Medical Evaluation: Part 4 — The Influence of Osteoporosis and Immunosuppressive Medications (1 CEU)

It’s crucial for clinicians to understand the influence of medications on dental implants, as some patients may be taking prescription medications that have been associated with an increased dental implant morbidity. Medications for the treatment of osteoporosis and autoimmune diseases are commonly prescribed today, especially in older patients. These medications have been directly associated with an increase in infection rates, such as medication-related osteonecrosis of the jaw (MRONJ).
In Part 4, the final article of this series on the medical evaluation of dental implant patients, a reference guide will be provided with common osteoporosis and immunosuppressive medications, with respect to their contribution to infection and increased dental implant morbidity. In addition, recommendations for the modification or discontinuation of medications will be discussed in detail. This straightforward guide is designed to assist clinicians in maximizing treatment success.
For the previous articles in this series, read Part 1 (Chairside® magazine Vol. 16, Iss. 1), which covers the preoperative evaluation of the dental implant patient; Part 2 (Vol. 16, Iss. 2), which describes systemic disease and oral implants; and Part 3 (Vol. 16, Iss. 3), which discusses the influence of systemic medications on dental implant treatment.
REFERENCE GUIDE
Antiresorptive Bone Medications
1. Bisphosphonates (BP)
Oral Bisphosphonate: Alendronate (Fosamax®), risedronate (Actonel ®) and ibandronate (Boniva®)
IV Bisphosphonate: Zoledronic acid (Zometa®, Reclast®) and pamidronate (Aredia®)
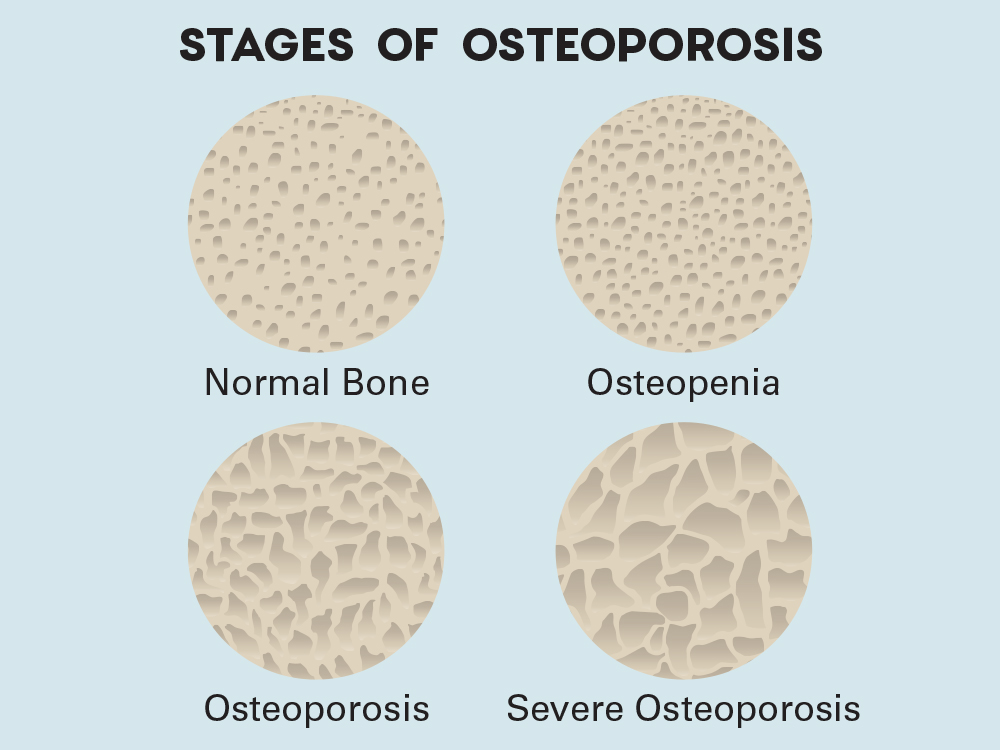
Bisphosphonates are a group of drugs that are widely used for various bone disorders, such as osteoporosis, metastatic bone cancer, and Paget’s disease. Bisphosphonates induce osteoclastic death or apoptosis at the cellular level and kill functionally resorbing osteoclasts not only at the peripheral sites, but also in the bone marrow. Unfortunately, bisphosphonates have been associated with osteonecrosis of the bone, termed medication-related osteonecrosis of the jaw (MRONJ).
