Removable and Fixed Solutions for the Edentulous Patient

The fully edentulous patient faces many challenges, including diminished chewing capability and compromised speech function, as well as social and psychological issues, that combine to create a negative impact on quality of life.1 Thankfully, modern dentistry affords the clinician a range of options for successful treatment of the edentulous patient, from the traditional complete denture to the fixed monolithic zirconia full-arch implant restoration. Depending on the oral condition and financial circumstances of the patient, a treatment plan can be developed that addresses the unique challenges of each case. While some cases require a fixed or removable implant solution to effectively restore function, a well-designed complete denture can meet the needs of others.
Studies have shown that fixed full-arch implant restorations offer the highest levels of prosthetic stability, function, satisfaction and quality of life for the edentulous patient.2,3,4 However, patients with favorable anatomical features can often be provided with a relatively stable conventional denture, particularly in the maxilla. Upper dentures with palatal coverage can usually achieve sufficient retention and function.5 When a patient requires full-mouth rehabilitation but only can afford implant therapy for one arch, an implant solution is typically recommended for the mandible, where it’s more difficult to establish a stable and retentive complete denture.
By comprehensively assessing the patient’s chief complaint, bone volume, anatomical landmarks, and the fit, stability and comfort of any existing oral appliances, clinicians can confidently determine whether a traditional complete