6 Years of Success: The Glidewell HT™ Implant System Shows Outstanding Long-Term Clinical Performance
Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
The Hahn™ Tapered Implant System was launched by Glidewell in 2015 and, with thousands of clinicians adopting the system, has since become one of the fastest growing implant systems in the United States. Between 2015 and 2018, an initial study of 259 implants was conducted to evaluate the clinical success of the system, resulting in overwhelming evidence that its unique design features were beneficial to patients, showing reliable outcomes, high clinical success rates and minimal marginal bone loss.
These positive results have been reinforced with the conclusion of a six-year study on the Hahn system completed in 2021.
SIX-YEAR STUDY RESULTS: A SUMMARY
In this new study, the Hahn Tapered Implant System achieved a clinical success rate of 96.2% and maintained crestal bone levels with 0.6 mm mean bone loss. These numbers compare favorably with the results of a systematic review of studies of other implant systems done over similar time periods, which have shown survival rates ranging from 93% to 95.6%.1
In addition, it is important to note that the six-year Hahn study focused on implant success, which is a more clinically relevant metric than implant survival, since it measures not only asymptomatic implants in situ at the end of the study, but also requires final restorations to be in place with no signs of excessive bone loss or loss of bone density in the surrounding area.
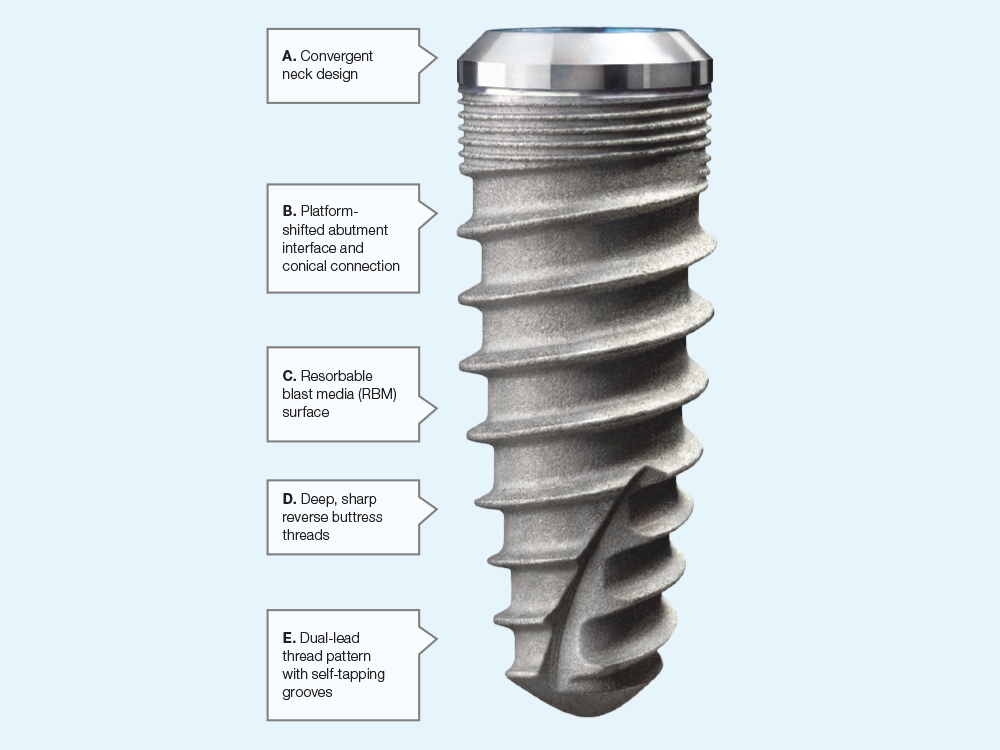
FEATURES OF THE HAHN TAPERED IMPLANT
A. Convergent Neck Design
The convergent, or tapered, shape of the neck on Hahn Tapered Implants, in contrast to other neck shapes such as concave, parallel or divergent, is crucial to the health of the bone surrounding the implant:
Reduces marginal bone stress2
- Minimizes compression forces on cortical bone
- Limits the odds of bone dehiscence (separation and failure to heal) in thin buccal plates
- Ideal for clinical situations where thickness of buccal plate may be limited
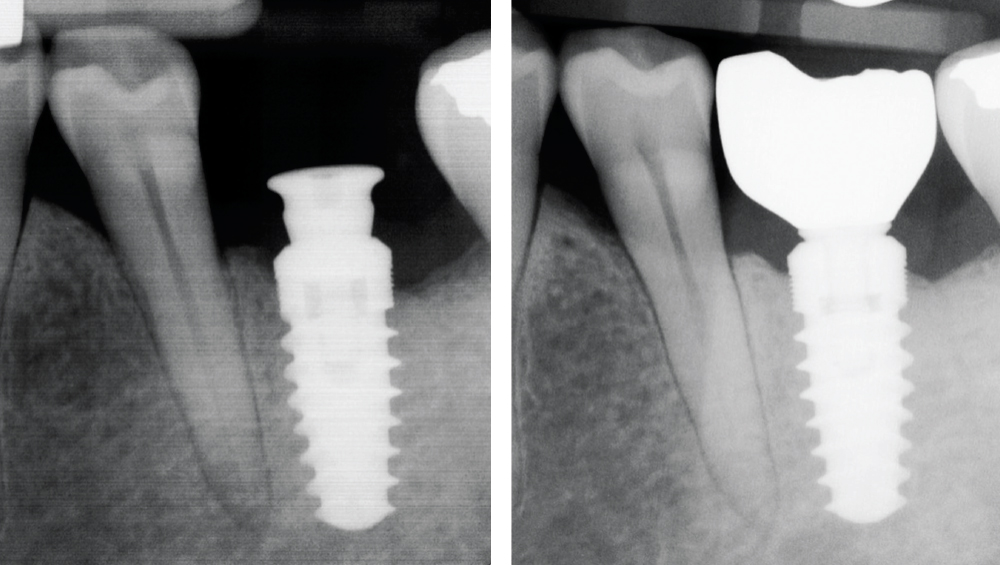
Post-op (left) and follow-up radiographs of a patient in the study illustrate the stability of interproximal bone levels around the Hahn Tapered Implant.
