Socket Grafting and Implant Placement: A Simplified Approach (1 CEU)

Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Bone grafting procedures are becoming commonplace in the general practice, whether for simple procedures like socket grafting or more complex ones like prosthetic reconstruction and implant placement. Fortunately, dentists today have access to bone grafting solutions that make socket grafting, ridge augmentation and peri-implant management simple and repeatable.
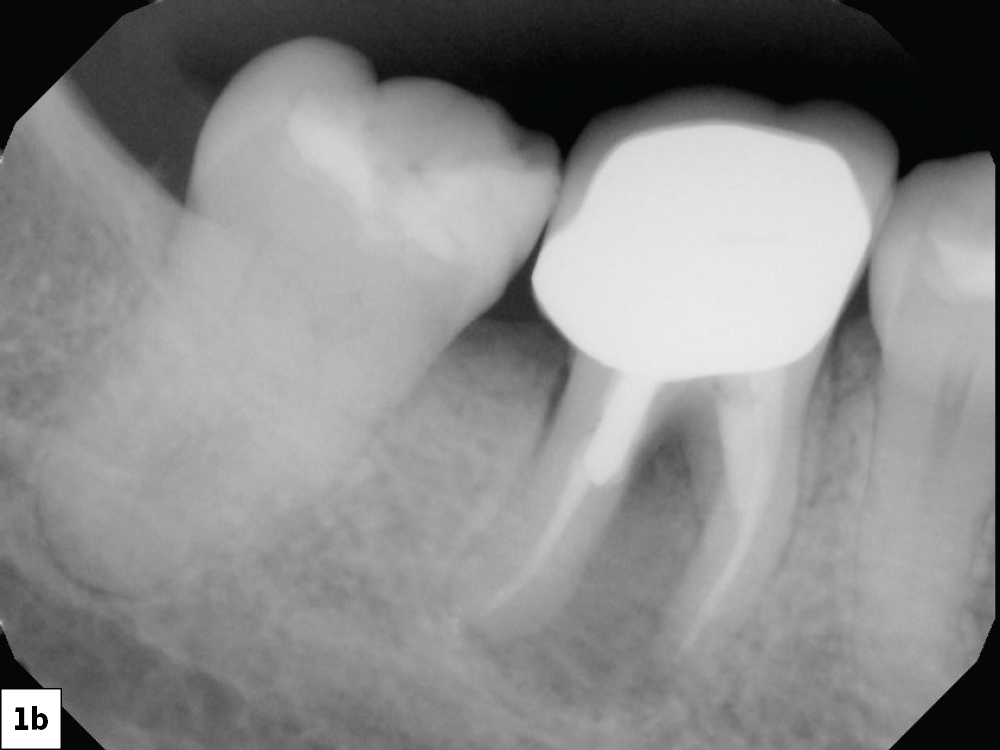
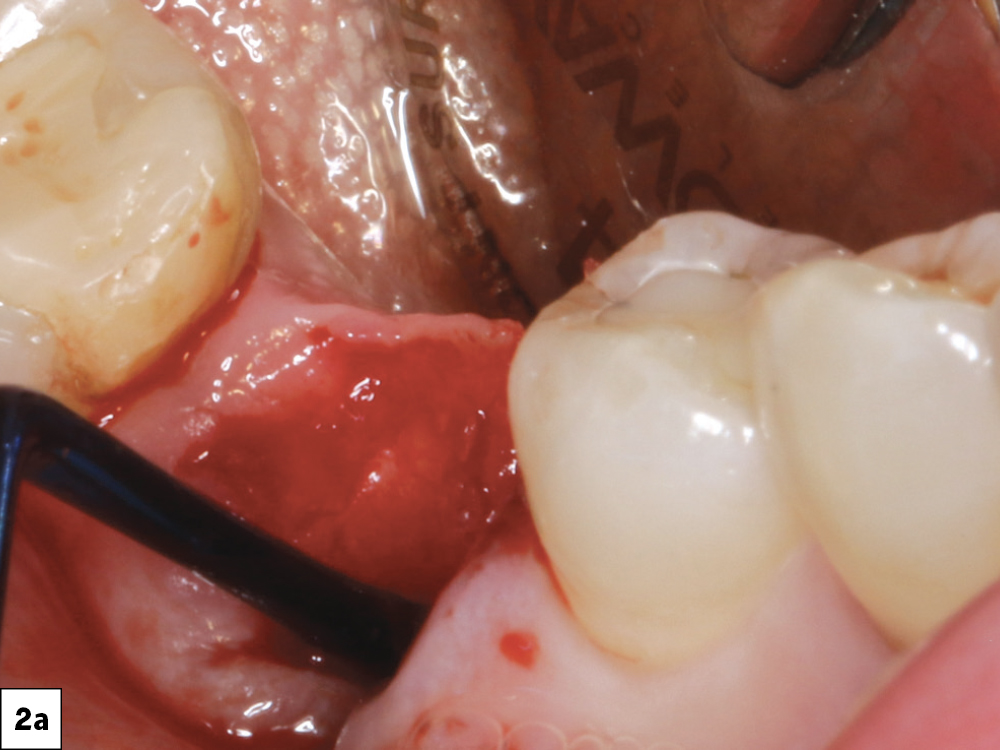