denture or an implant-supported prosthesis is indicated. After presenting the treatment options, doctors can work with the patient in developing a solution that is both affordable and effective.
CASE REPORT
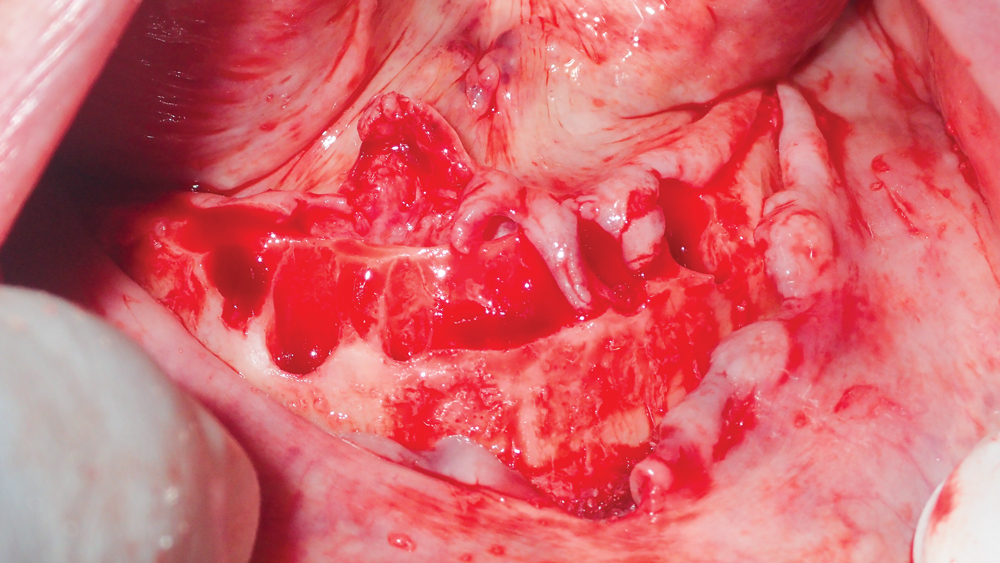
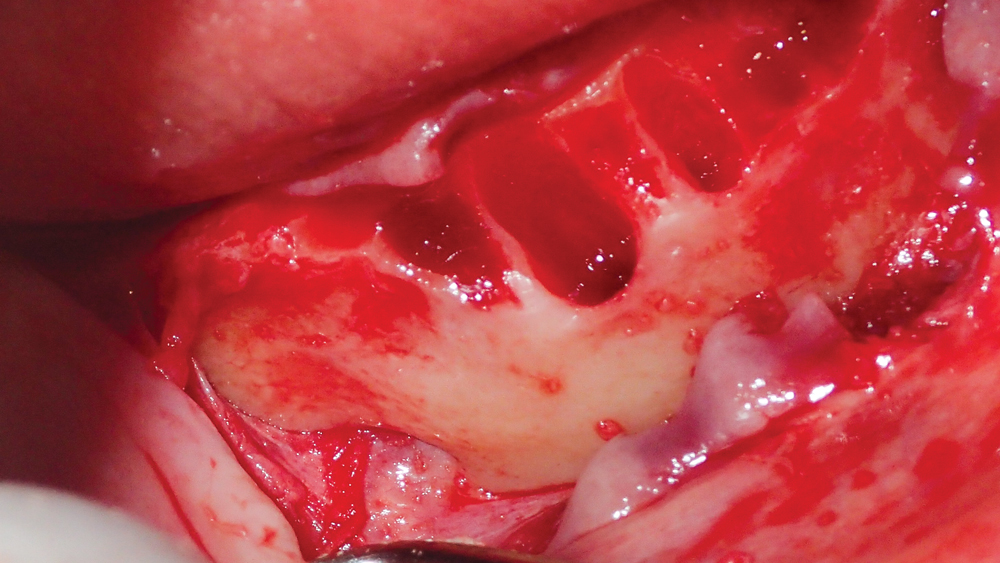
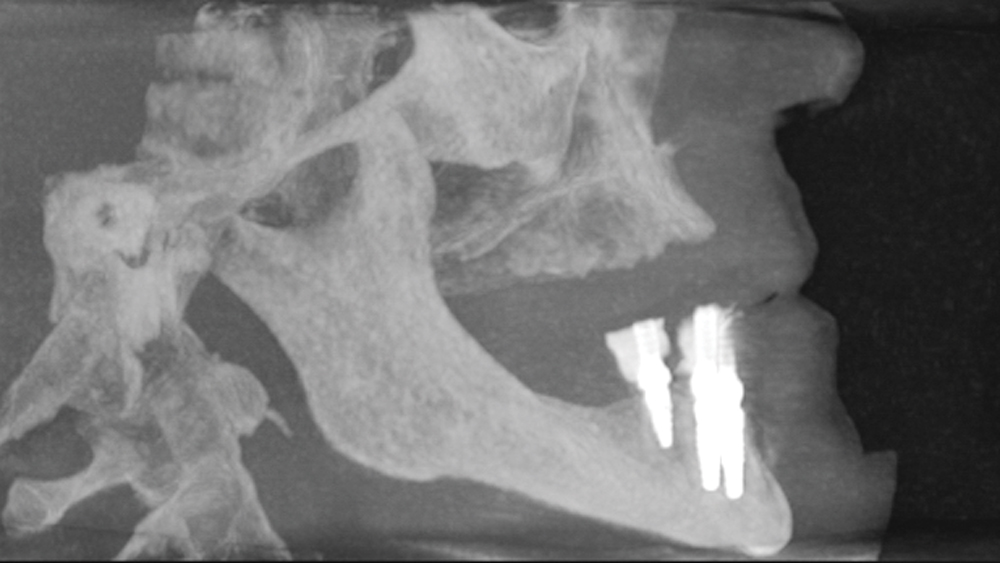
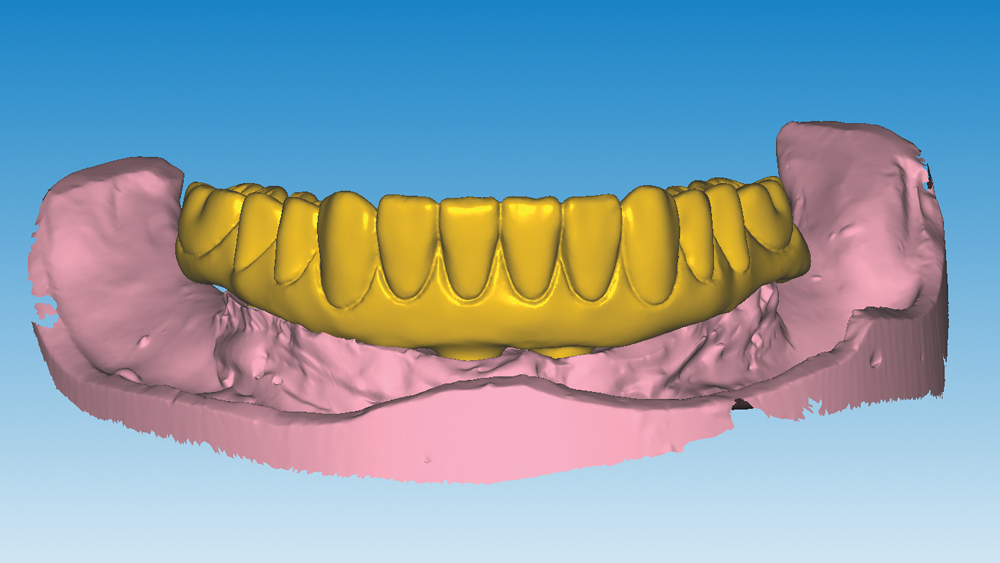
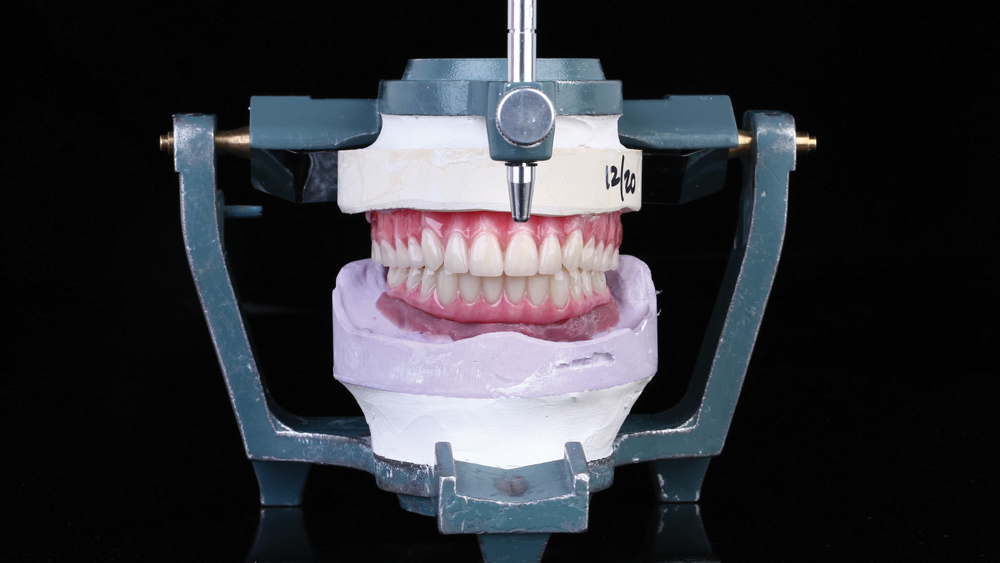
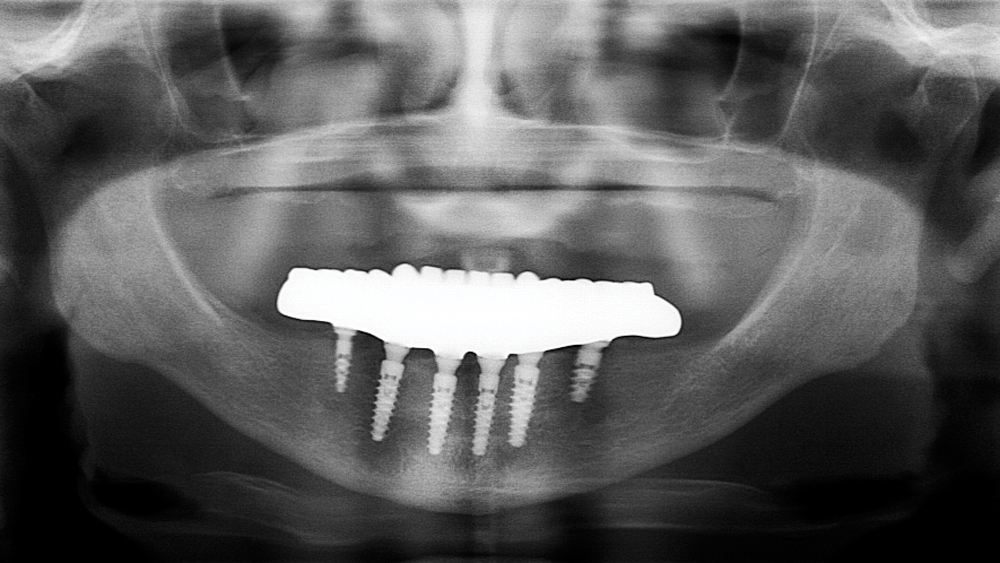
This patient was unhappy with the esthetics of her existing upper denture as well as the discomfort and instability caused by her loose-fitting mandibular partial denture. Although her concerns with the maxillary denture could be addressed with a new, more esthetic appliance, she preferred implant treatment for her mandible, where a fixed solution was needed to adequately restore function, stability and comfort.
