Aligning Patients’ Esthetic and Financial Goals

For so many of our patients, recent months have been challenging on both a personal and financial level. Patients still want the dentistry that will make them feel confident about their smiles, but, for many, finances have constricted due to the economic consequences of COVID-19. Despite payment options that may be available, many patients are simply unable to afford ceramic veneers and other first-choice esthetic treatment. Flexibility in determining patient treatment plans is one of the keys to success during this recovery, so how then can we deftly scale our treatment options to suit a range of budgets? When it comes to esthetic dental needs, I would like to propose three options.
SMILE TRANSITIONS™
The Smile Transitions™ cosmetic appliance, which simply fits over existing teeth, is an affordable option that can benefit patients who want near-immediate results for minimal cost and effort. After one appointment for impressions or scans, they can return to the office about a week later to receive their Smile Transitions. No tooth preparation or cementation is required. And, for patients who desire to do so, the appliance can be worn while eating and drinking.
In addition to the dramatic esthetic improvement, patients find the results to be motivational. Wearing Smile Transitions provides a glimpse of what’s possible, from filling in missing teeth to rejuvenating a stained, worn smile. Patients can enjoy full, albeit temporary, smile makeovers at a fraction of the top-tier cost, and still look forward to more definitive esthetic treatment when finances improve.
CASE STUDY




A complex treatment plan is needed to improve this patient’s smile. For a temporary, affordable transformation, her doctor delivered Smile Transitions. – Clinical dentistry by Taylor Manalili, DDS
DIRECT BONDING (DIRECT COMPOSITE VENEERS)
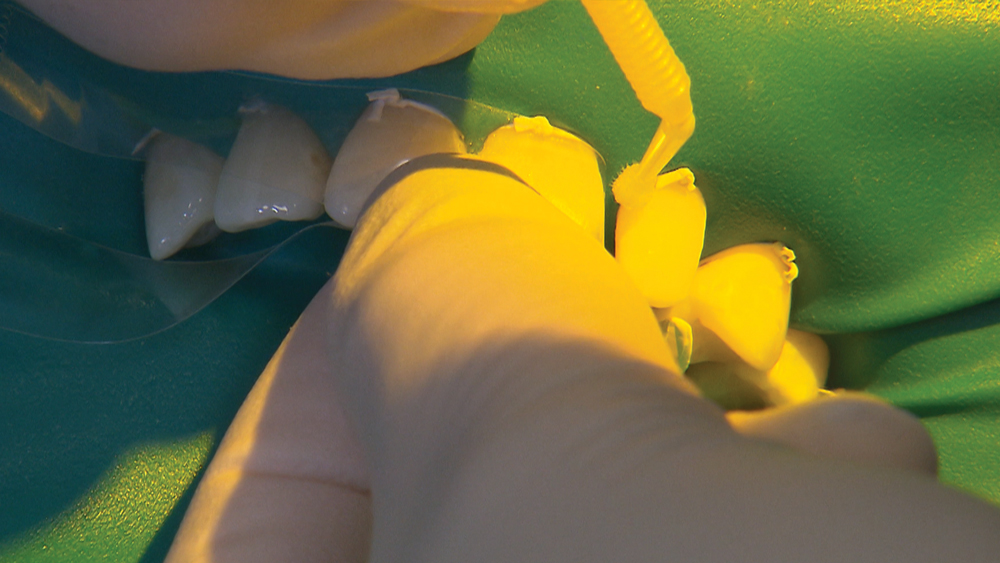
Direct composite veneers can also provide an interim option that is budget-friendly and provides many of the esthetic benefits of ceramic veneers. The esthetic outcome is highly dependent on clinical execution, as direct bonding is technically demanding. However, this option is still very cost-effective and convenient, requiring just one or two appointments.
