The Partial-Arch Implant Prosthesis: When, Why and How

When your partially edentulous patient presents with an edentulous span of five units or more, the partial-arch implant restoration is an excellent option that can fully restore form and function. The challenge in designing this type of restoration is typically related to the volume and type of tissue that must be replaced. According to the Misch classification, there are three types of fixed prostheses: FP-1, FP-2 and FP-3.11 The FP-1 is an implant restoration that replaces only the crown portion of the missing teeth. An FP-2 prosthesis restores the crown as well as portions of the root, resulting in teeth that are usually longer than normal. The FP-3 restoration includes a gingiva-colored portion, replacing areas of the soft tissue in addition to the missing teeth.
Fixed Prosthesis Classifications According to the Misch Institute
FP-1: Replaces teeth with anatomy similar to natural crowns
FP-2: Replaces crown and portions of the root, resulting in elongated teeth
FP-3: Replaces crowns and soft-tissue areas
For the purposes of this article, we will focus on cases where the patient has experienced hard- and soft-tissue loss in the edentulous area, requiring an FP-3 implant prosthesis.
After determining that the FP-3 prosthesis is the optimal solution, the clinician must work with the patient in deciding whether to preserve the remaining teeth. The health and long-term prognosis of the remaining teeth must be considered as well as whether the patient is happy with the appearance of their teeth. If there is periodontal disease or caries involving the remaining teeth, or the patient prefers the uniform esthetics of a full-arch restoration, extraction followed by full-arch implant treatment may be the best way forward. Conversely, if the remaining teeth are healthy, preserving the dentition is a conservative approach to treatment that some patients prefer and also makes it easier to maintain the vertical dimension of occlusion (VDO).
The Partial-Arch Implant Prosthesis Is Recommended for:
Edentulous spans of 5 units or more
Cases where an FP-3 prosthesis is indicated due to hard- and soft-tissue loss
Partially edentulous patients with healthy dentition adjacent to implant sites
Patients who are happy with the esthetics of their remaining natural teeth
Cases where the prognosis of the remaining teeth is very good
CASE REPORT
Due to its exceptional strength and stunning esthetics, the BruxZir® Esthetic Implant Prosthesis (Glidewell; Irvine, Calif.) has become my restoration of choice in these situations. In this case report, I’ll show an example of a patient for whom this restorative solution is recommended. The case involves a longstanding patient who had been wearing a removable partial denture spanning teeth #4–11 for over two decades, and decided she wanted a fixed restoration to improve her oral health, comfort and quality of life. She expressed a strong desire to keep her remaining maxillary teeth, which were healthy and showed no signs of caries or periodontal disease. The patient accepted a treatment plan in which four implants would be placed to support a partial-arch restoration fabricated from BruxZir Esthetic Zirconia — a process eased by Glidewell’s streamlined restorative protocol.


