Getting Started with Anterior Implant Placement

Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Most dentists wisely select posterior cases when they are in the early stages of the learning curve for implant surgery. Although moving from the posterior region of the mouth to the esthetic zone can be intimidating, clinicians can surgically place and restore implants in the anterior with confidence by following some straightforward criteria for success. The primary areas on which to focus include case selection, implant positioning, and prosthetically driven treatment planning.
CASE SELECTION
When placing implants in the esthetic zone, it is important to understand and manage your patients’ expectations. I always tell patients that all restorations in the anterior are difficult — whether implant or traditional crown & bridge — due to challenges with matching the shade and characterization of adjacent teeth. I suggest letting patients know that the restoration will look great, but when they look at it very closely, they may notice a difference. It’s also a good idea to begin with patients who have been part of your practice for some time, as the rapport that you have developed with them often makes it easier to comprehend and meet their expectations.
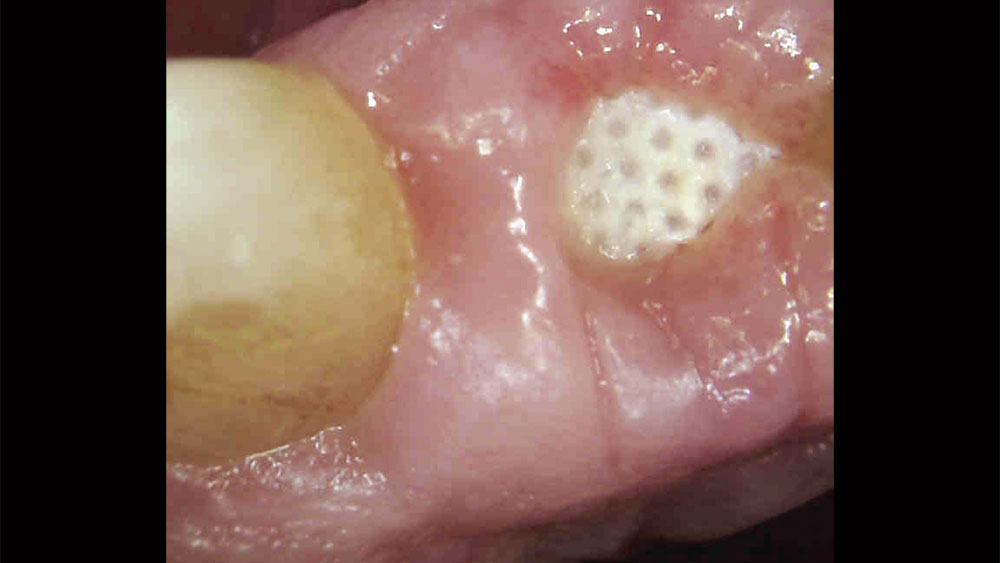
For the first few anterior cases, you should select clinical situations in which an untreatable tooth is removed, the extraction site is grafted, and the implant is placed after several months of healing. This approach allows you to develop the ideal soft-tissue contours and bone volume needed for straightforward implant surgery and a predictable outcome. Until you have more experience, I would not suggest extraction with immediate implant placement — unless you have Dr. Jack Hahn standing by your side! It’s also important to select patients who have favorable teeth alignment as well as a thick tissue biotype, both of which make it easier to achieve a natural emergence profile and esthetic result. High smile lines should be avoided.
Until you have more experience, I would not suggest extraction with immediate implant placement — unless you have Dr. Jack Hahn standing by your side!
