Full-Arch Implant Treatment: A Restorative-Driven Approach (1 CEU)

Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Advancements in digital technology have made it possible to visualize the esthetic outcome before treatment begins, even for complex cases such as full-arch implant rehabilitation. Treatment planning with the goal in mind allows the clinician to understand potential limitations and provide realistic options for the patient.
To understand the benefits of this restorative-driven approach, let’s look at a case where we were able to leverage this technology to rebuild a patient’s smile.
CASE REPORT
This patient presented with stage IV periodontitis and sought a solution to his loose and missing teeth. A CBCT scan was taken and, after discussing the results with the patient, full-mouth extraction with implant placement was determined to be the desired treatment plan. Due to the severity of the periodontal disease, the patient’s teeth were no longer in the proper restorative position. Before devising the surgical plan, we needed to establish the ideal tooth position, desired vertical dimension of occlusion and jaw relationship.
After determining the ideal tooth position, we can visualize where the implants should be placed to support this tooth arrangement. This approach allows us to see how much restorative room we will need to fabricate a prosthesis with the desired esthetics. Our goal was to restore the patient with BruxZir® Esthetic Implant Prostheses. After capturing the necessary clinical information, we collaborated with the Glidewell team to create a prosthetically driven surgical plan. With the help of Glidewell’s Digital Treatment Planning (DTP) team, we created a treatment plan that ensured implant positioning for an optimal esthetic outcome. The expertise of the Full-Arch Implant department allowed for a seamless, predictable workflow once the implants were ready for restoration.

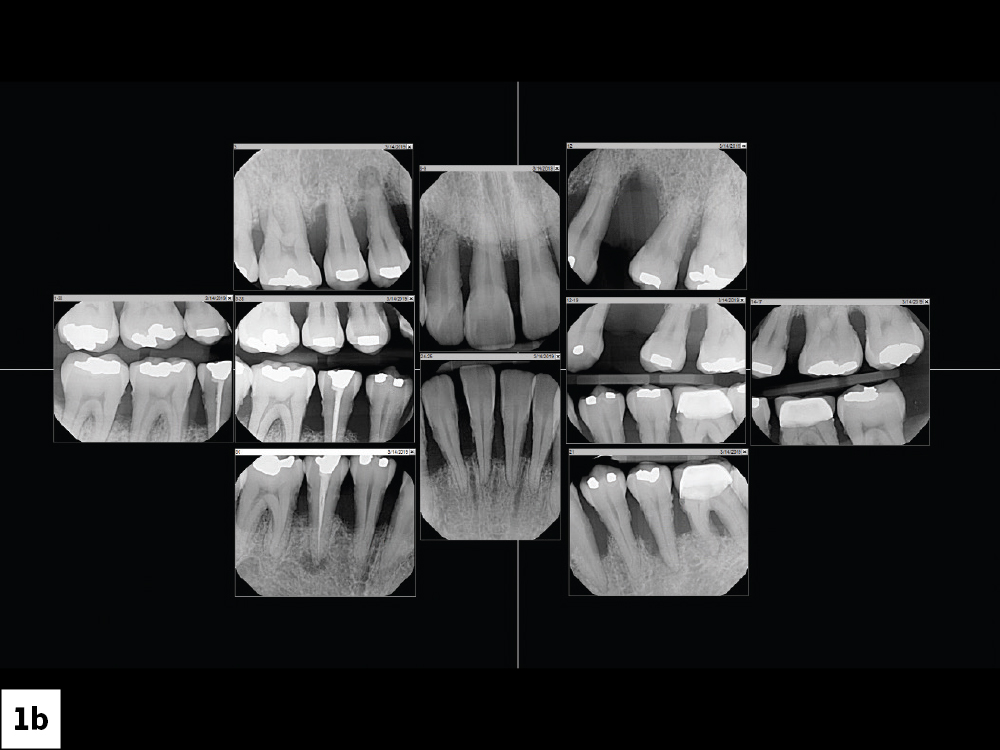
Figures 1a, 1b: The patient presented with stage IV periodontitis and grade 3 mobility. With grade 3 mobility, teeth are considered terminally mobile and are indicated for extraction.