Dental Implant Treatment Considerations
When considering dental implants in patients undergoing bisphosphonate therapy, the implant clinician must be conscious of the possibility of infection and/or loss of implants. According to the American Association of Oral and Maxillofacial Surgeons (AAOMS) recommendation,1 patients taking oral BP for less than four years with no comorbidities do not require any modification to the planned implant surgery. For patients with comorbidities or who have taken oral bisphosphonates for more than four years, discontinuation of the bisphosphonate (drug holiday) and/or a CTx blood test should be considered prior to surgery. However, for patients under IV bisphosphonate therapy, elective treatment is contraindicated. See Tables 1 and 2.
Table 1: Bisphosphonate Treatment Options*
Oral Bisphosphonate — Relative Contraindication
Alendronate (Fosamax), risedronate (Actonel) and ibandronate (Boniva)
Oral Use < 4 Years + No Comorbidities
- Proceed with surgery, with detailed oral and written informed consent for bisphosphonate-associated osteonecrosis and possible decreased implant healing
- Strict adherence to antibiotic prophylaxis and antimicrobial use (0.12% chlorhexidine)
- Elective: Medical clearance, CTx test or drug holiday
Oral Use > 4 Years or < 4 Years with Comorbidities
- Medical clearance
- CTx test (> 150 pg/mL) and/or drug holiday (~2-month drug-free period)
- Proceed with surgery, with detailed oral and written informed consent for bisphosphonate-associated osteonecrosis and possible decreased implant healing
- Decrease comorbidities: Periodontal disease, infections and smoking
- Strict adherence to antibiotic prophylaxis and antimicrobial use (0.12% chlorhexidine)
IV Bisphosphonate — Absolute Contraindication
Zoledronic acid (Zometa, Reclast) and pamidronate (Aredia)
*Early learning curve: Referral
Table 2: Elective Adjunct Treatments
- Drug holiday (medication discontinuation, by physician only)
- CTx blood test (risk assessment)
CTx Value (pg/mL)
300–600 (normal)
150–299
101–149
< 100
Risk for Osteonecrosis
None
None to minimal
Moderate
High

Dentists may need to obtain medical clearance for patients who take certain osteoporosis and autoimmune medications. To get started, clinicians can download Dr. Randolph Resnik’s free medical consultation/clearance form at glidewell.com/download-form.
2. Monoclonal Antibodies
Denosumab (Prolia®, Xgeva®)
These medications are human monoclonal antibodies that function as RANK (receptor activator of nuclear kappa B) ligand inhibitor, which results in decreased osteoclast function and slows the progression of bone disease. Denosumab recognizes the specific protein that normally activates osteoclasts, inhibiting their activation and preventing them from resorbing bone.
Prolia is a semiannual subcutaneous injection for the treatment of osteoporosis. It has a short half-life (26 days) and does not accumulate in the bone like bisphosphonates. Xgeva, which is prescribed at a much higher dose than Prolia, has been used to treatmetastatic bone disease.
Dental Implant Treatment Considerations
There is some debate on how implant dentists should treat patients on denosumab. Although not as common as bisphosphonates, denosumab has been linked to MRONJ. There are several oral triggers to developing MRONJ, such as invasive surgical procedures (e.g., extractions, implant placement, bone grafting).
Studies have shown that the treatment interruption of denosumab leads to the reversal of its bone-mineral-density effect, resulting in pre-therapy levels within one year of discontinuation. In addition, it has been reported that these patients are at an increased risk of fragility fractures, and drug cessation has been associated with a high risk of rebound vertebral fractures.Therefore, many physicians are reluctant to approve a discontinuation of Prolia because of increased susceptibility to bone fractures.2 Recently, a new protocol has been reported that minimizes the possibility of bone fragility (Table 3).3
Patients on Xgeva (higher doses of denosumab) are usually on a monthly regimen for metastatic bone disease. Because of the potential for MRONJ, any type of elective dental treatment is absolutely contraindicated.
Table 3: Denosumab Treatment Option
Delayed Dosing Protocol — Relative Contraindication
- Surgery Date: Determine the fifth month after the last administration of Prolia. Schedule the procedure within a 15-day window after the fifth month.
- Medical Clearance: Consult directly with the patient’s physician concerning the delayed dosing window. The physician should contact the patient to modify the administration date.
- Prophylactic Antibiotics: Ensure the patient is treated with pre- and post-op prophylactic antibiotics (beta-lactam).
- Surgical Procedure: Minimize the invasiveness of the proposed surgery and reduce surgical duration.
Patients who take medication to treat osteoporosis may require an implant treatment protocol that minimizes the possibility of bone fragility.