PROPER CASE SELECTION
- Know your patients and manage their expectations
- Extract, graft and wait
- Avoid high smile lines
- Select favorable tooth alignment
- Look for thick tissue biotype
IMPLANT POSITIONING
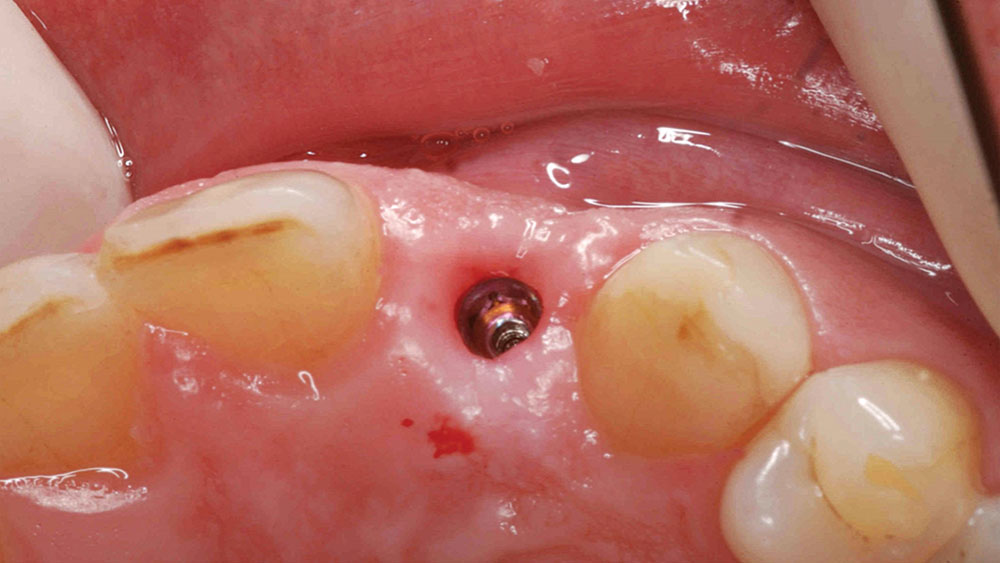
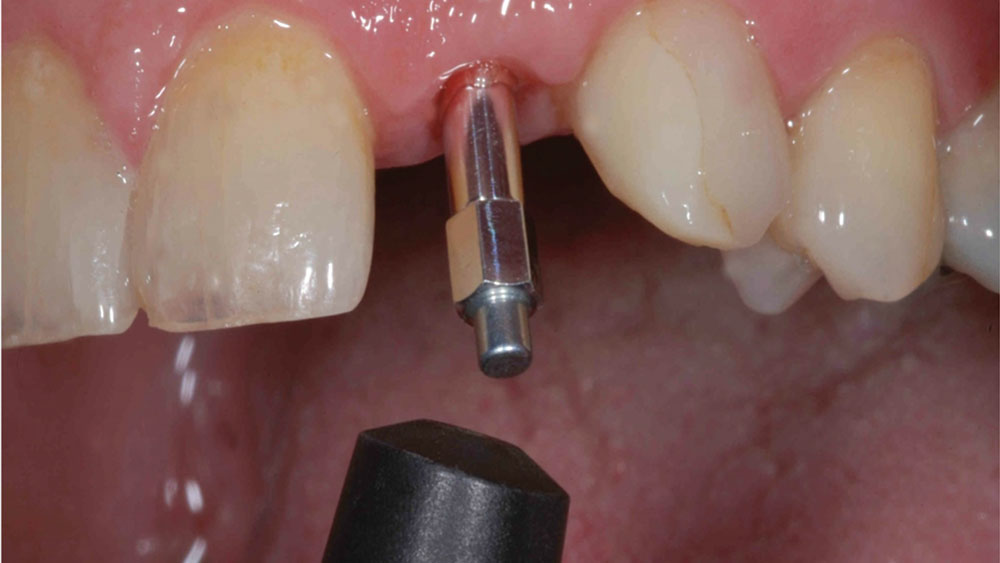
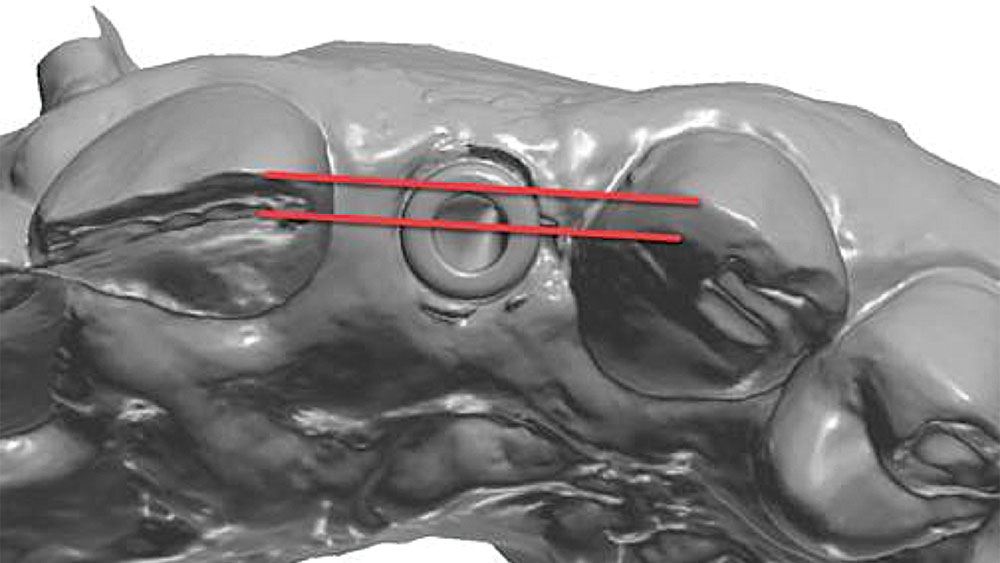
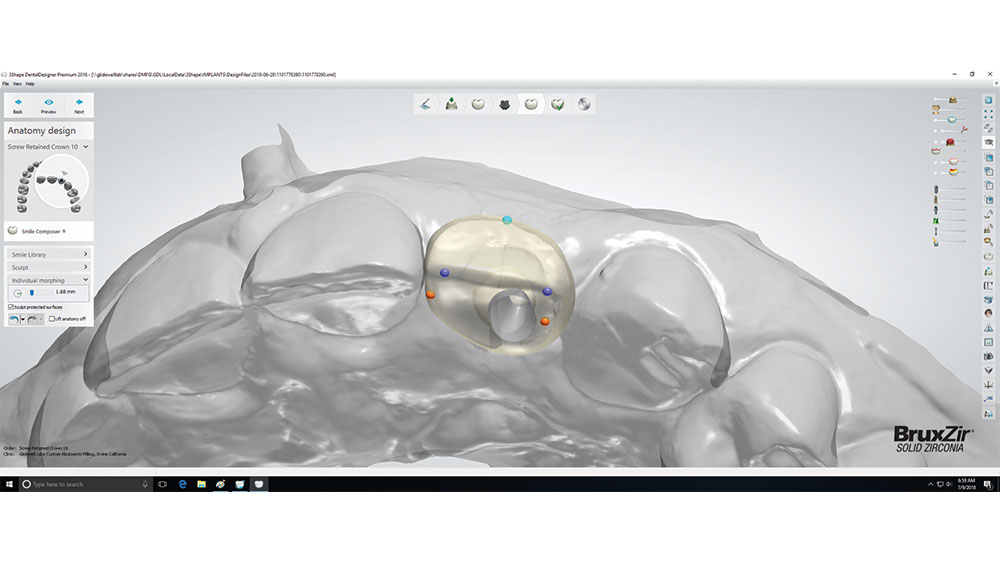
To achieve an optimal functional and esthetic outcome, the implant must be placed correctly with regard to trajectory, adjacent vital anatomy, and buccolingual, apicocoronal and mesial-distal positioning. Situating the implant so that the edges of the osteotomy are at least 2 mm from the buccal and lingual cortical plates, 2 mm from adjacent roots, 2 mm from vital structures, and 2–3 mm below the crest of tissue will keep the implant within the envelope of acceptability. The implant trajectory should emerge lingual to the incisal edge of the planned restoration, which allows for a screw-retained crown.
IMPLANT PLACEMENT PARAMETERS