Treatment plan:
- Upper: Full denture
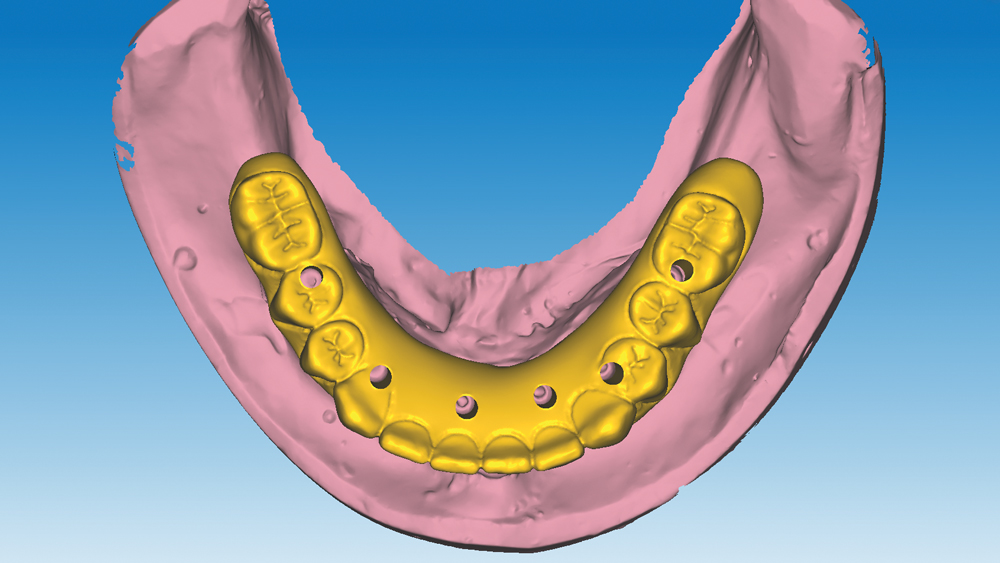
- Lower: Fixed BruxZir® Full-Arch Implant Prosthesis
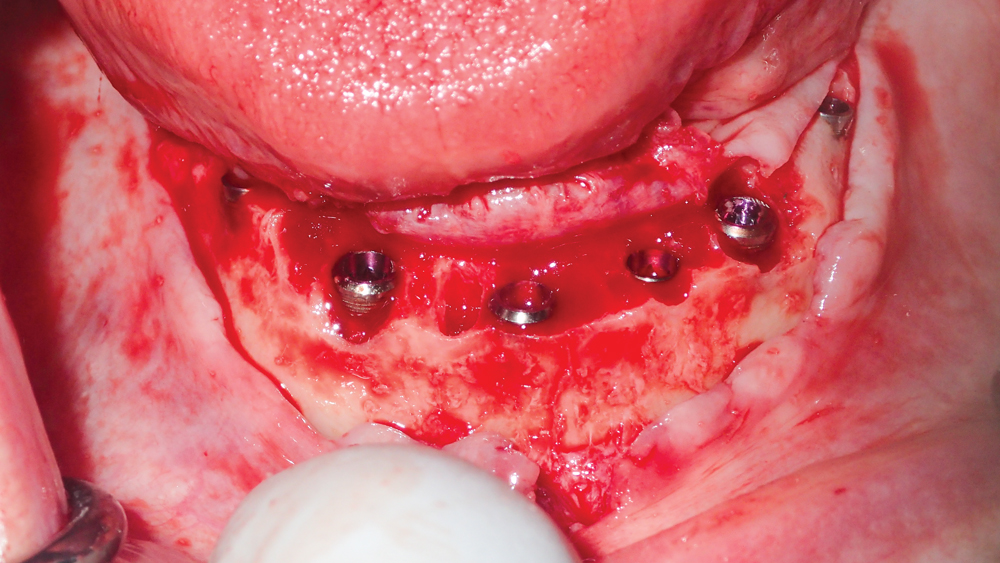
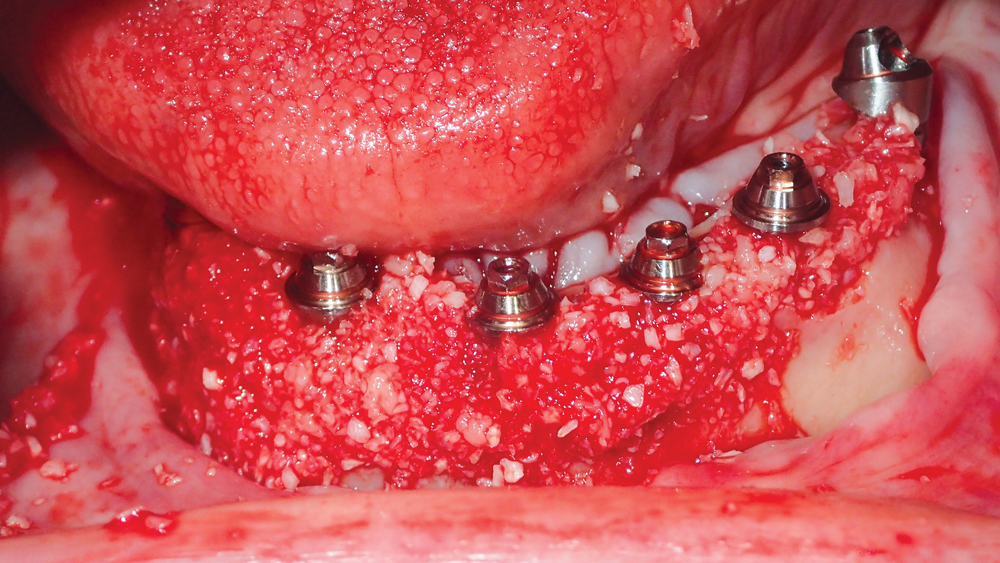
The patient’s remaining mandibular teeth were extracted followed by immediate implant placement and delivery of a fixed provisional appliance. After integration of the implants, the prosthetic designs for the new upper denture and lower implant restoration were determined in tandem. Ultimately, the dual-arch restorations addressed the functional and esthetic challenges of the case while staying within the financial means of the patient, demonstrating the benefits of a flexible, multifaceted approach to restorative dentistry.
The dual-arch restorations addressed the functional and esthetic challenges of the case while staying within the financial means of the patient.
CONCLUSION
When providing treatment for the edentulous arch, the ability to offer traditional removable dentures as well as implant-supported prostheses affords the flexibility required to address the various needs of patients. By carefully considering the oral health, anatomy and financial circumstances of each case, clinicians can devise a treatment plan that effectively restores form and function within the budget of the patient.
