Seven Things You Need to Know About Sleep and Airway Health

I have yet to meet a patient who doesn’t want to experience a great night’s sleep. In my practice, it’s routine to discuss sleep and airway health with my patients, who often admit to a lack of energy or excessive daytime sleepiness during our consultation. This conversation is the first step in helping those who suffer from sleep-disordered breathing. Receiving treatment has the potential to greatly improve a patient’s health and ability to enjoy life.

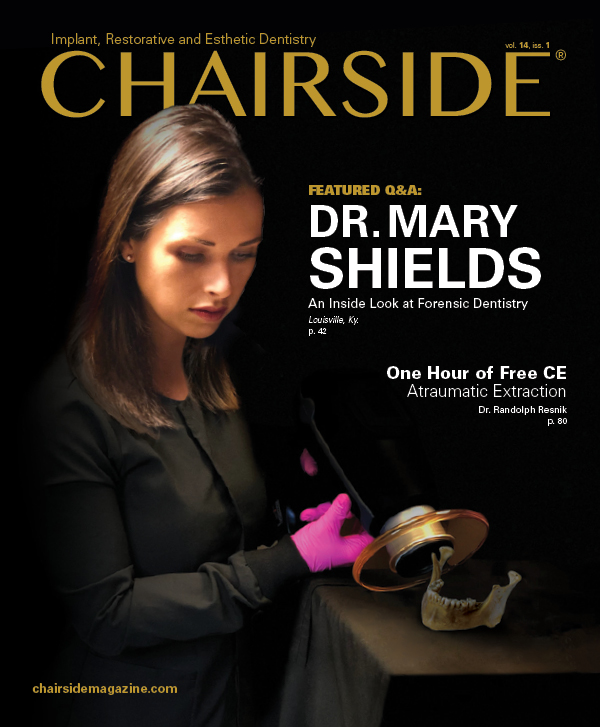
Oral appliance therapy can improve your patients’ quality of life, as they experience more energy during the day.
On both a professional and personal level, there are many benefits to expanding the dental practice to treat patients who suffer from snoring and obstructive sleep apnea (OSA). Here are seven things you should know to become involved in sleep dentistry and grow your practice:
1. PATIENTS IN YOUR PRACTICE MAY BE IN NEED OF ORAL APPLIANCE THERAPY AND NOT KNOW IT.
Approximately 22 million people suffer from sleep apnea in the U.S.,1 and an estimated 90 percent of OSA cases are undiagnosed.2 According to a study conducted by the CHEST Foundation, 26 percent of participants who took a Berlin questionnaire, a subjective survey, were at high risk of experiencing undiagnosed sleep apnea.3 This means, in a dental practice with 2,100 patients of record, approximately 546 individuals could be at high risk of undiagnosed sleep-disordered breathing.
2. OSA IS A MEDICAL CONDITION WITH A DENTAL SOLUTION.
Because OSA is a medical condition, patients can be treated after receiving a diagnosis from a board-certified sleep physician via an attended overnight sleep study (polysomnogram) or a home sleep test. After receiving a diagnosis, patients can be advised of various treatment options, including continuouspositive airway pressure (CPAP), oral appliance therapy, a combination of CPAP and oral appliance therapy, or surgical procedures.
APNEA-HYPOPNEA INDEX (AHI)
Provided as a result of a sleep test, the apnea-hypopnea index is the combined average number of apneic and hypopneic events that occur during sleep, and is used to assess the severity of sleep apnea.
Mild OSA: 5–15 events per hour
Moderate OSA: 15–30 events per hour
Severe OSA: Greater than 30 events per hour
3. OSA CAN BE EXPLAINED TO PATIENTS EASILY WITH A CORK AND STRAW ANALOGY.
Results from a sleep study will reveal your patient’s apnea-hypopnea index (AHI). The AHI can be explained to patients simply by using an analogy of corks and straws. For example, I explain to patients that an apneic event is like having a cork in the airway, which prohibits breathing. That cork in the airway for 10 seconds or longer is considered an apneic event. I tell patients, “When I say apnea, think of a cork.” Hypopnea is shallow breathing for 10 seconds or longer. I instruct patients to imagine breathing through a straw for 10 seconds or longer; this is considered a hypopneic event, or hypopnea.
When I explain the sleep study in terms of corks and straws, I tell patients: “We look at the number of corks you had and the number of straws you had, add them together, and divide by the total number of minutes you slept. That’s called the AHI or apnea-hypopnea index.” I then further discuss the patient’s sleep study. For example, if the sleep study reveals that the patient had an AHI of 25, this indicates the individual had 25 events (corks and straws) per hour, and the severity of the disease is then derived. Note that 5–15 events per hour is mild OSA, 15–30 events per hour is moderate OSA, and greater than 30 events per hour is severe OSA. Therefore, an AHI of 25 would mean the patient suffers from moderate OSA. When you explain OSA in this manner, patients are able to easily understand the disorder.
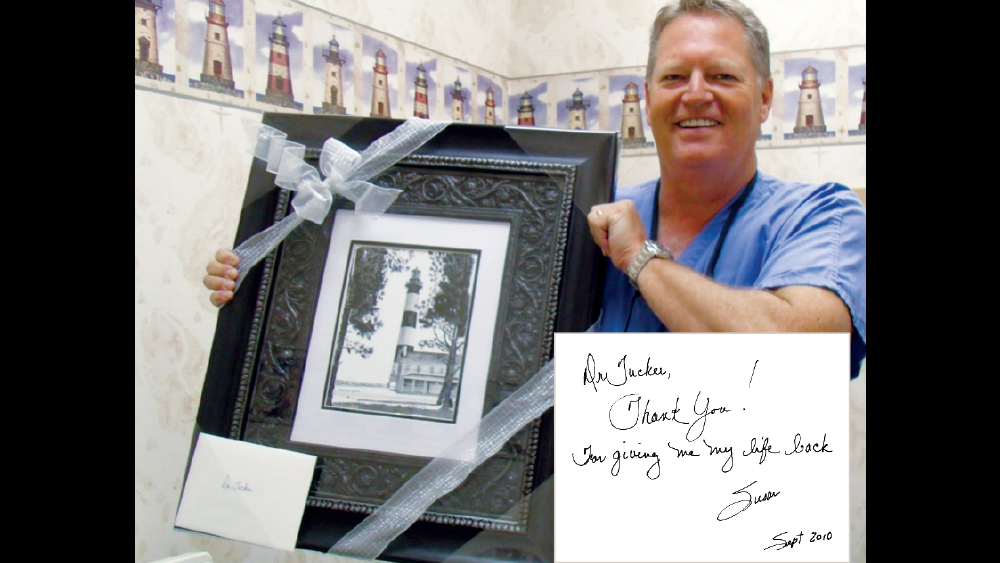
Dr. John Tucker received a framed, original painting from his patient Susan. She presented the gift in appreciation for the life-changing results she has enjoyed due to oral appliance therapy.