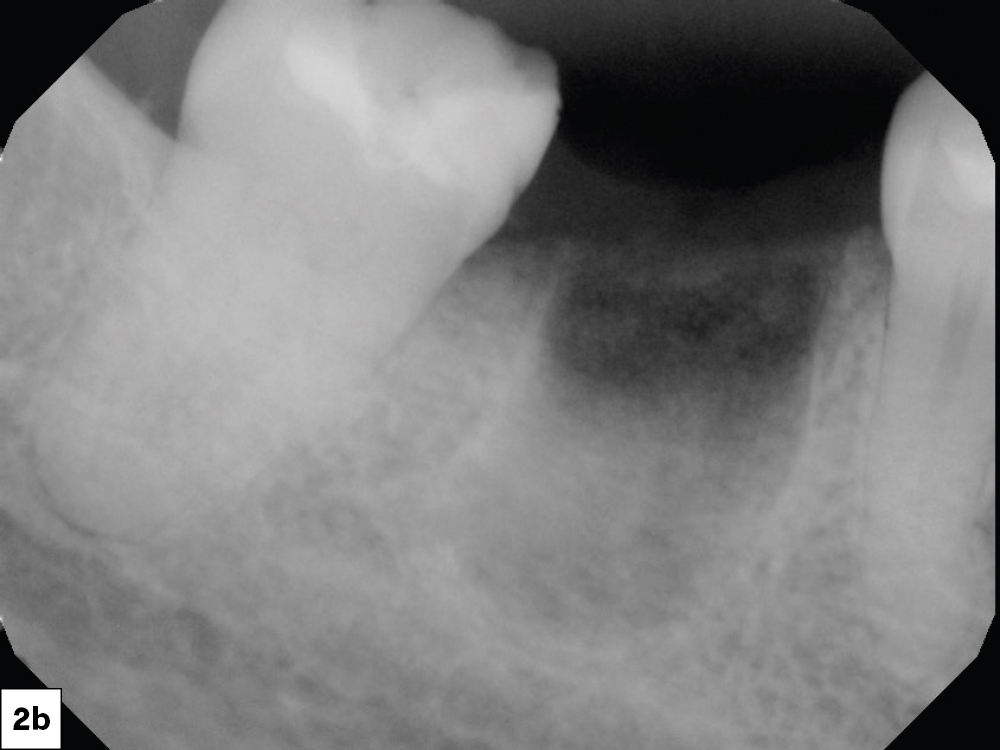
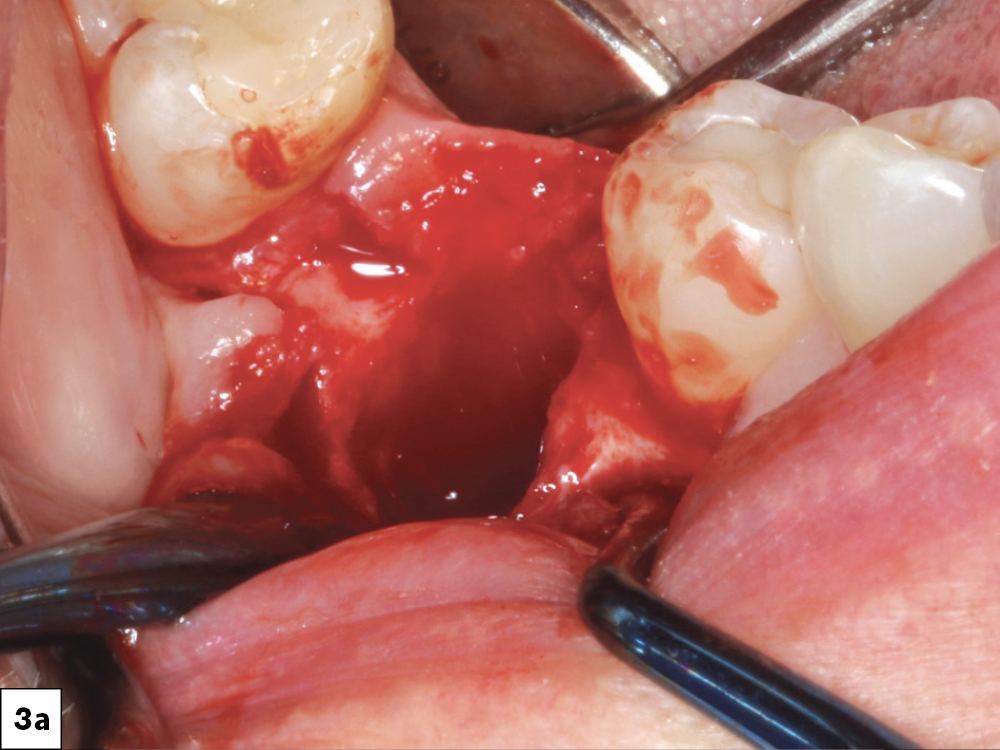
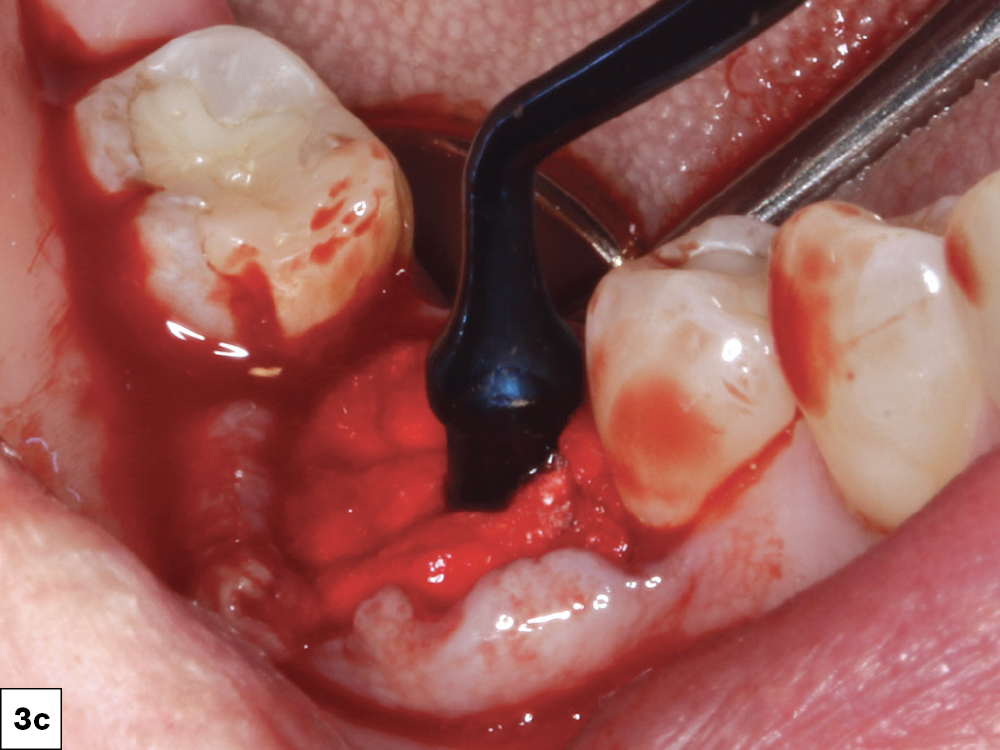
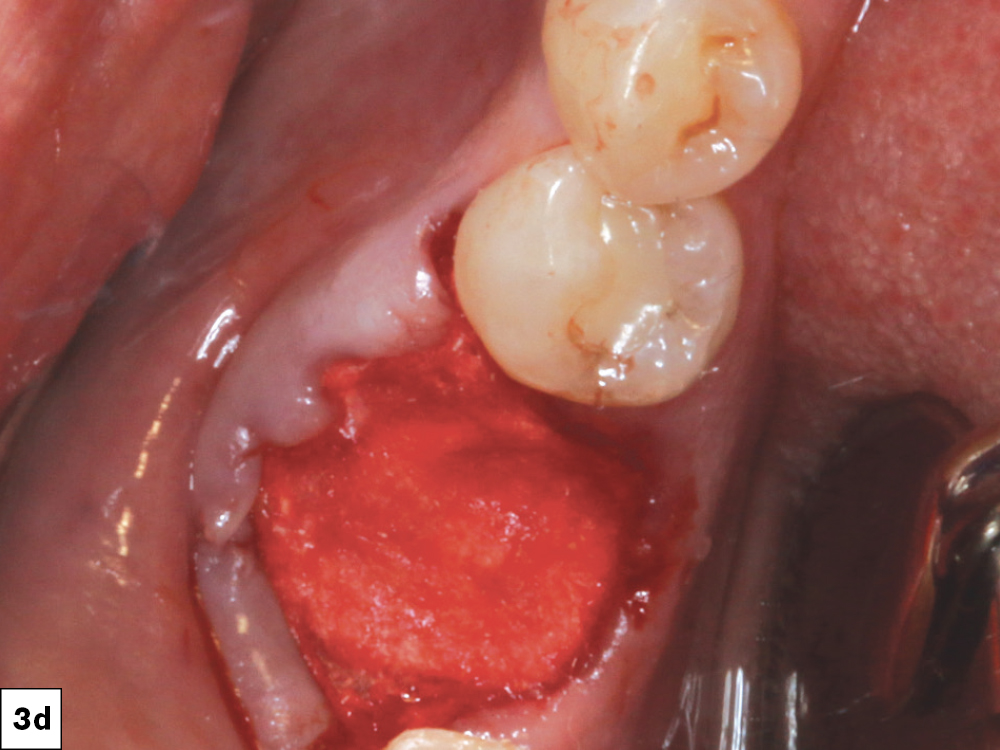