- 2 mm of bone buccal and lingual to the osteotomy
- 2–3 mm subgingival to the crest of tissue
- Angulation lingual to the incisal edge
- 2 mm from adjacent teeth and vital structures
RESTORATIVE CONSIDERATIONS
Most patients desire an esthetic result when viewed with a mirror at a 10-inch distance. Placing an implant in a grafted, healed extraction site typically allows for the natural tissue tone and texture patients desire, as well as the keratinized soft tissue needed to fill the embrasures and avoid black triangles around the restoration. Achieving proper apicocoronal implant positioning as described above helps avoid any visible metal at the gum line. It’s also important to choose a ceramic material that blends well with the color, contours and texture of adjacent teeth.
ESTHETIC GUIDELINES FOR THE FINAL RESTORATION
- Natural tissue tone and texture
- Absence of black triangles and metal at the gum line
- Esthetic result from 10-inch distance
- Ceramic material choice: color, contour and texture
CASE REPORT
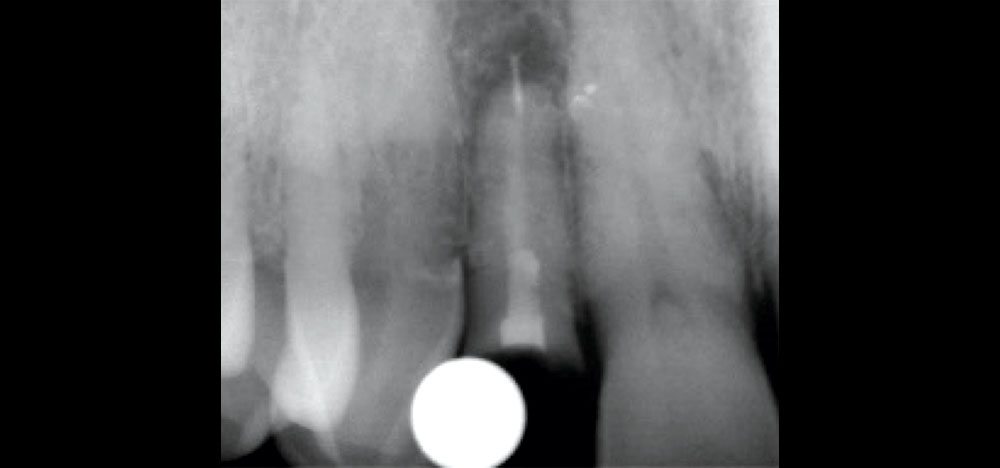