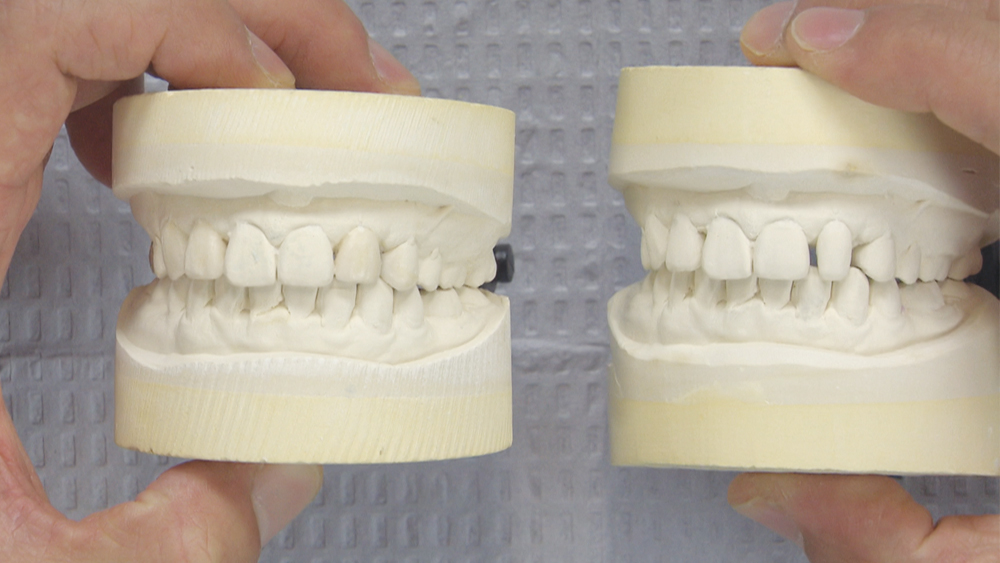
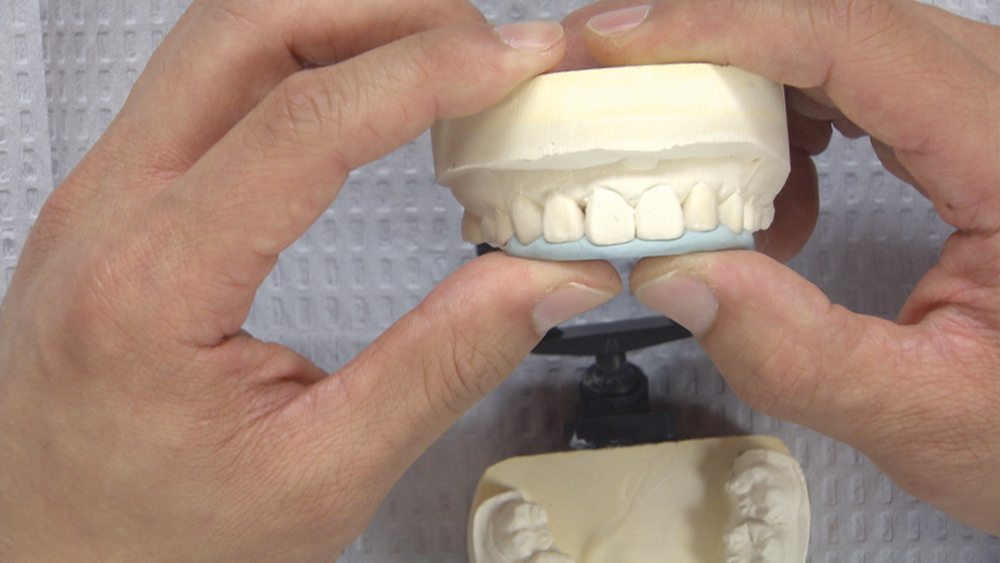
For cases of 1–2 units, I like to do direct bonding in a single appointment. For cases of more than 2 units, I advise using diagnostic wax-ups, which can be created on-site or ordered from the lab. When a diagnostic wax-up is used, the full process for direct composite veneers includes a treatment-planning appointment, an optional second appointment to review the diagnostic wax-up and mock-up, and the final appointment for the direct bonding procedure.