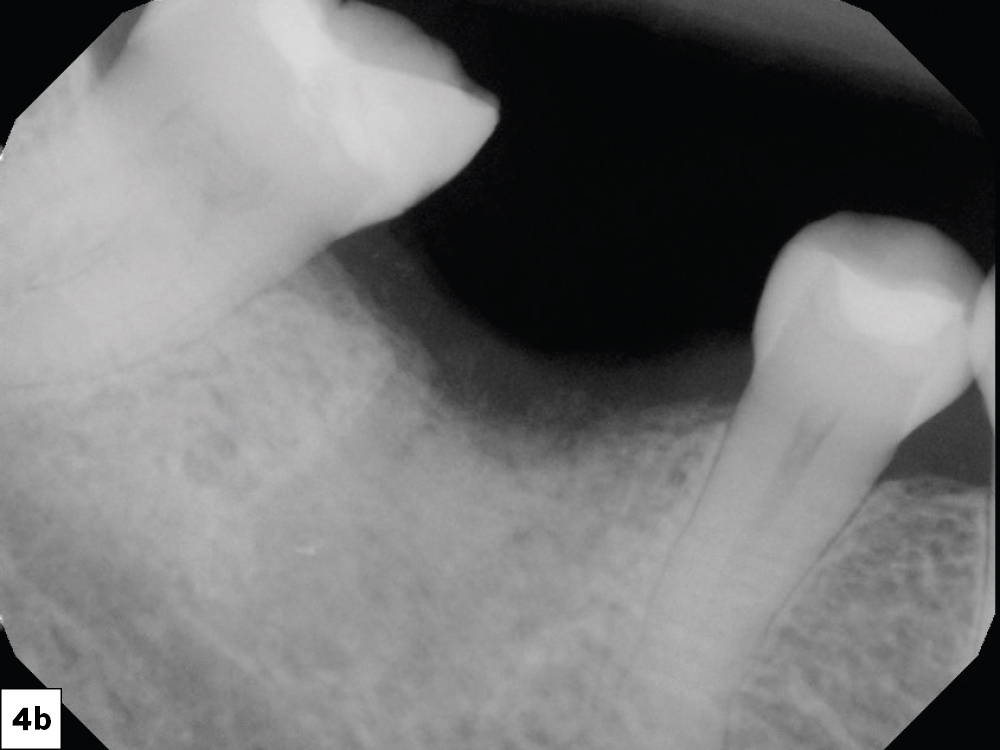
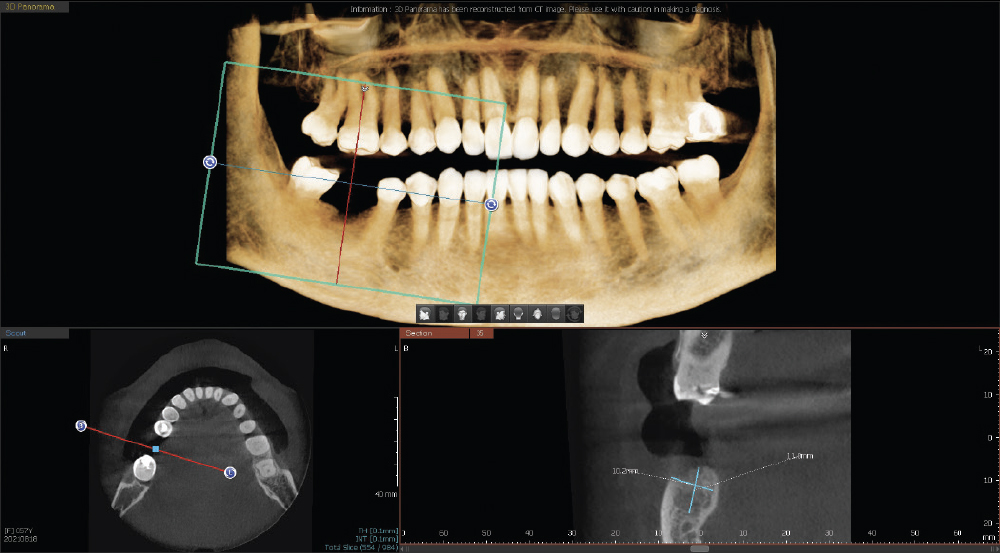
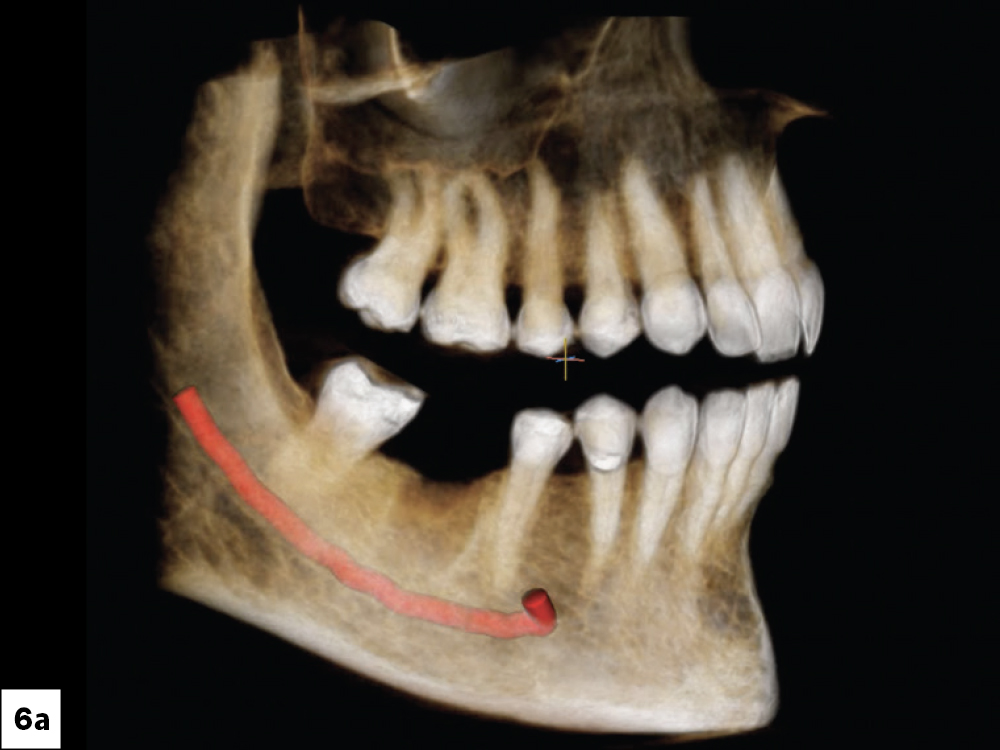