Immunosupressive Medications
1. Biologics
Varies (Table 4)
Biologics are a newer class of therapeutic drugs that are utilized in the treatment of autoimmune diseases and cancers. Biologic medications are tumor necrosis factor (TNF) inhibiting drugs, which are involved in inhibiting chronic inflammatory conditions and the resulting immune response (Table 4).
Dental Implant Treatment Considerations
Although case reports with dental implants and biologics are minimal, caution must be exercised, as patients are susceptible to increased infectious episodes, intraoperative bleeding and compromised bone healing.
For patients who have used biologic medication in the past, medical consultation is recommended to determine the level of immune suppression and the current status of the patient’s disease process. A detailed oral and written informed consent is recommended. For patients concurrently taking biologic medications, medical consultation/clearance is highly recommended. Physicians will evaluate the specific medication in question, medication dosage, treatment duration, comorbidities, possibility of disease rebound and type of surgical procedure to be performed. In most cases, physicians will recommend the modification of the medication in the perioperative period, which most likely will include a discontinuation via a drug holiday of four to five times the half-life of the medication.4,5
For example, the most common biologics — etanercept (two weeks), adalimumab (six to eight weeks), and infliximab (four to six weeks) — would be discontinued prior to surgery. The dental clinician should recommend that the physician instruct the patient of the specific instructions of the drug holiday. In no situation should a dental clinician modify a patient’s biologic medication that is prescribed by the patient’s physician. In addition, a detailed verbal and written informed consent should be presented. Biologic medications are most commonly restarted postoperatively provided that wound healing is satisfactory with no evidence of infection or prolonged bleeding.
Dental Implant Implications
Past biologic therapy: Relative contraindication after medical consultation
Concurrent biologic therapy with implant therapy: Medical consult and relative or absolute contraindication
Table 4: Most Common Biologic Medications
- Adalimumab (Humira®): Rheumatoid arthritis, Crohn’s disease, ulcerative colitis, psoriatic arthritis, ankylosing spondylitis
- Infliximab (Remicade®): Rheumatoid arthritis, Crohn’s disease, ulcerative colitis, psoriatic arthritis, ankylosing spondylitis
- Etanercept (Enbrel®): Rheumatoid arthritis, psoriatic arthritis
- Trastuzumab (Herceptin®): Human epidermal growth factor receptor 2-positive (HER2+) breast cancer
- Ranibizumab (Lucentis®): Age-related macular degeneration
- Interferon beta-1a (Avonex®): Multiple sclerosis
- Glatiramer acetate (Copaxone®): Multiple sclerosis
- Brodalumab (Siliq®): Psoriatic arthritis
- Ixekizumab (Taltz®): Psoriatic arthritis
- Secukinumab (Cosentyx®): Psoriatic arthritis, ankylosing spondylitis
- Ustekinumab (Stelara®): Psoriatic arthritis, Crohn’s disease

For patients concurrently taking biologic medications, medical consultation/clearance is highly recommended. After careful evaluation, the patient’s physician may recommend the modification of the medication in the perioperative period.
2. Chemotherapy Agents
Methotrexate: Otrexup® (PF), Xatmep® , Trexall® and Rasuvo®
Cyclosporin: Sandimmune® , Neoral® , Gengraf® and Restasis®
Chemotherapeutic agents (cytotoxins) are common medications in the treatment of malignant disease. Unfortunately, these drugs cannot discriminate between malignant and normal tissues and become cytotoxic to normal tissue. Most chemotherapeutic agents are known to have detrimental effects on bone, especially on grafted bone in which the blood supply is compromised.
Many of these cytotoxic medications have been shown to predispose patients to infection and delayed bone healing. In addition, studies have shown that these medications may negatively influence the bone-implant interface of previously placed dental implants.6
Dental Implant Treatment Considerations
The effect of cytotoxic medications on the healing or maintenance phases of dental implants is variable and is dependent on many factors, including the patient’s immune status. Therefore, a medical consultation is highly recommended for any patient who has had or will have therapy. The physician and implant clinician should take into consideration the current immunosuppressive level, medication toxic effects and the patient’s ability to tolerate the implant surgery.
In most cases, concurrent chemotherapy is an absolute contraindication to dental implant therapy, as there is a high infection and failure rate. However, it is not uncommon for some of the cytotoxic medications to be used in lower doses for various other diseases. For example, methotrexate, originally an aggressive cancer therapy, is now a first-line treatment (in low doses) of psoriasis and rheumatoid arthritis. At the low doses, the cytotoxic medication is considered a relative contraindication.
The effect of cytotoxic medications on the healing or maintenance phases of dental implants depends on the patient’s immune status, among other factors.