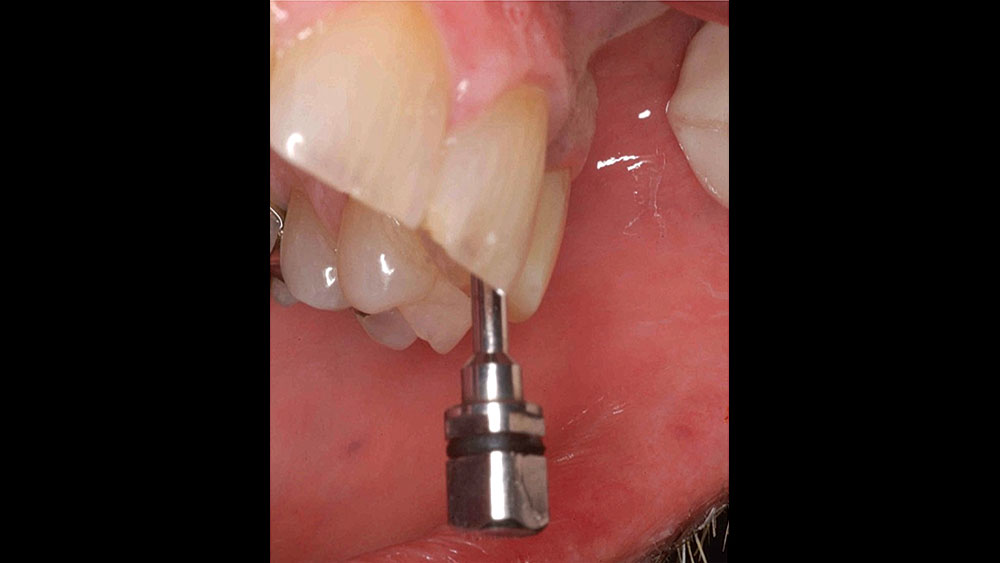
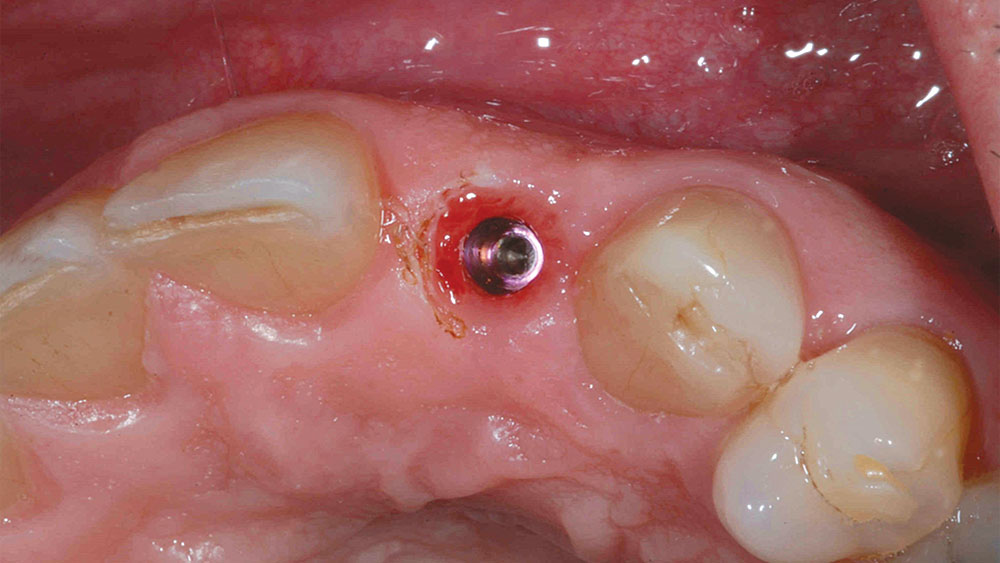
This case is an example of an ideal clinical situation for dentists who are new to placing implants in the esthetic zone. The patient requested treatment for a fractured upper lateral incisor. After extraction, grafting and healing, ample bone and soft tissue were present, and an implant was placed in optimal position for an esthetic result. The screw-retained restoration predictably restored form and function, illustrating the beautiful results that can be achieved by observing simple surgical and prosthetic guidelines.
CONCLUSION
Implant placement in the esthetic zone is well within the ability of the dentist who has mastered the posterior and is ready to expand the services offered by his or her practice. By carefully selecting and diagnosing the case, practicing restorative-driven treatment planning, and adhering to proven surgical principles, a predictable result is achieved that satisfies the expectations of doctor and patient alike.