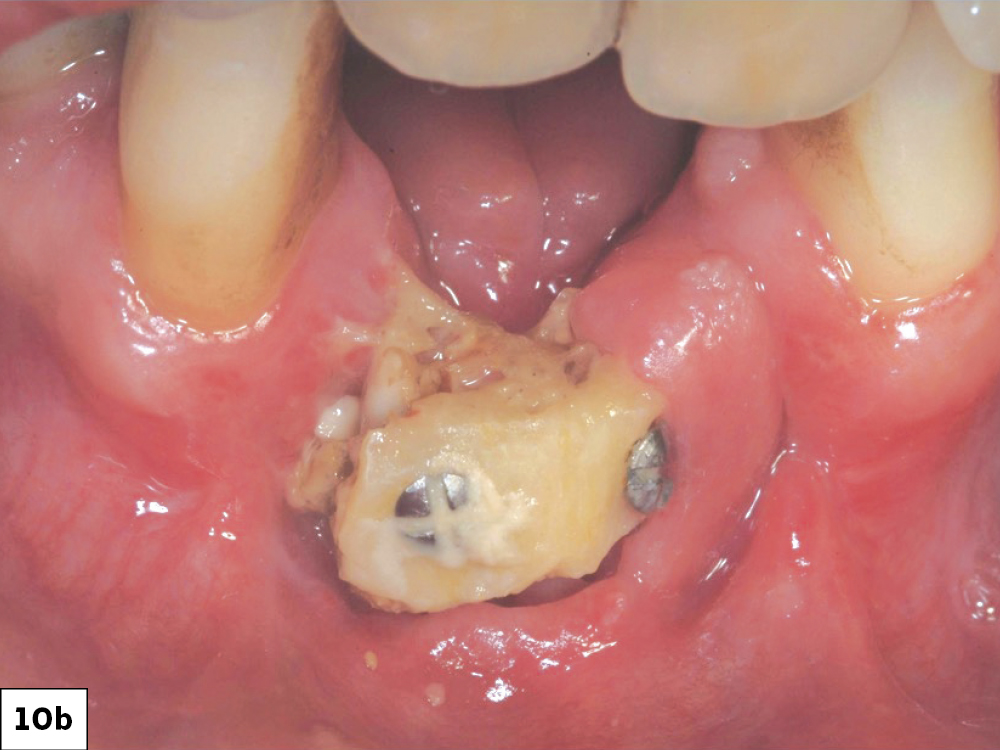
Resuturing
Resuturing wound dehiscences is a challenging procedure, which often results in delayed and unpredictable healing (Fig. 10). Attempting to resuture a fresh wound, particularly when the epithelium is thin and friable, often leads to tearing of the incision line, potentially causing a larger dehiscence or infection. Therefore, resuturing should be approached with care. Greenstein et. al., suggest that resuturing is more viable when the dehiscence is small and occurs within 24 to 48 hours.2 As the wound enlarges (2 to 3 cm) or the time elapsed exceeds 2 to 3 days, the feasibility of excising and resuturing is decreased and commonly results in increased morbidity and should not be attempted.8
Healing via Secondary Intention
In most ILO cases, the correct treatment is to allow the surgical wound to heal via secondary intention. Allowing the site to heal by secondary intention requires considerable discipline and patient cooperation for a successful outcome (Box 2, Fig. 11). This treatment approach is influenced by various factors such as the health of existing tissue, tissue thickness, location, patient age and the size of the dehiscence. The technique involves implementing the following:
a. Hygiene/Antimicrobial Measures: Use of hygiene and antimicrobials to decrease the bacterial count within the incision line, thereby reducing the possibility of infection and allowing for more predictable healing.
b. Avoidance of ILO Surgical Site Trauma: The clinician must strongly emphasize that the patient avoid any deleterious activity (e.g., smoking, alcohol, direct mastication). In addition, the clinician must implement a rigorous follow-up evaluation protocol to assess and monitor the healing process.
CONCLUSION
The prevention of complications in the field of oral implantology requires scrupulous adherence to procedural principles, proficiency in surgical skills and consistent practice. However, despite a clinician’s best efforts, occurrences of ILO may still arise. In such instances, prompt attention and treatment are crucial to attaining a favorable surgical outcome.
RELI and REDISORB are registered trademarks of Myco Medical Supplies, Inc.
Available CE Course
References
-
Sadig W, Almas K. Risk factors and management of dehiscent wounds in implant dentistry. Implant Dent. 2004;13(2):140-7.
-
Greenstein G, Greenstein B, Cavallaro J, et al. Flap advancement: practical techniques to attain tension-free primary closure. J Periodontol. 2009;80(1):4-15.
-
Suzuki JB, Resnik RR. Wound dehiscence: incision line opening. In: Misch CE, editor. Misch’s Avoiding Complications in Oral Implantology. Mosby; 2018:402-439.
-
Rosenfeld EA. Inverted periosteal flap: an alternative to the buccal advancement flap for tension-free, watertight closure1. J Oral Maxillofac Surg. 2014 Jul;72(7):1244-50. doi: 10.1016/j.joms.2014.03.0062. Epub 2014 Mar 203. PMID: 24768423.
-
Trowbridge HD, Emling RC. Inflammation: A Review of the Process. 5th ed. Quintessence Publishing Co, Inc; 1997:149-167.
-
Allgöwer M. Wound healing. In: Wound Closure in the Operating Theater. 1st ed. B. Braun Melsungen AG; 1981:20, 26, 28, 66.
-
Jovanovic SA, Spiekermann H, Richter EJ. Bone regeneration around Ti dental implants in dehiscenced defect sites: a clinical study. Int J Oral Maxillofac Implants. 1992;7:233-45.
-
Greenstein G, Cavallaro J, Romanos G, et al. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: a review. J Periodontol. 2008;79(8):1317-29.
-
Suzuki JB, Resnik RR. Wound dehiscence: incision line opening. In: Misch CE, editor. Misch’s Avoiding Complications in Oral Implantology. Mosby; 2018:402-439.