Figure 2: To help guide the digital treatment planning process, intraoral scans were taken, which eliminated the risk that mobile teeth could be removed while taking a physical impression.
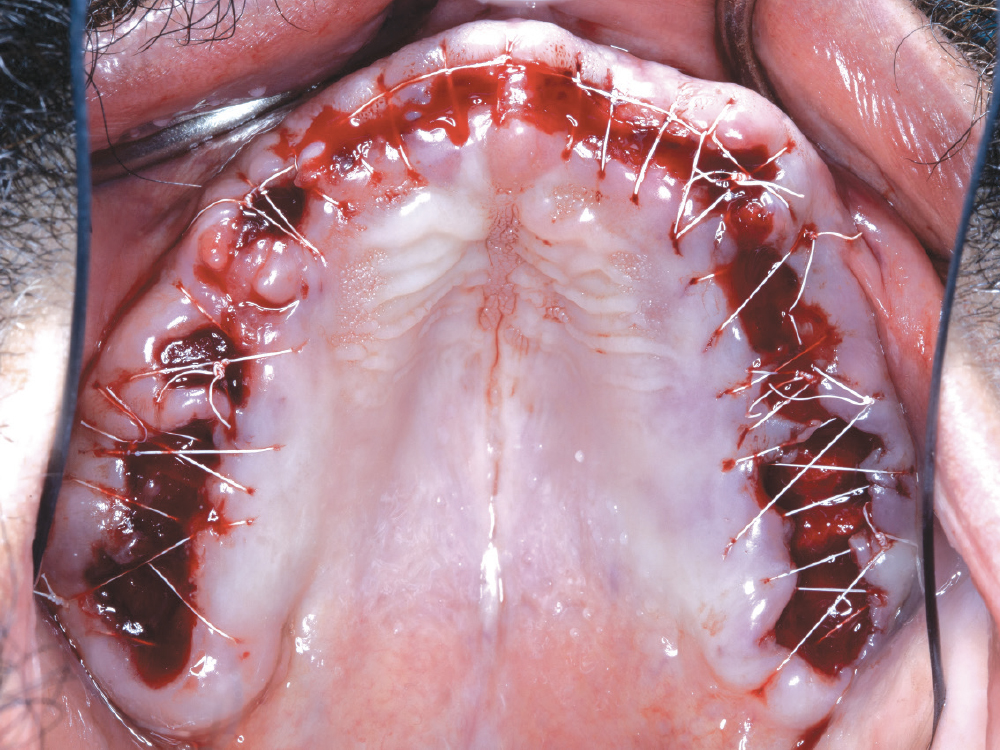
Figure 3: Rather than opting for immediate implant placement, we took a “graft and wait” approach. The bone was recontoured and, where needed, Newport Biologics™ Resorbable Collagen Plugs (Glidewell Direct; Irvine, Calif.) were placed.
With the help of Glidewell’s Digital Treatment Planning (DTP) team, we created a treatment plan that ensured implant positioning for an optimal esthetic outcome.


Figures 4a, 4b: Immediate Simply Natural™ 3D-Printed Dentures (Glidewell; Newport Beach, Calif.) were relined with tissue conditioner and delivered following the extractions. The dentures were constructed based on the patient’s initial vertical, which would need refining after the arches healed.


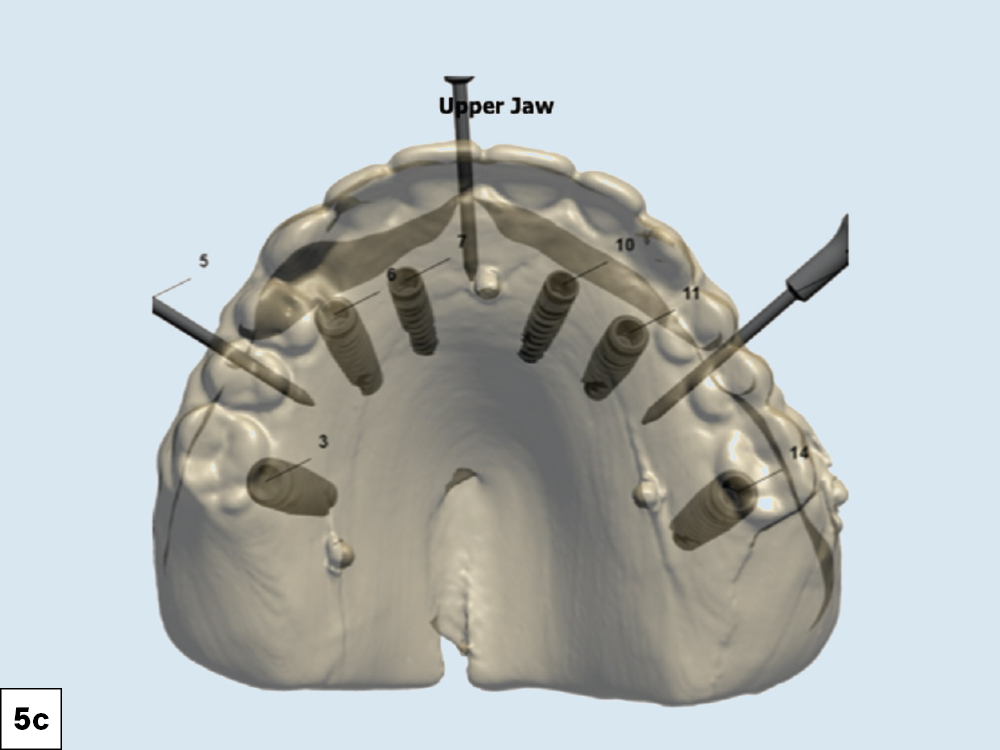
Figures 5a–5c: After four months of healing, a new set of dentures was fabricated to create the ideal tooth position and to establish the desired esthetics and vertical dimension. This tooth arrangement also helped to digitally plan the position of the implants and served as the basis for the eventual BruxZir full-arch restorations. The dual-scan CBCT protocol was followed with the new set of dentures, allowing the DTP team to visualize the ideal restorative plan. The lip position (lip line) is important information to note before placing the implants. The goal is to either blend the transition line of the final prosthesis by sculpting the tissue or hide it by ensuring it is covered by the lip. Providing the DTP team with adequate CBCT images, duplicates of the existing prosthesis and clinical photographs (true high smile line) allows the technicians to work with you to provide the best restorative outcome.