Dr. Tucker believes sleep dentistry is most successful when dentists employ a team-driven approach, and his courses teach strategies for communicating a unified message to patients.
4. IT’S NOT DIFFICULT; IT’S JUST DIFFERENT.
Treating patients with an oral appliance is not difficult. It’s not like performing a full-mouth reconstruction. Sleep-disordered breathing uses different terminology that may at first seem unfamiliar — like learning new vocabulary during those first days in dental school. But it’s not difficult; it’s just different.
5. SLEEP DENTISTRY IS A PRACTICE CHANGER.
When you give a patient back a smile, it’s an important and rewarding part of the profession. But when you shift the focus to sleep and airway health, you give patients back their life. For example, I’m reminded of a patient, Susan, who was referred to my office by a board-certified sleep physician as being PAP-intolerant (i.e., unable to use positive airway pressure for treatment of OSA). Prior to oral appliance therapy, she had been unable to walk up and down her driveway. After six months of treatment with an oral appliance, she returned to my office to report that she was now able to ride her new bike around a 17-mile loop. There was also an extreme decrease in blood pressure, as well as weight loss of 60 pounds. She had tears in her eyes when she said, “Thank you for giving me my life back.”

Dr. Tucker demonstrates how to take a proper bite for an oral appliance.
6. INVESTING IN YOUR TEAM GOES A LONG WAY.
Sleep dentistry doesn’t require a large investment in office equipment. However, you will need to invest in your team and in yourself. Sign up for courses that teach you how to successfully implement dental sleep medicine into your practice, and learn strategies for communicating a unified message to patients. Sleep dentistry is 95 percent team-driven, and a cohesive message will help encourage patients’ acceptance of treatment. In addition, learn how to successfully screen patients for sleep-disordered breathing, work with physicians, choose the proper sleep appliance, and receive support from the dental lab.
7. PATIENTS READILY ADAPT TO ORAL APPLIANCE THERAPY.
It’s my experience that patient compliance and acceptance of oral appliance therapy is nearly 100 percent. That said, there are certain considerations for selecting the proper appliance for the patient’s situation. For example, choose an FDA-cleared device, such as the Silent Nite® sl (Glidewell Laboratories; Newport Beach, Calif.) or EMA® (Frantz Design Inc.; Austin, Texas), that provides ample room for excursive movements, has proper strength and durability, is low-volume in the oral cavity, and allows the tongue to move out of the airway.

Dentists can utilize the Sleep Device Sample Kit (Glidewell Direct; Irvine, Calif.) to inform patients about the treatment of sleep-disordered breathing.
CONCLUSION
Sleep dentistry is a field that I encourage all dentists to learn more about — for the good of your patients as well as the growth of your practice. In my experience, dental sleep medicine has been an advantageous component of my practice, and many doctors who have become involved in sleep dentistry have expressed how much they enjoy building their practice with a service that offers so many benefits, including the opportunity to assist our medical colleagues in providing life-changing treatment for patients.
References
- ^Sleep apnea information for clinicians [internet]. Washington, D.C.: American Sleep Apnea Association; c2017 [cited 2018 Nov 5]. Available from: https://www.sleepapnea.org/learn/sleep-apnea-information-clinicians.
- ^Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997 Sep;20(9):705-6.
- ^Hiestand DM, Britz P, Goldman M, Phillips B. Prevalence of symptoms and risk of sleep apnea in the U.S. population: Results from the national sleep foundation sleep in America 2005 poll. Chest. 2006 Sep;130(3):780-6.