Available CE Course
References
- ^Zembic A, Wismeijer D. Patient-reported outcomes of maxillary implant-supported overdentures compared with conventional dentures. Clin Oral Implants Res. 2014 Apr;25(4):441-50.
- ^Turkyilmaz I, Company AM, McGlumphy EA. Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology. 2010 Mar;27(1):3-10.
- ^Brennan M, Houston F, O’Sullivan M, O’Connell B. Patient satisfaction and oral health-related quality of life outcomes of implant overdentures and fixed complete dentures. Int J Oral Maxillofac Implants. 2010 Jul-Aug;25(4):791-800.
- ^Preciado A, Del Río J, Lynch CD, Castillo-Oyagüe R. Impact of various screwed implant prostheses on oral health-related quality of life as measured with the QoLIP-10 and OHIP-14 scales: a cross-sectional study. J Dent. 2013 Dec;41(12):1196-207.
- ^Misch CE. Contemporary implant dentistry. 3rd ed. St. Louis: Mosby; 2007. p. 367.
- ^Colomina LE. Immediate loading of implant-fixed mandibular prostheses: a prospective 18-month follow-up clinical study–preliminary report. Implant Dent. 2001;10(1):23-9.
- ^Najafi H, Siadat H, Akbari S, Rokn A. Effects of immediate and delayed loading on the outcomes of all-on-4 treatment: a prospective study. J Dent (Tehran). 2016 Nov;13(6):415-22.