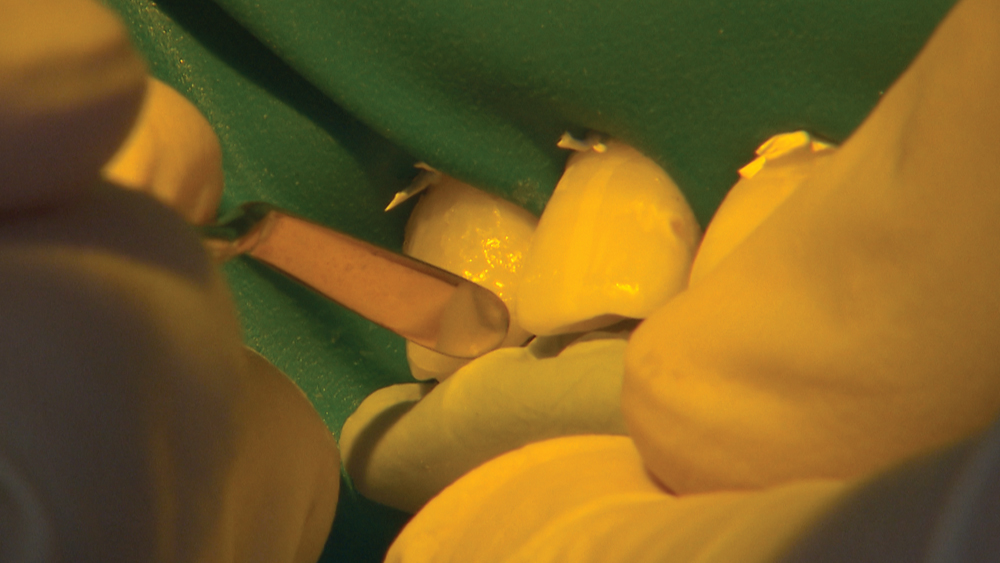
CASE STUDY
CERAMIC VENEERS
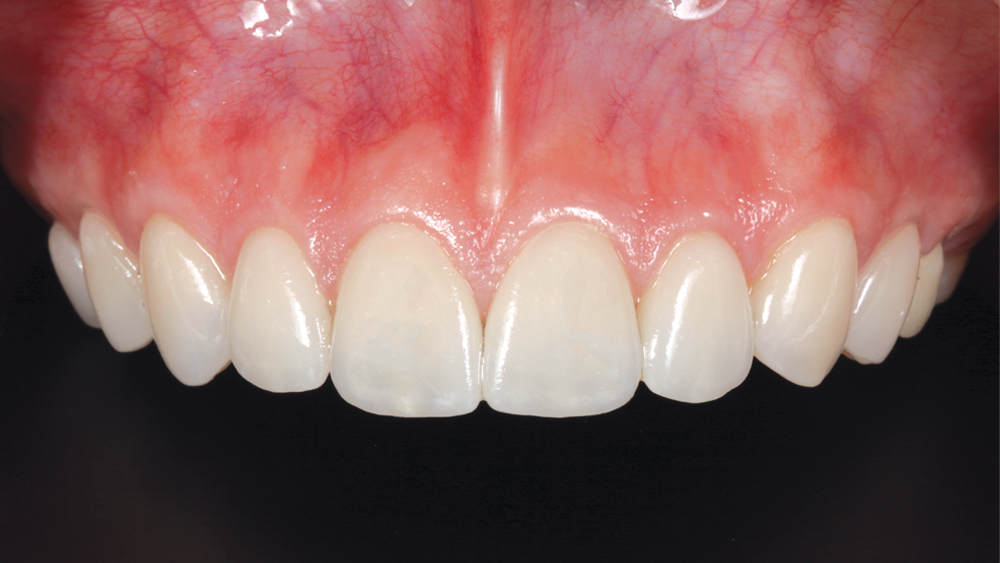
Assuming the patient’s teeth do not require full-coverage restorations, ceramic veneers are the premier option that I propose when patients can afford to make a substantial investment in their smiles. Ceramic veneers offer the most ideal esthetics and stability. Plus, ceramic veneers allow the greatest range for improving the shape and color of teeth.
When I am choosing veneer materials, I prescribe based on an occlusal analysis. In the absence of parafunctional habits, I order Obsidian® lithium silicate ceramic, which provides fantastic translucency and shade. And for those veneer cases that demand extra strength, my material of choice is BruxZir® Esthetic Zirconia.
In addition to these proven materials, I rely on diagnostic wax-ups for planning the case. This step enables me to successfully communicate my vision for the case to my lab team. And when I’m chairside, the diagnostic wax-up is indispensable for patient communication and motivation. All around, I view diagnostic wax-ups as the best way to eliminate surprises and stay in sync with my patients and lab team for esthetic success.
CASE STUDY
CONCLUSION
As dentists, we always prefer to render the ideal treatment. However, particularly in times such as these, it’s not just about precise clinical techniques. We must stay attuned to patients’ financial priorities and be ready to advise them on a spectrum of restorative options that will provide them with the esthetic benefits they are seeking.