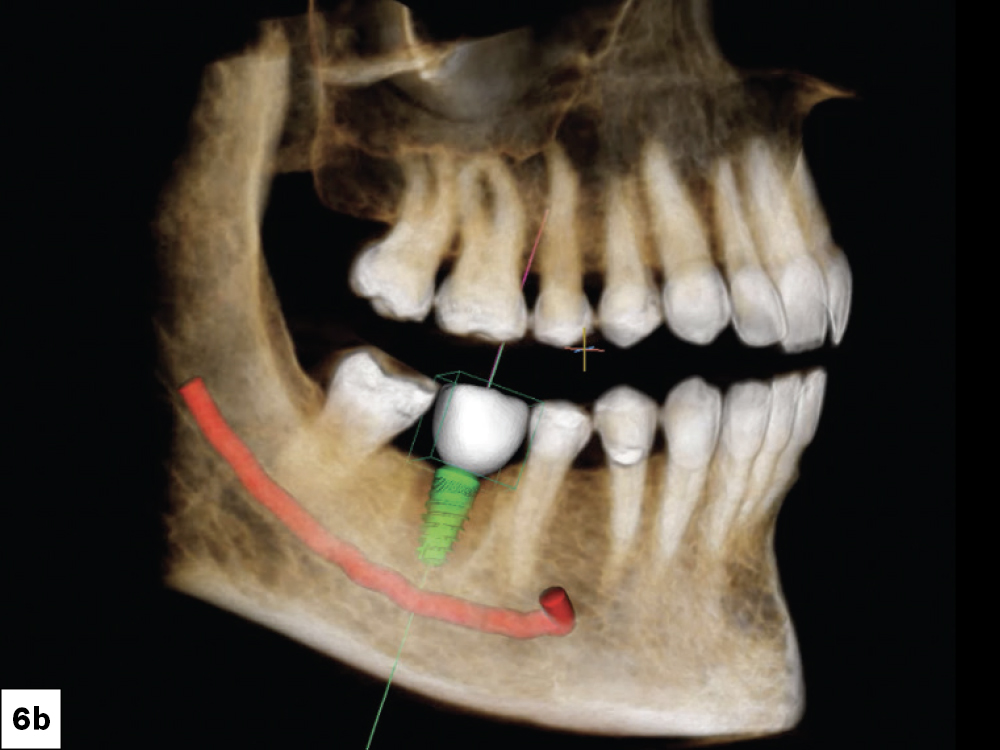
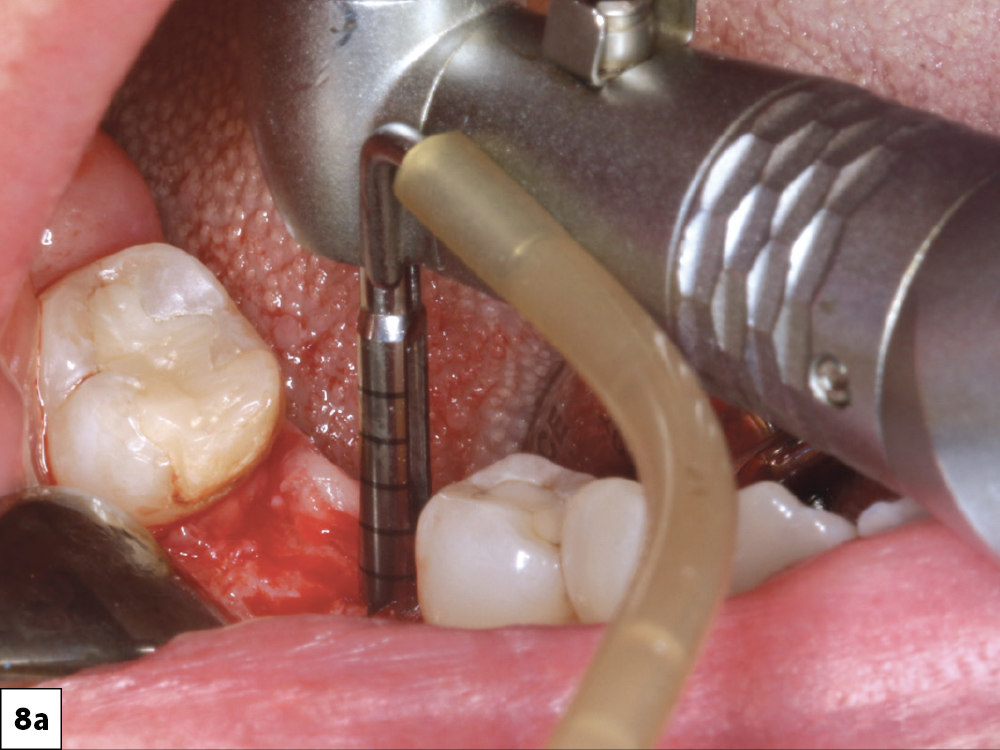
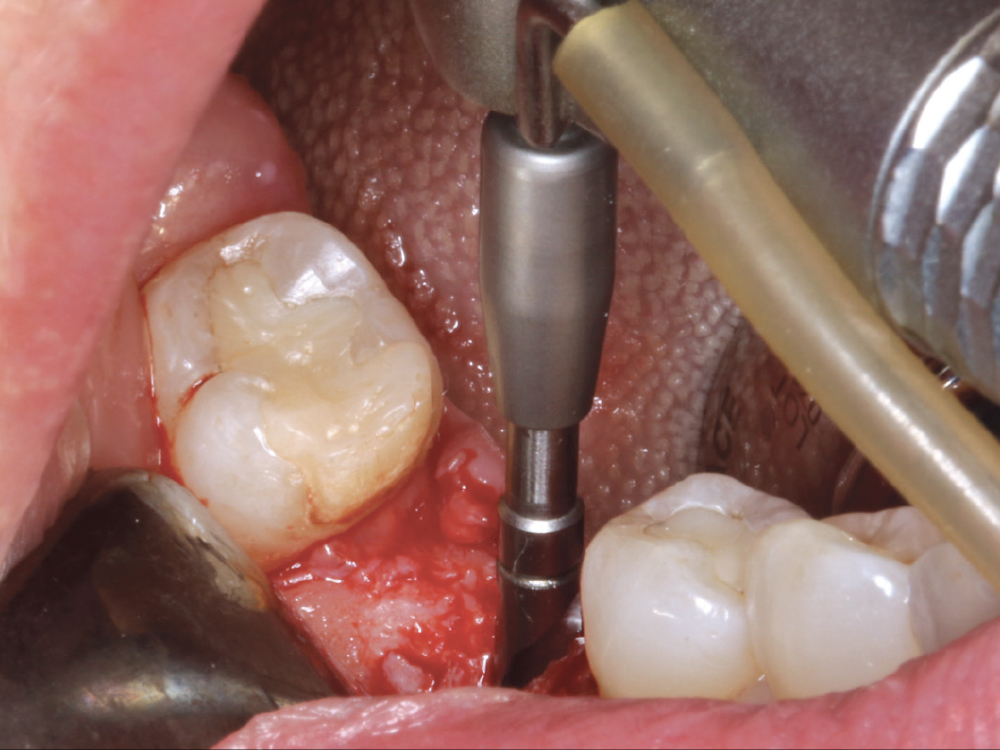
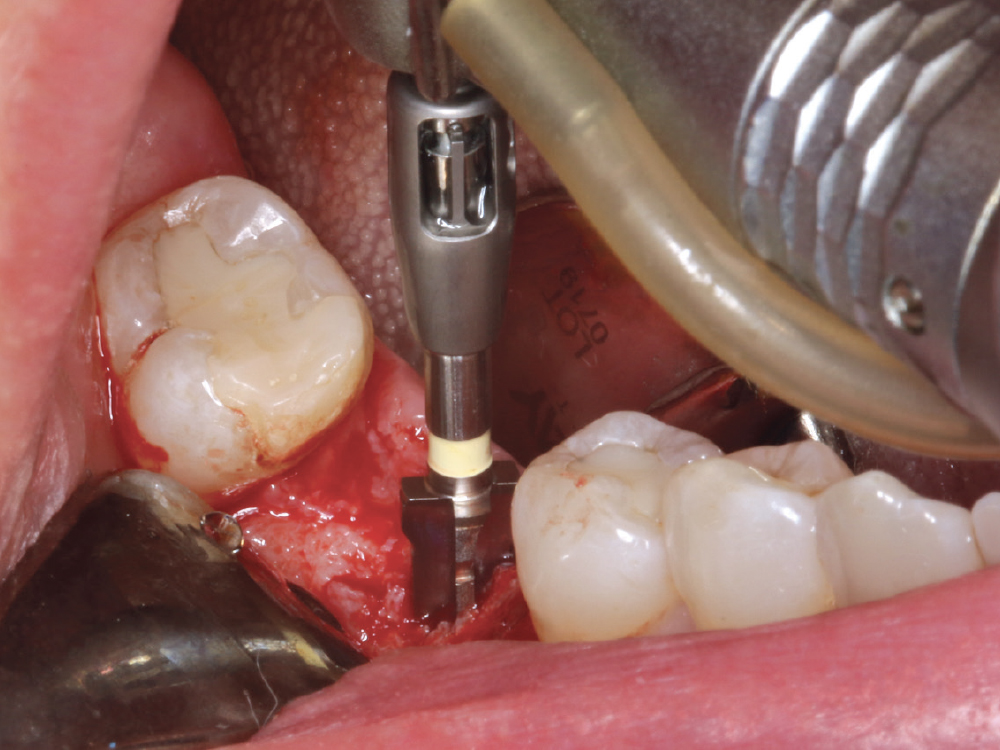
