BruxZir® Screw-Retained to the Rescue

For the anterior zone, where the patient’s primary concern for esthetics is focused, implant manufacturers have developed comprehensive tools and components to promote the desired results. However, commonly with these systems, there is a trade-off of strength for materials that are able to produce a translucent, lifelike appearance. While clinicians strive to achieve the best balance between beauty and durability for their implant cases, events during surgery and healing often prevent those desired outcomes. From root resorption, to complications during extraction, to failed osseointegration, or even to simply placing the implant at an undesired depth, implantology is fraught with issues that can diminish the esthetic success of a case.
The case study that follows will demonstrate a unique implant solution that combines strength and esthetics for situations that require clinical flexibility in the anterior.
Case Presentation
A female patient was referred to our office by her brother-in-law, a dentist who practiced in another state. He had diagnosed her with non-restorable root resorption on tooth #9. The tooth had been part of a traumatic injury suffered in childhood that was treated at the time with endodontic therapy.
With the patient in our office, a clinical intraoral exam, as well as radiographic examination, confirmed the previous diagnosis of non-restorable root resorption (Fig. 1). The patient also exhibited a thin-tissue biotype in the esthetic zone. Due to the perceived complexity of the case, the patient was referred from our practice to a local oral surgeon for extraction and placement of the implant, as well as immediate temporization.
Prior to surgery, a CBCT scan was taken to assess the bone for viability of immediate implant placement and to evaluate the extent of resorption. During extraction, the tooth broke into several pieces, which necessitated a flap to facilitate its total removal. A BIOMET 3i™ Certain® tapered implant (BIOMET 3i, LLC; Palm Beach Gardens, Fla.) was delivered, and a particulate bone-grafting material was then placed on the palatal coronal third of the implant. After completing an evaluation for implant dehiscence, the flap was sutured closed. A torque measurement of 35 Ncm verified that the implant had achieved primary stability at the time of placement and was capable of immediate loading. A BioTemps® crown (Glidewell Laboratories; Newport Beach, Calif.) and a polyether ether ketone (PEEK) abutment were immediately seated (Fig. 2).
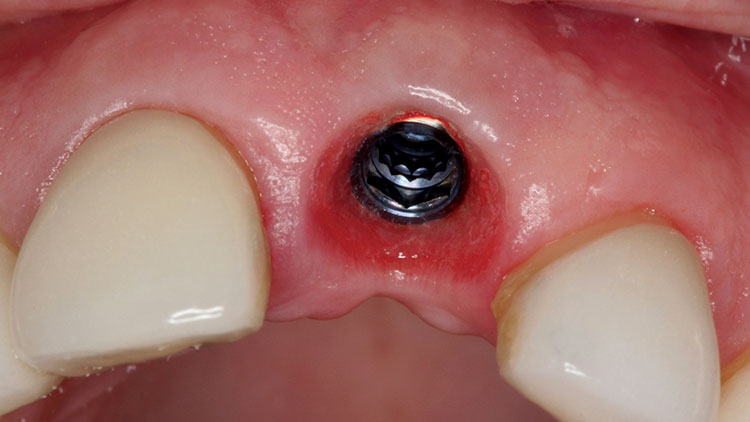
The healing period for this case was longer than usual (approximately six months), as we wanted to assess the full maturation of the tissue because of the patient’s thinner biotype (Fig. 3). Even with the best intentions and techniques, it is often difficult to place the implant as desired. When the patient returned to our practice for the restorative appointments, it was observed that a bit more recession had occurred than expected (Fig. 4). It was likely that the implant was placed at the appropriate depth, but that trauma from the initial extraction combined with the required flap caused more vertical bone loss than projected (Fig. 5).
Even with the best intentions and techniques, it is often difficult to place the implant as desired.
Due to limited availability of space, an all-zirconia abutment was not feasible without having the white margin show, which would not satisfy the esthetic requirements of either our practice or the patient. Rather, a treatment plan was devised that utilized a titanium abutment because the margin can be milled lower than the all-zirconia equivalent.
An impression of the implant was taken utilizing an attached impression coping and standard vinyl polysiloxane impression technique. This was sent to the lab for fabrication of an Inclusive® Custom Titanium Abutment (Glidewell Laboratories) and an IPS e.max® crown (Ivoclar Vivadent; Amherst, N.Y.). Titanium abutments, however, require a certain marginal thickness in order to be durable enough to cope with the stresses of osseointegration and lasting use. Unfortunately for this case, the margin of the titanium abutment had to be placed very near the tissue line, allowing a grayness to show through the thinner biotype. The margin could not be placed any more apically than pictured, resulting in partial visibility (Fig. 6).
With the desired esthetic result not achieved, we decided to turn to a BruxZir® Solid Zirconia screw-retained crown (Glidewell Laboratories). These restorations provide a one-piece alternative to cemented implant restorations by combining the abutment and crown into a single solid prosthesis (Figs. 7a, 7b). One of the biggest benefits of using a monolithic restoration like this is the elimination of the crown margin, because the titanium segment rests at the deepest possible point: on the head of the implant.
Utilizing the BruxZir screw-retained restoration resolved the issue of the visible titanium abutment margin … and gave the tissue some needed vitality.
A new impression was taken and sent to the laboratory for the fabrication of the screw-retained crown. With the patient back in the office, the crown was torqued into place, and the screw hole was sealed with composite (Fig. 8). Utilizing the BruxZir screw-retained restoration resolved the issue of the visible titanium abutment margin previously exhibited by the IPS e.max crown, and gave the tissue some needed vitality. The esthetics were much more pleasing than the initial definitive prosthesis, letting our practice deliver a final solution that met our patient’s requirements (Fig. 9).
Conclusion
While implantology has greatly advanced in recent years thanks to technological leaps in imaging and component creation, it is still quite possible for a case to heal in an undesirable way. In situations similar to this, it is paramount that the clinician is aware of and utilizes the best materials possible to provide the results required by the patient, especially in cases where the restoration is in the esthetic zone. To that end, BruxZir Solid Zirconia screw-retained crowns can help to maximize the durability and esthetics of cases that are anything but optimal.
Dr. Tarun Agarwal maintains a full-time private practice emphasizing esthetic, restorative and implant dentistry in Raleigh, North Carolina. Contact him via email at dra@raleighdentalarts.com or visit raleighdentalarts.com.