B. Platform-Shifted Abutment Interface and Conical Connection
Hahn Tapered Implants feature a platform-shifted abutment interface, where the diameter of the implant differs from the diameter of the abutment. This has many beneficial results, including:
Enhanced seal and stability; improved bone and tissue preservation2
- Distances the implant-abutment interface from the surrounding bone, minimizing potential contamination
- Allows for more stable peri-implant tissues by creating extra room and circumferential support
- Improves preservation of surrounding crestal bone by allowing it to maintain a coronal position
C. Resorbable Blast Media (RBM) Surface
Hahn implants are given a resorbable blast media (RBM) treatment that results in a textured surface that is ultra-clean. This has been shown to correlate with increased clinical success in a variety of ways:
Promotes osseointegration for increased survival rates and improved bone maintenance
- Improved bone-to-implant contact leads to better survival in compromised situations like post-extraction sockets
- Stronger mechanical bond during initial healing
- Increased marginal bone maintenance
- Minimized growth of epithelial cells allows better adherence of tissue fibers to implant collar
D. Deep, Sharp Reverse Buttress Threads
Implants are subjected to three types of forces during occlusal loading: compressive (inward pressure), tensile (lengthwise pulling force) and shear (two forces pushing in opposite directions). For maximum bone strength and favorable adaption, an ideal implant design should minimize shear force while doing its best to balance compressive and tensile forces.3
The Hahn Tapered Implant achieves this with reverse buttress threads; the depth and sharpness of these threads combines with their shape to provide the following benefits:
High primary stability and directional control, with reduced biomechanical stress4
- Reverse buttress thread layout transmits and balances force on the implant
- Establishes initial stability, ideal for immediate load scenarios
- Deep threads screw more securely into bone, increasing stability even in poor bone situations by increasing surface area of the implant5
E. Dual-Lead Thread Pattern with Self-Tapping Grooves
Implant stability, a key factor in osseointegration, is greatly increased by extended thread lengths. To achieve this without increasing the length of the implant itself, Hahn Tapered Implants use a dual-lead thread pattern. When combined with self-tapping grooves, this contributes to implant success on several levels:
Increases insertion speed while promoting implant stability
- Eliminates the need to drill or tap a pilot hole into bone prior to insertion
- Self-tapping insertion has been shown to result in far greater stability compared to drilling
- Dual-lead threads double the depth of insertion with each screw turn, resulting in swift, efficient insertion
- Faster insertion may promote better healing and minimized risk of contamination
CONCLUSION
Since its introduction in 2015, the Hahn Tapered Implant System has been adopted by thousands of doctors worldwide. Its efficient, economical and effective performance was first established by the successful two-year study that concluded in 2018. Now, with the conclusion of this six-year study, the excellence of the Hahn system has been validated even further.
The high clinical success rates of the Hahn system, combined with its proven record of minimized marginal bone loss, along with the other benefits it provides, should make it of interest to any doctor who places implants.
To learn how Hahn implants can help you build your practice, click here to read our blog post.
References
- ^Pjetursson BE, et al. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res. 2012;23 Suppl 6:22-38.
- ^Gracis S, Llobell A, Bichacho N, Jahangiri L, Ferencz JL. The influence of implant neck features and abutment diameter on hard and soft tissues around single implants placed in healed ridges: clinical criteria for selection. Int J Periodontics Restorative Dent. 2020 Jan/Feb;40(1):39-48.
- ^Abuhussein H, Pagni G, Rebaudi A, Wang HL. The effect of thread pattern upon implant osseointegration. Clin Oral Implants Res. 2010 Feb;21(2):129-36.
- ^Resnik RR. Principles of Implant Occlusion: Part 1 — implants are not teeth [Internet]. Glidewell; 2016 Nov 1 [cited 2022 Jun 21]. Available from: https://glidewelldental.com/education/inclusive-dental-implant-magazine/volume-7-issue-3/implant-occlsuion1
- ^Manikyamba YJB, et al. Implant thread designs: An overview [Internet]. Trends In Prosthodontics; 2018 June 23 [cited Jun 22]. Available from: https://www.researchgate.net/publication/323612840_Implant_thread_designs_An_overview