Figures 1a, 1b: At the initial consultation, the patient complained of her removable partial denture, desiring a fixed restoration that looked and felt more like natural teeth and would allow her to eat normally and smile without worrying about her prosthesis becoming loose. Because the patient’s remaining teeth were healthy and a conventional bridge was not an option, the patient agreed to receive four implants to support an FP-3 prosthesis, which would replace the missing teeth as well as the lost hard and soft tissue in the edentulous span.
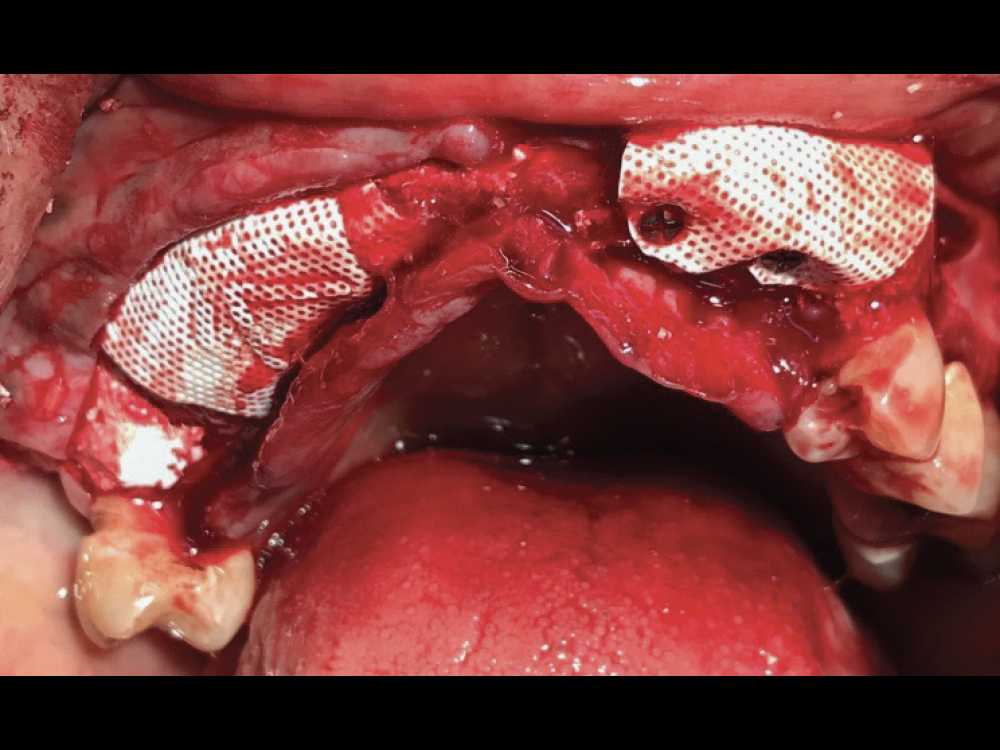
Figure 2: Treatment began with horizontal guided bone regeneration to widen the ridge between the patient’s healthy maxillary teeth. Alveoplasty was performed to level the bone, the ridge was grafted with a 50-50 blend