Car Salesman Gets a New Grille

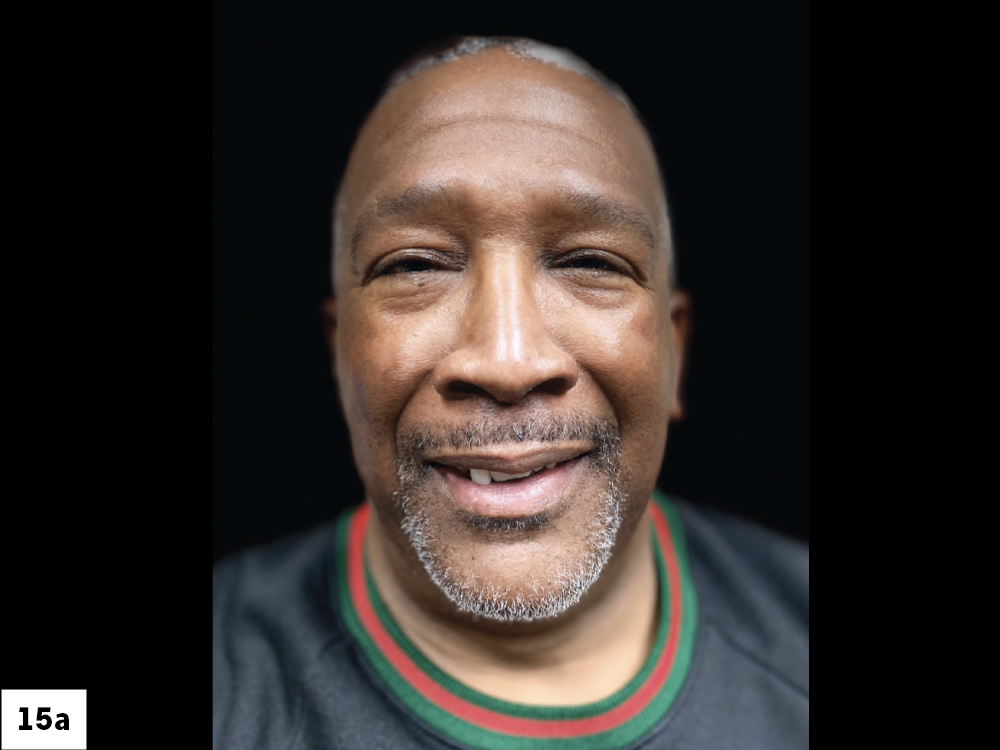
Sometimes a disappointing experience can prevent patients from pursuing treatment that they need and want. The patient in the following case study, a personable automobile sales professional, felt apprehensive about pursuing dental implant treatment after an unsatisfying consultation with another doctor several years earlier.
After he shared his story with me, we arranged a no-fee consultation so I could understand his expectations and provide the details he needed to make an informed decision. The process is not about closing a “sale” — our goal is to educate the patient about how we can meet their desires and address their health needs.