3. Antihypertensive Medications
Oral Antihypertensives: Amlodipine (Norvasc®), irbesartan (Avapro®), lisinopril (Prinivil®), losartan (Cozaar®), metoprolol (Lopressor®), valsartan (Diovan®) and enalapril (Vasotec®)
Hypertension is a chronic medical condition that affects approximately half of adults in the United States, and only about 24% of patients with hypertension have the condition under control. Hypertension is most commonly treated with oral medications, such as beta-blockers, thiazide diuretics, angiotensin converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs). Interestingly, antihypertensive drugs can affect bone metabolism in different ways (Table 5).7
Table 5: Antihypertensive Medication Effects on Bone
- Beta-blockers: Inhibit activity of osteoclasts by blocking beta-2 adrenergic receptors
- Thiazide diuretics: Increase bone formation by increasing calcium absorption
- ACE inhibitors and ARBs: Increase bone formation by blocking the reninangiotensin system
Dental Implant Treatment Considerations
The use of antihypertensive medications may directly affect dental implant treatment in the following ways:
- Surgical Risk: Patients who are hypertensive pose a risk to the implant clinician with respect to perioperative cardiovascular emergency events.
- Positive Effect: Antihypertensive medications have been shown to positively affect the integration of implants with higher survival rates.8
- Negative Effect: A higher incidence of bruxism has been shown with hypertensive patients. Bruxism is a risk factor for prosthetic failure and dental implant loss.9
Care must be exercised when treating patients on antihypertensive medications, as they pose a possible surgical and prosthetic risk. In cases of suspected poor hypertension compliance, clinicians should obtain medical clearance and verify the patients have a stable cardiovascular status.

To maximize success, clinicians should understand how antihypertensive medications may affect the treatment of dental implant patients.
CONCLUSION
Patients today, even those with life-threatening diseases, are more socially active and have a better quality of life than ever before because of advancements in medical care. However, many of the newer, more common medications can be associated with devastating effects on dental implant treatment. Patients being treated with antiresorptive, chemotherapeutic and immunosuppressive medications are at the forefront of possible increased dental implant complications. Therefore, a comprehensive assessment and understanding of the patient’s medical history and current medication usage is crucial for the long-term success of dental implant treatment.
All third-party trademarks are property of their respective owners.
References
- ^Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O’Ryan F; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw — 2014 update. J Oral Maxillofac Surg. 2014 Oct;72:1938-56.
- ^Anastasilakis AD, Polyzos SA, Makras P, Aubry-Rozier B, Kaouri S, Lamy O. Clinical features of 24 patients with rebound-associated vertebral fractures after denosumab discontinuation: systematic review and additional cases. J Bone Miner Res. 2017 Jun;32(6):1291-6.
- ^Di Fede O, Panzarella V, Mauceri R, Fusco V, Bedogni A, Lo Muzio L, Sipmo Onj Board, Campisi G. The dental management of patients at risk of medication-related osteonecrosis of the jaw: new paradigm of primary prevention. BioMed Res Int. 2018 Sep 16; 2018:1-10.
- ^Smith CH, Anstey AV, Barker JN, Burden AD, Chalmers RJ, Chandler DA, Finlay AY, Griffiths CE, Jackson K, McHugh NJ, McKenna KE, Reynolds NJ, Ormerod AD; (Chair of Guideline Group). British Association of Dermatologists’ guidelines for biologic interventions for psoriasis 2009. Br J Dermatol. 2009 Nov;161(5):987-1019.
- ^Radfar L, Ahmadabadi RE, Masood F, Scofield RH. Biological therapy and dentistry: a review paper. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015 Nov; 120(5):594-601.
- ^Blanchaert RH. Implants in the medically challenged patient. Dent Clin N Am. 1998 Jan;42(1):35-45.
- ^Wu X, Al-Abedalla K, Eimar H, Arekunnath Madathil S, Abi-Nader S, Daniel NG, Nicolau B, Tamimi F. Antihypertensive medications and the survival rate of osseointegrated dental implants: a cohort study. Clin Implant Dentistry Relat Res. 2016 Dec;18(6):1171-82.
- ^Al-Subaie AE, Laurenti M, Abdallah MN, Tamimi I, Yaghoubi F, Eimar H, Makhoul N, Tamimi F. Propranolol enhances bone healing and implant osseointegration in rats tibiae. J Clin Periodontol. 2016 Dec;43(12):1160-70.
- ^Martynowicz H, Dymczyk P, Dominiak M, Kazubowska K, Skomro R, Poreba R, Gac P, Wojakowska A, Mazur G, Wieckiewicz M. Evaluation of intensity of sleep bruxism in arterial hypertension. J Clin Med. 2018 Oct 5;7(10):327.