of cortico-cancellous allograft and bovine-derived xenograft, and dense polytetrafluoroethylene (d-PTFE) membranes were positioned and held in place with fixation screws. The surgical flap was closed with interrupted sutures, and the patient left the appointment wearing a partial appliance, with a relieved intaglio surface in the grafted area.
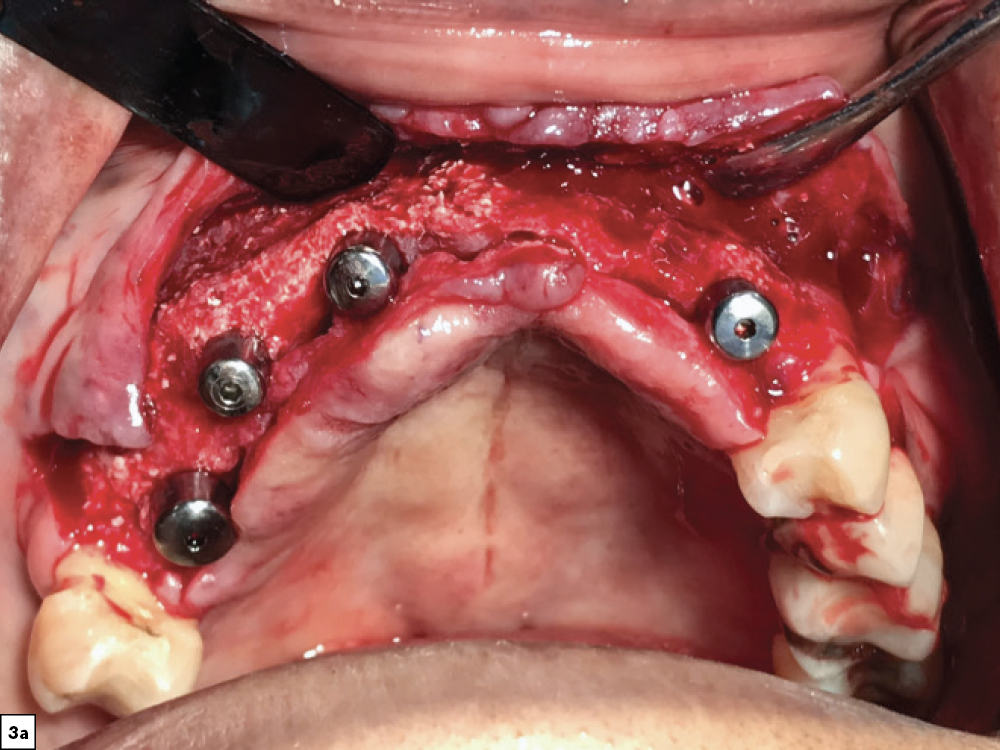
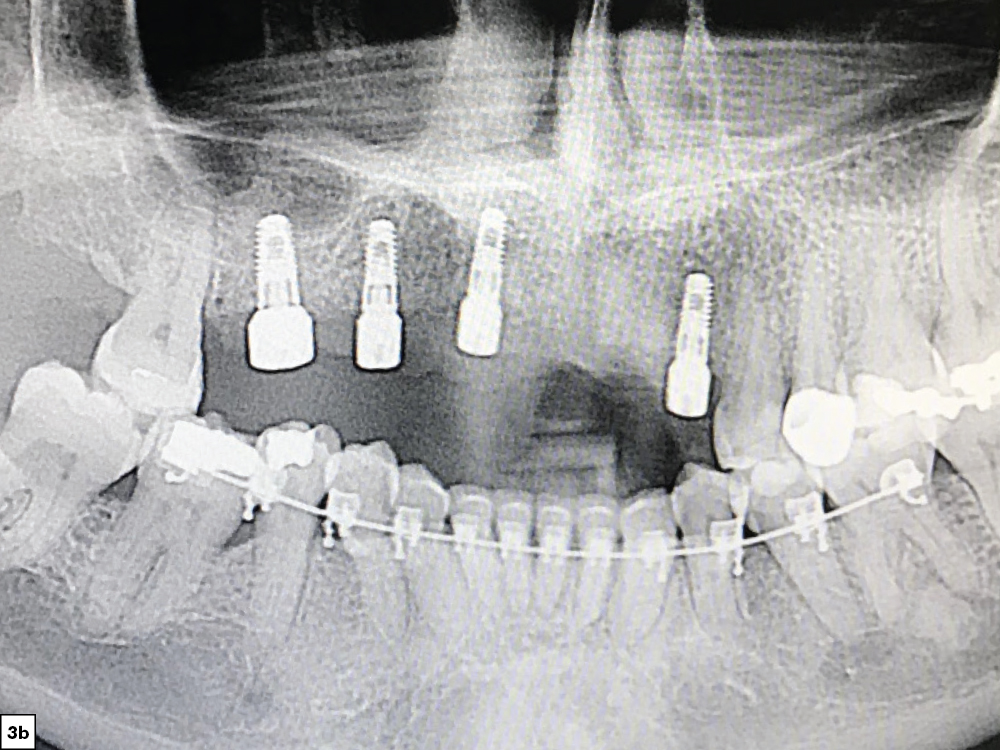
Figures 3a, 3b: After four months of healing, the patient returned for evaluation and exhibited sufficient bone volume for implant placement. After reflecting a full-thickness periosteal flap with vertical releasing incisions, four implants were placed. Healing abutments were connected to the implants, additional grafting material was placed and the surgical flap was sutured.