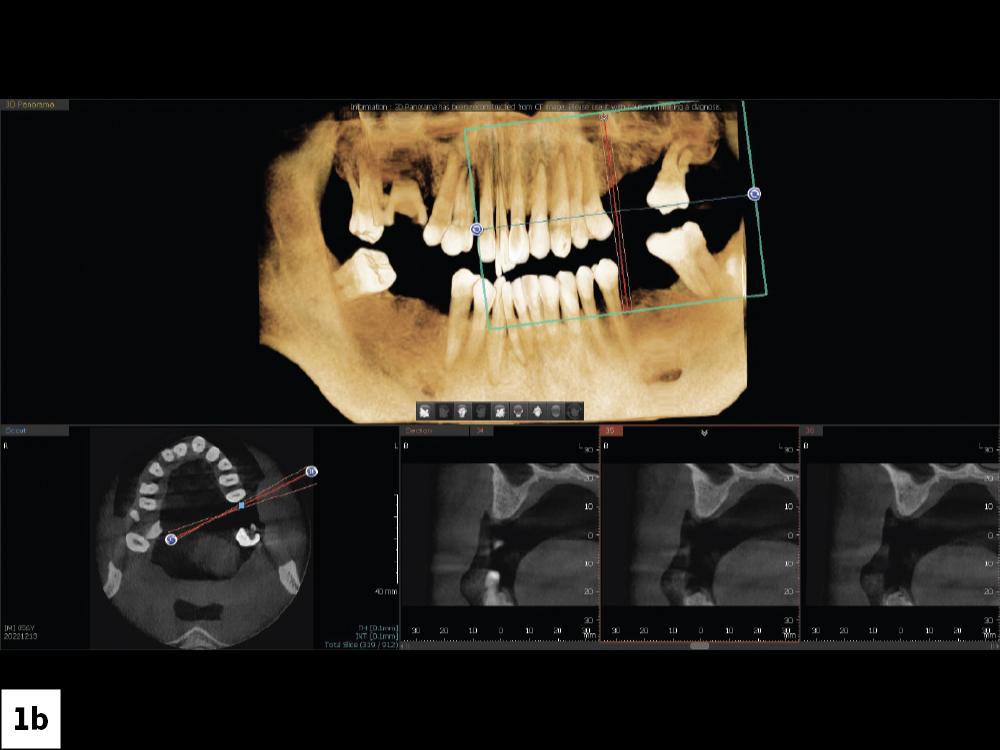
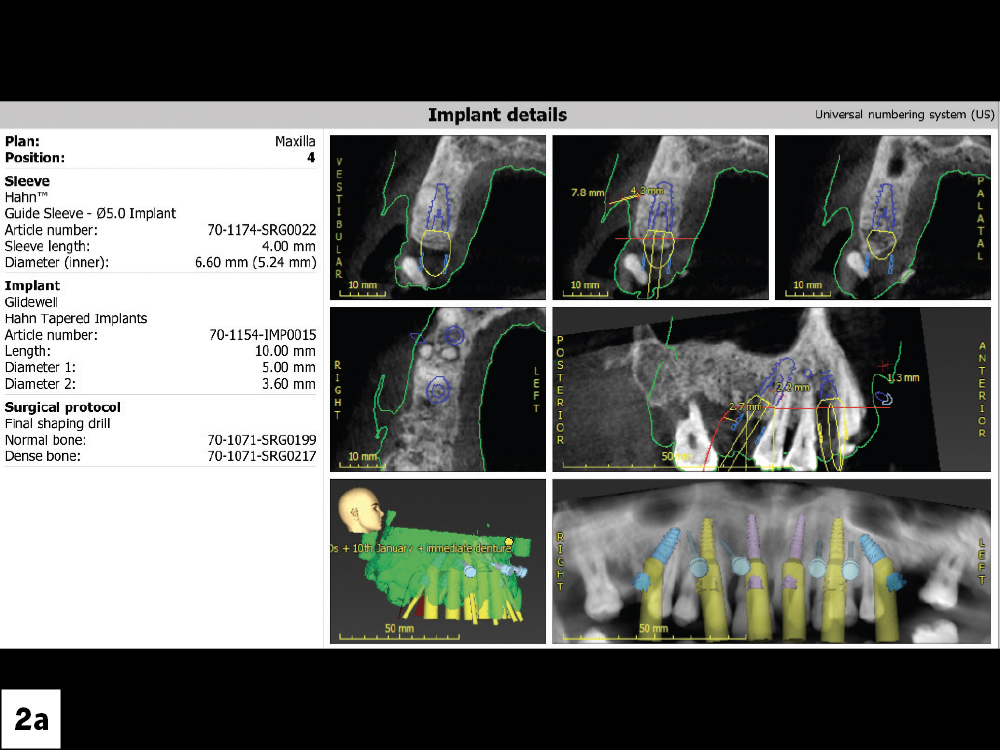
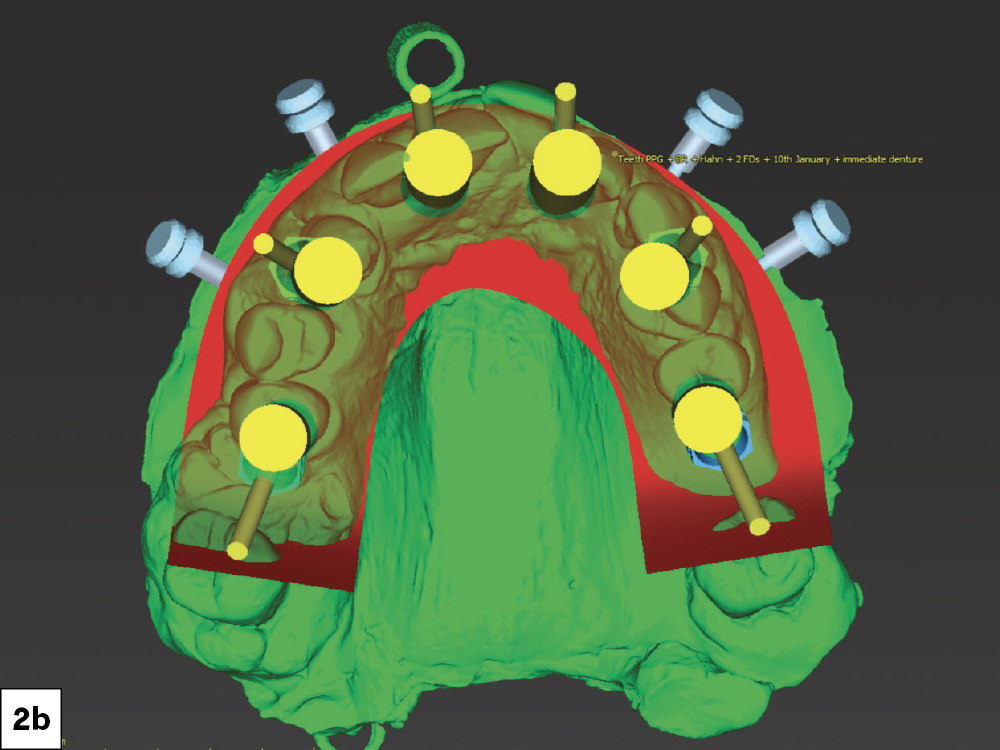
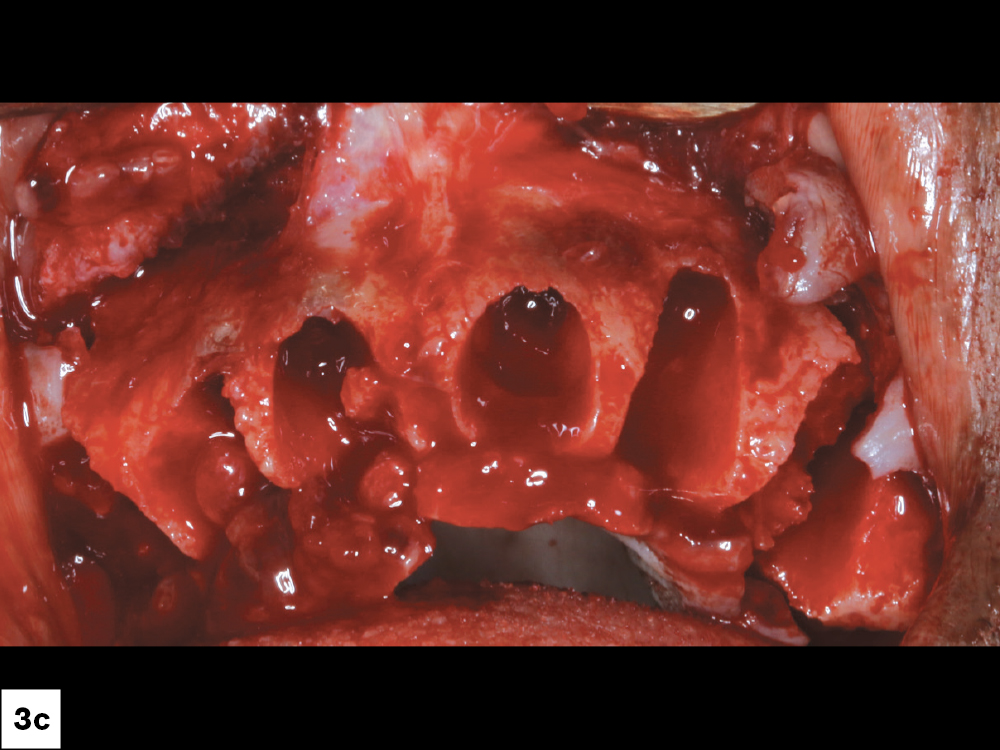