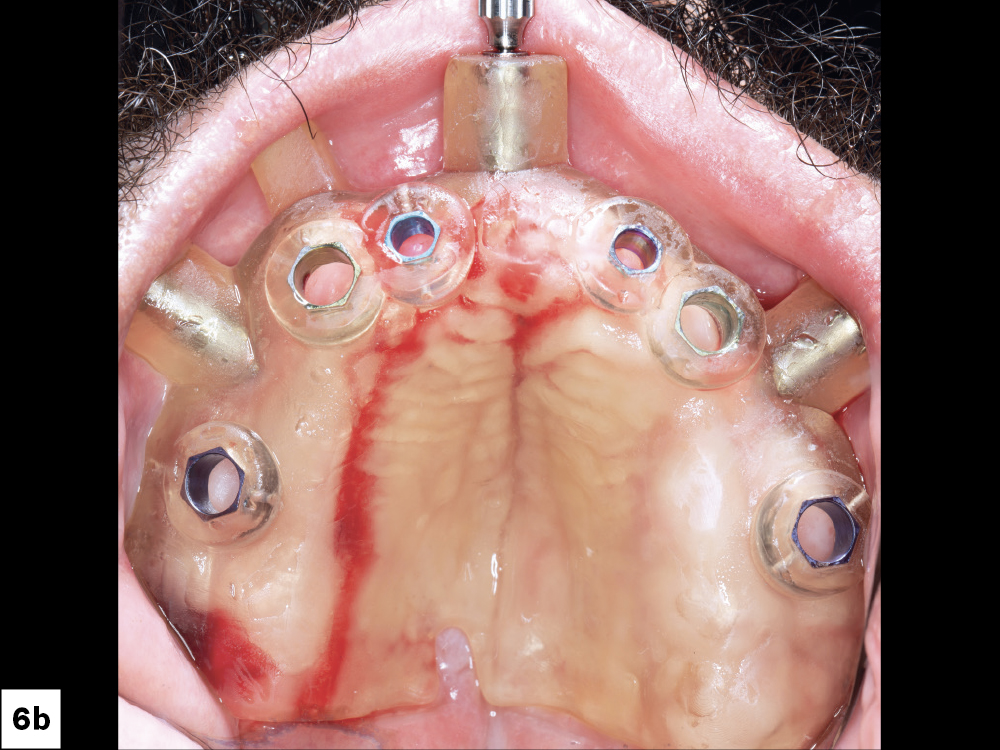
Figures 6a, 6b: On the day of implant surgery, we seated the surgical guide over the maxilla and used three anchor pins to fix the guide to the arch to keep it securely in place during the procedure.

Figure 7: The implant osteotomies were created by following the simplified surgical protocol of the Hahn™ Tapered Implant Guided Surgery System (Glidewell Direct). With the Hahn system, there are no drill keys or “spoons,” making for a less cumbersome and more efficient surgical procedure. The Hahn Tapered Implants were placed through the surgical guides, completing a fully guided implant placement procedure from start to finish.