Figure 4: Three months after implant placement, the patient returned, and a screw-retained provisional implant prosthesis was fabricated chairside using non-engaging abutments, flowable acrylic, a vacuum thermoforming machine and the patient’s existing partial denture as a template. Orthodontic treatment was undertaken for the lower arch to intrude the supererupted mandibular teeth and level the occlusal plane.

Figure 5: One month later, a preliminary impression was made using the closed-tray technique and medium-body VPS material, beginning the restorative process for the BruxZir Partial-Arch Implant Prosthesis. The impressions were sent to the lab along with photos of the patient and a duplicate of the patient’s existing appliance.
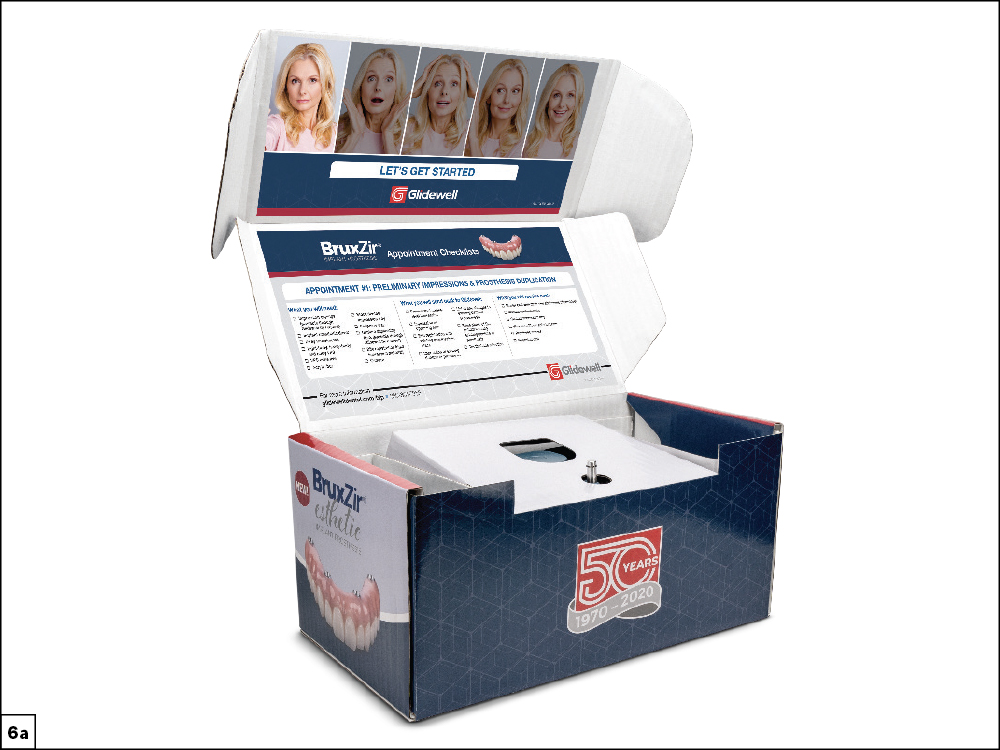

Figures 6a, 6b: Restoration fabrication went smoothly and efficiently thanks to the new and improved clinical workflow recently implemented at Glidewell, which includes step-by-step instructions, checklists and “how to” videos that simplify each appointment. Multi-unit abutments provided by the lab were connected to the implants and eased the seating of try-ins by elevating the restorative platform above the tissue level. The angled 17-degree multi-unit abutments ensured that the screw access holes would be located in the palatal areas of the restoration.

Figure 7: An implant verification jig (IVJ) was connected to the implants and splinted together using cold-cure acrylic. The lab provides an IVJ for the final impression to make sure that the partial-arch restoration seats passively without putting strain on the implants.

Figure 8: The lab also included a custom tray for the final impression over the IVJ. After seating the tray to make sure the guide pins of the IVJ emerged through the holes in the tray, the final impression was made and sent to the lab for the fabrication of a wax try-in.

Figure 9: The wax setup was tried in and evaluated according to the step-by-step checklist included with the case. Adjustments were made to correct for overjet and fine-tune the occlusion.