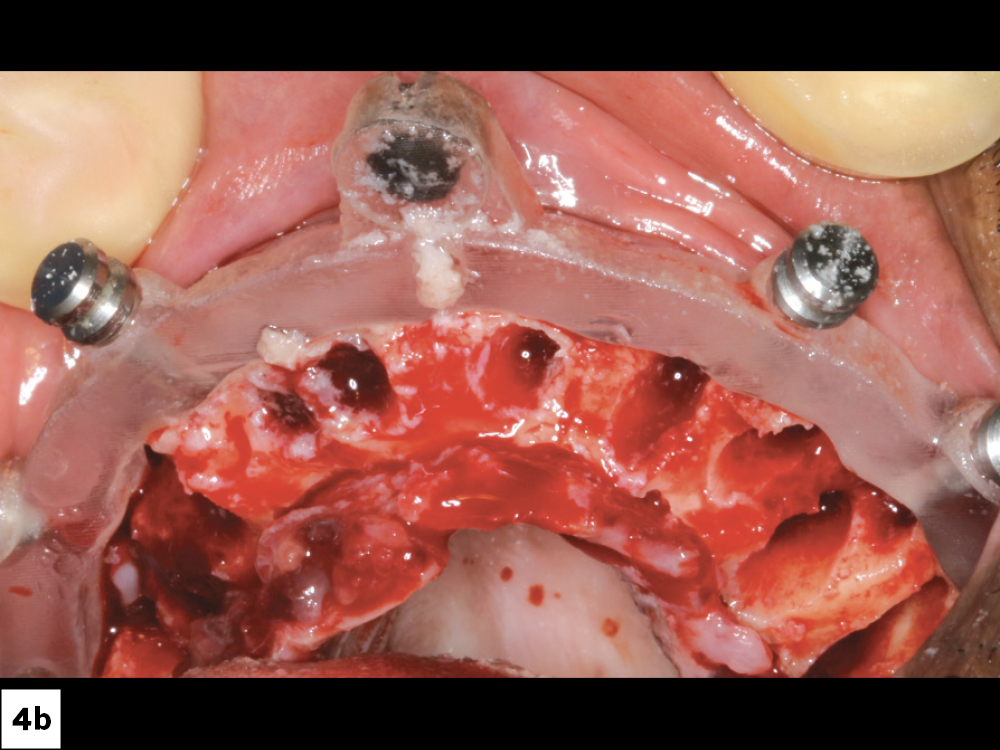
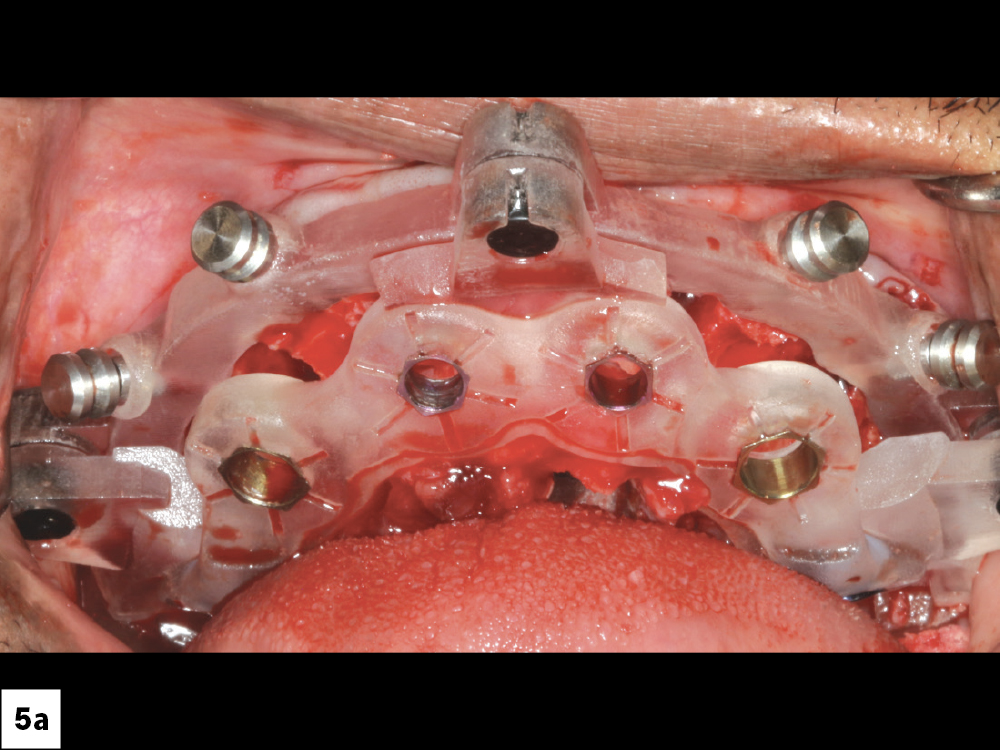
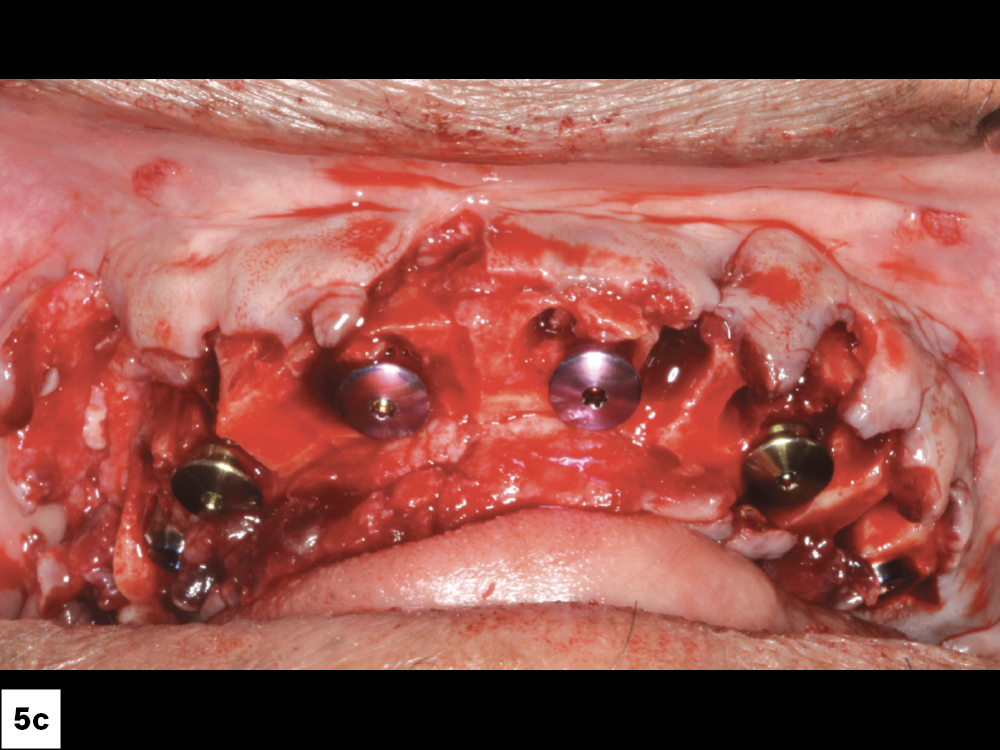
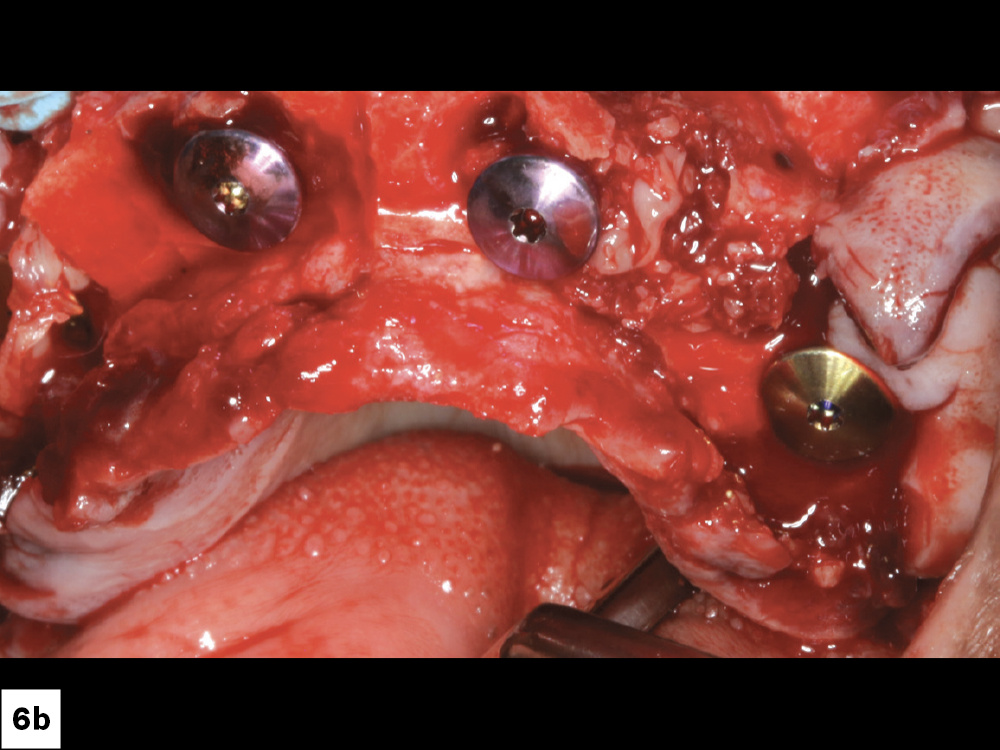