Figures 8a, 8b: At time of placement, the implants had sufficient primary stability, allowing multi-unit abutments to be torqued into place. (The angle and height of each multi-unit abutment were previously selected as part of the digital treatment plan.) Multi-unit temporary healing caps were subsequently placed. The tissue was contoured around the multi-unit abutments while the implants integrated. The intaglio surfaces of the dentures were hollowed to allow space for the healing caps. Another option at this time would be to convert the existing denture or attach a 3D-printed prosthesis at the time of surgery.
With the Hahn system, there are no drill keys or 'spoons,' making for a less cumbersome and more efficient surgical procedure.


Figures 9a, 9b: When it came time to fabricate the definitive restorations, the implant lab at Glidewell used scans of the definitive dentures as a reference for the setup of the final BruxZir Esthetic Implant Prostheses.
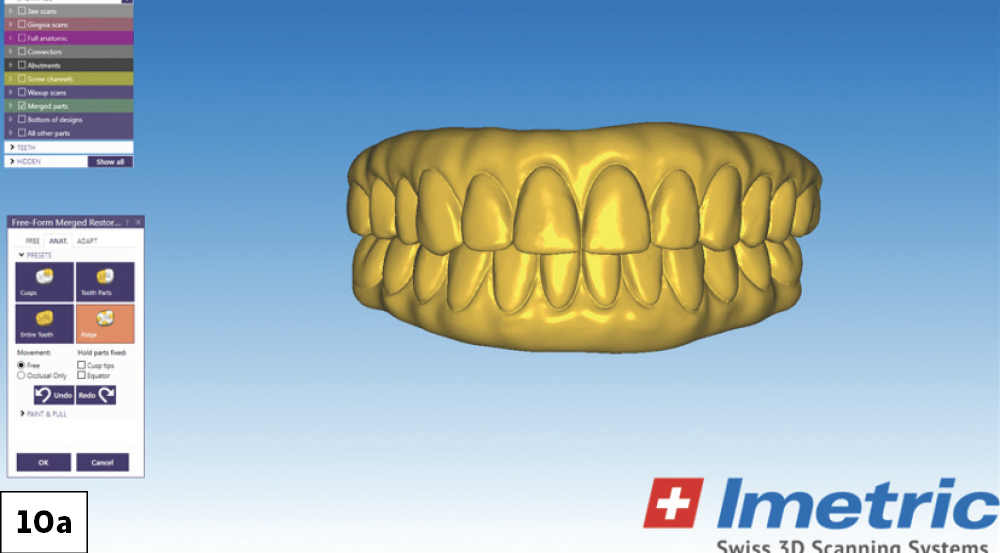
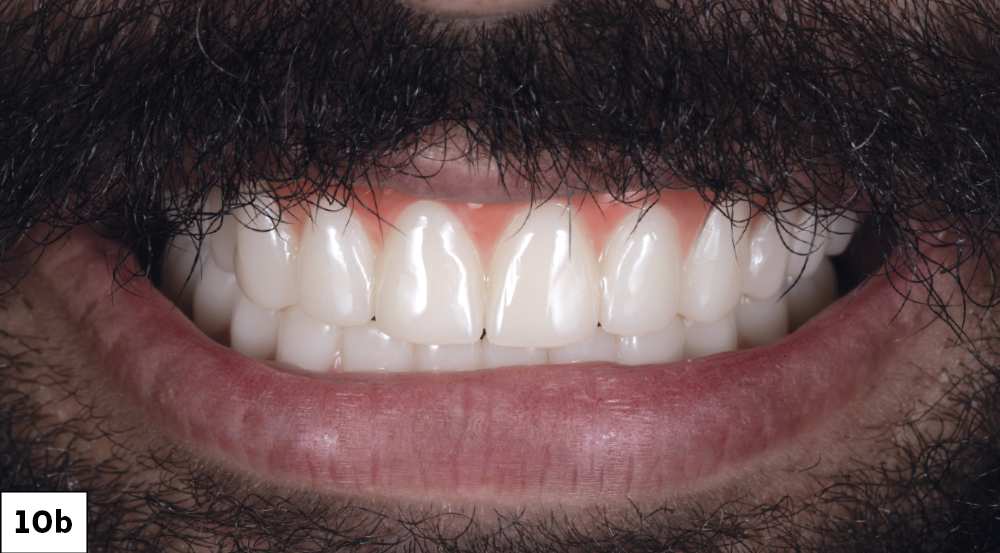
Figures 10a, 10b: Digital designs for the restorations were created in collaboration with the lab before the provisionals were fabricated. It is recommended that poly(methyl methacrylate) (PMMA) provisional implant prostheses be worn by the patient for a trial period to “test drive” the prosthetic design and confirm occlusion and esthetics.