Figure 10: The lab scanned the approved wax setup and designed the implant prosthesis using advanced CAD/CAM technology. A provisional implant prosthesis was 3D-printed for clinical and patient verification. We asked the patient to wear the provisional for two weeks to get input from her loved ones, confirm proper function when chewing food and talking, and make sure it was comfortable. She asked for darker gingival-tissue and tooth shades, which I relayed to the lab technician in the final prescription. Minor chairside adjustments were made for occlusion, and the provisional was returned to the lab for fabrication of the final restoration. The provisional proved to be a valuable tool in ensuring the patient was happy with the final outcome.
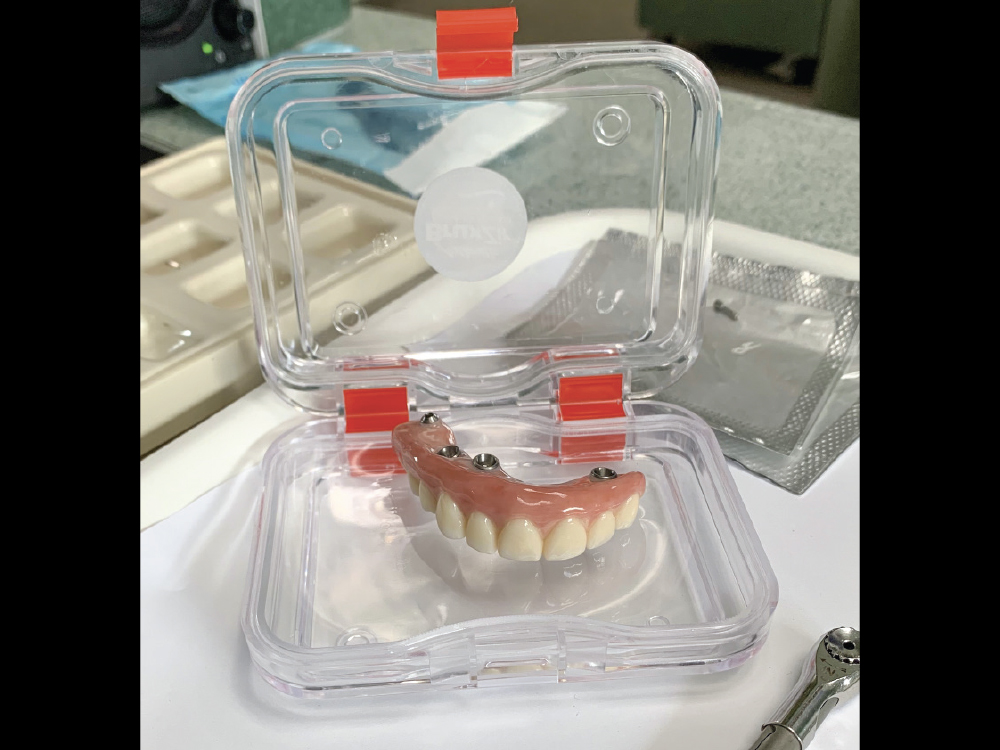
Figure 11: The lab scanned the provisional to capture the occlusal adjustments in the final restoration design, and the partial-arch implant prosthesis was milled from BruxZir Esthetic. Fabricated from 870 MPa monolithic zirconia, this new formulation of the BruxZir Implant Prosthesis is warrantied for life and combines premium esthetics with exceptional durability, avoiding the chipping and fractures of the porcelain or acrylic used in other types of premium FP-3 prostheses.

Figure 12: At the final delivery appointment, the BruxZir Esthetic Partial-Arch Implant Prosthesis was seated. We checked the occlusion, contacts, lateral excursions and phonetics, and everything was exactly as expected. The patient was extremely happy with the lifelike esthetics of the restoration and enjoys the ability to eat and smile with confidence.


Figures 13a, 13b: Before-and-after images illustrate the dramatic transformation we were able to provide for the patient through implant dentistry and the use of BruxZir Esthetic Zirconia.
CONCLUSION
The partial-arch implant prosthesis is a viable solution for patients who desire a fixed implant restoration and have healthy teeth adjacent to a long edentulous span. This solution allows for a conservative approach to treatment and avoids the problems associated with removable partial dentures. And by fabricating the restoration from BruxZir Esthetic Zirconia, we can provide patients with beautiful restorations they can depend on for life.
LEARN MORE
For more information about the BruxZir Implant Prosthesis, visit glidewelldental.com/bip.