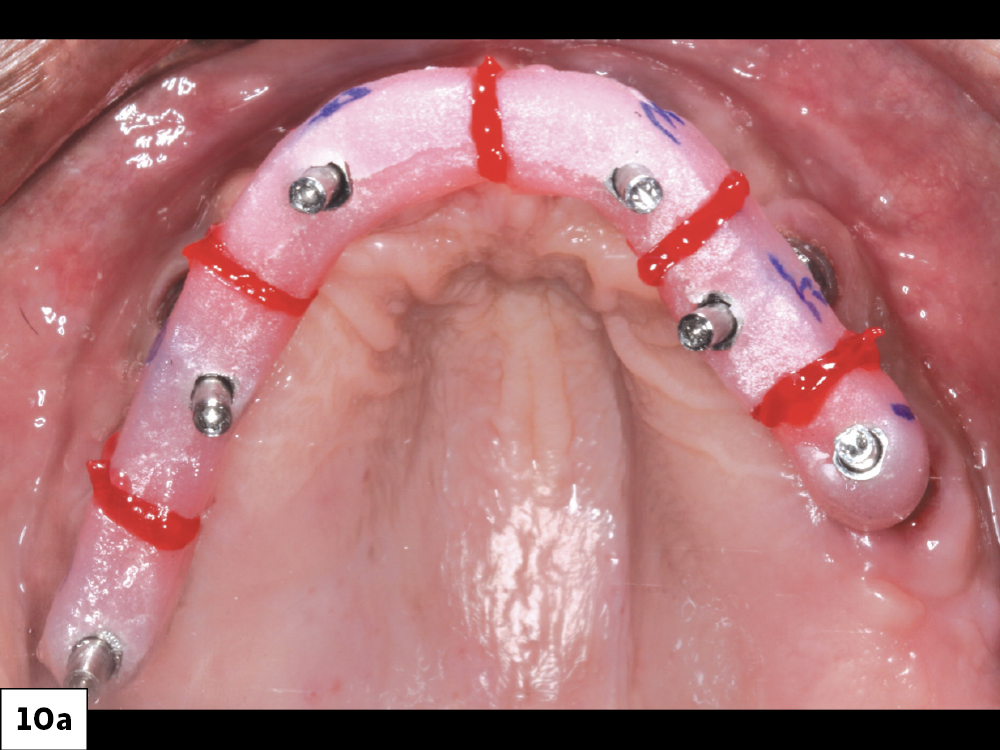
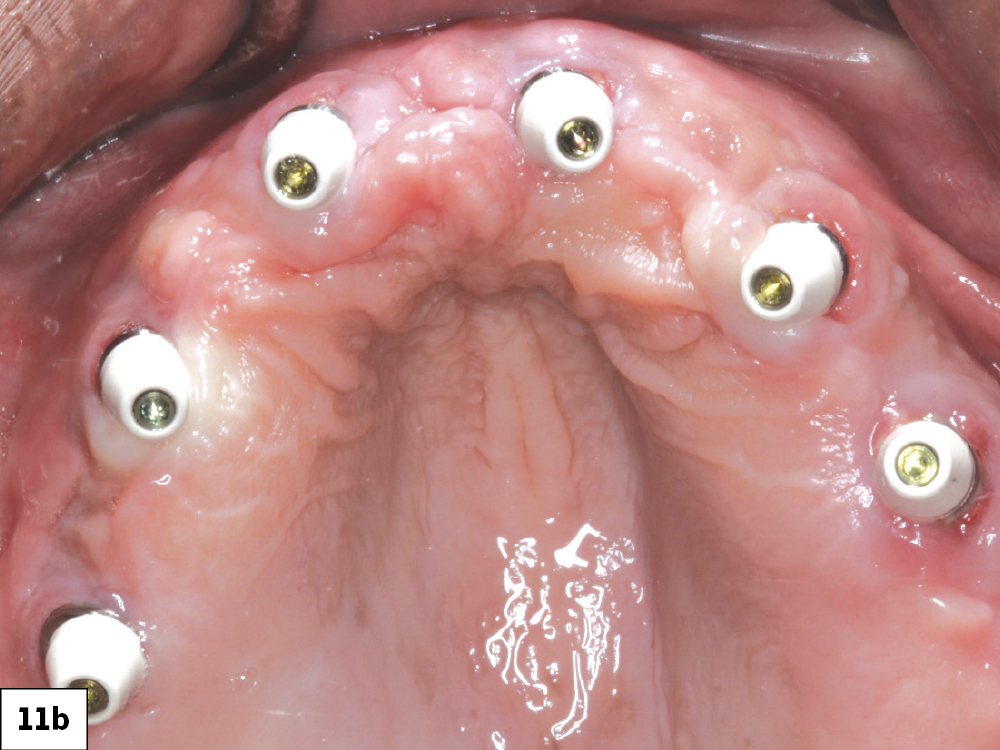
CASE REPORT
The process is not about closing a “sale” — our goal is to educate the patient about how we can meet their desires and address their health needs.
CONCLUSION
Esthetics motivated the patient to pursue a full, upper implant reconstruction. However, the additional health benefits further validated his decision.
A thorough yet efficient process made the procedure possible and addressed any reservations the patient had due to past experiences. Emphasizing the many positives, without pressure — implants as a health and lifestyle choice as opposed to a product to be sold — helped the patient take this important step.