Figures 11a, 11b: After the patient wore the PMMA provisionals for four weeks and indicated his approval of the design, definitive BruxZir Esthetic Implant Prostheses were then milled from 100% solid zirconia, bringing the visualized treatment plan to life. Collaboration between the restorative doctor, surgical doctor and laboratory technicians throughout the patient’s implant journey is key in providing predictable outcomes.
It is recommended that poly(methyl methacrylate) (PMMA) provisional implant prostheses be worn by the patient for a trial period to 'test drive' the prosthetic design and confirm occlusion and esthetics.

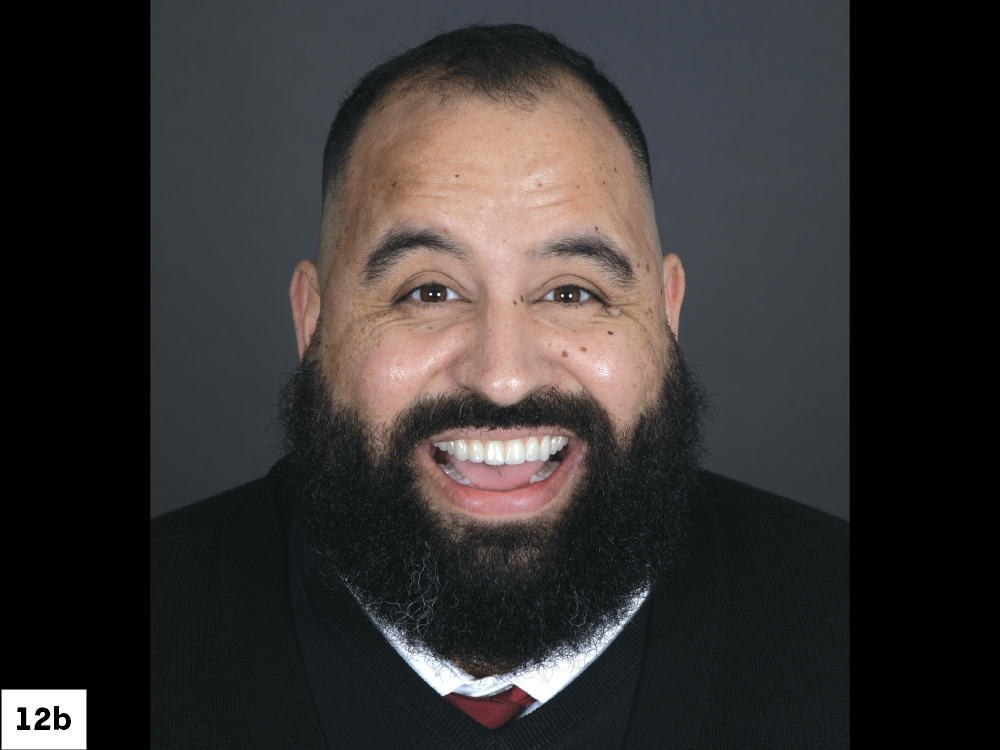
Figures 12a, 12b: The “before” image shows the initial patient condition, which presented challenges that necessitated a restorativedriven approach to implant treatment. The “after” image shows the definitive BruxZir Esthetic restorations in place, completing a full mouth rehabilitation done entirely with Glidewell Implant Solutions, from bone grafting material to digital treatment planning, surgical guides, implants and final prostheses.
CONCLUSION
In the end, full-arch implant treatment is all about reviving the patient’s smile. When I’m placing implants, whether for a single tooth or the entire arch, I always want to work toward that goal. The best way to achieve predictable results is with a team that works together and understands the importance of a prosthetically driven treatment plan.
Glidewell empowers clinicians by providing them with the resources necessary to provide predictable implant treatment, from initial planning to the delivery of the restoration. When you restore your Hahn Tapered Implant System case at Glidewell, you automatically receive 20% off the definitive restoration. Additionally, the Hahn system is supported by bundle pricing when you work with Glidewell DTP, which reduces your surgical and restorative costs by as much as 28% (list price of bundle components $552; Hahn bundle price for single site $395). This comprehensive approach, which keeps the treatment plan’s end result in mind from the very beginning of the restoration case, culminates with a seamless patient experience.