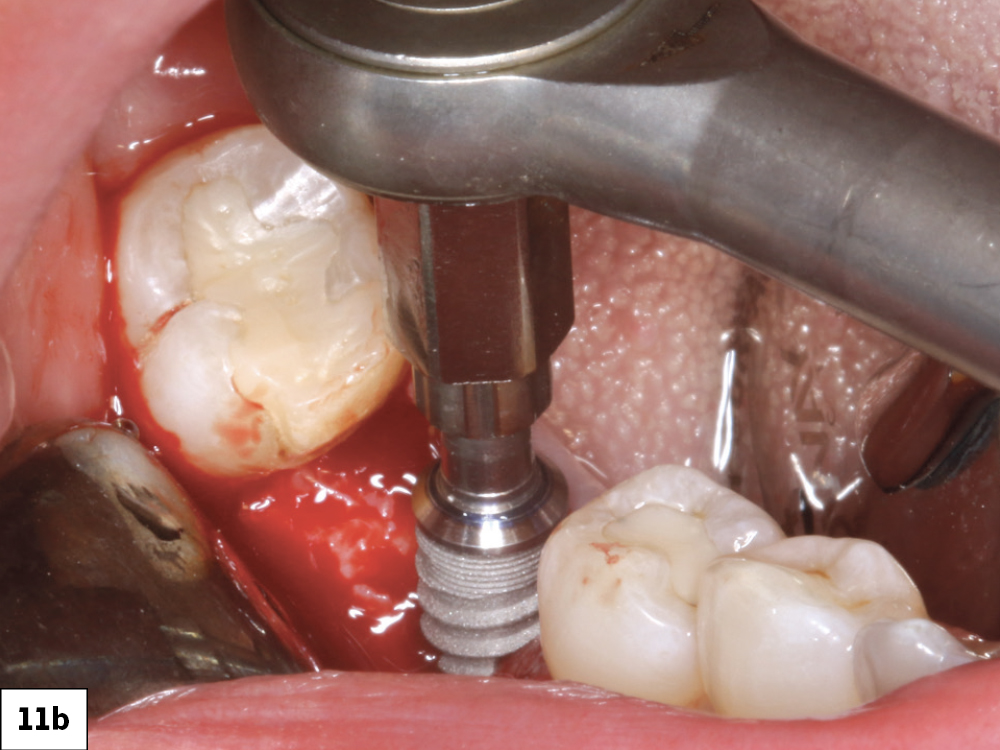
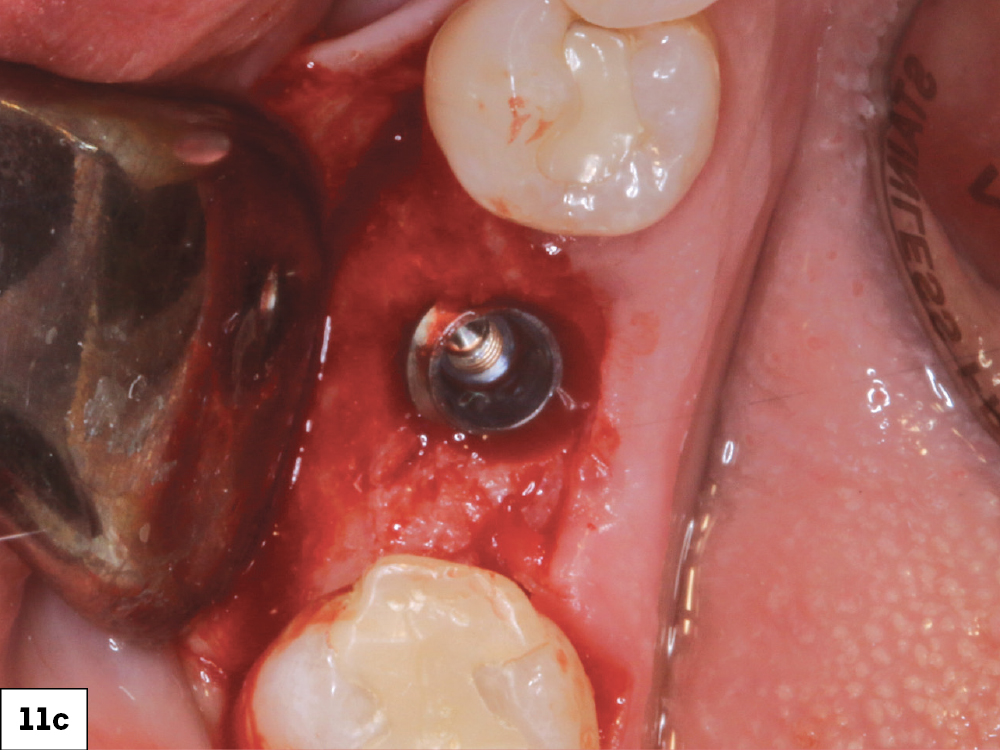
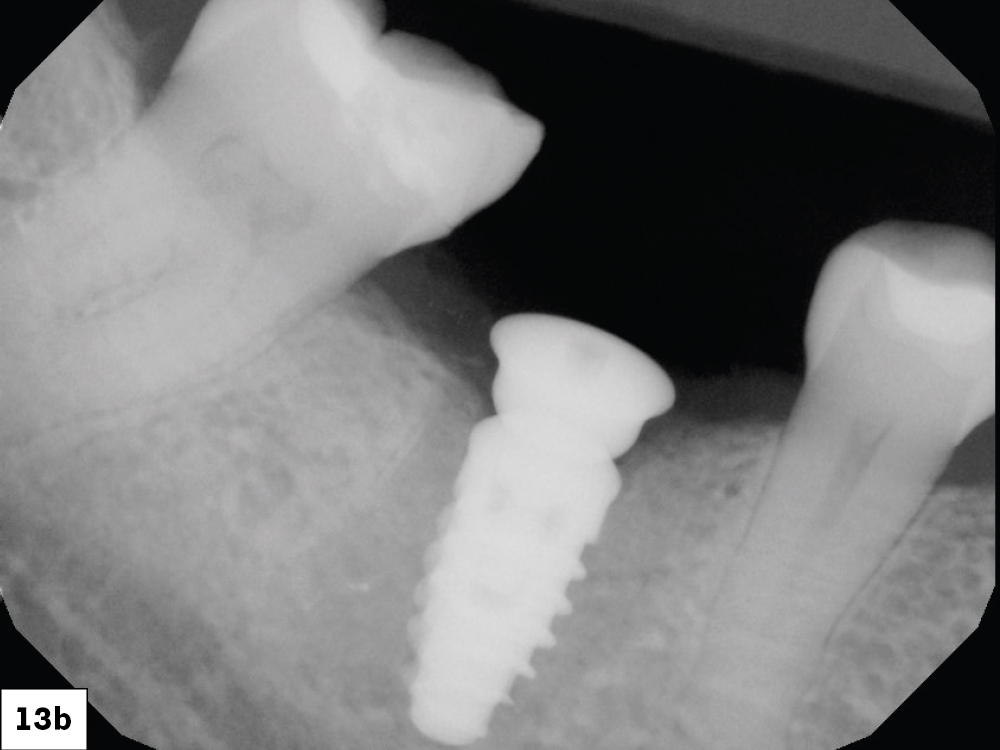
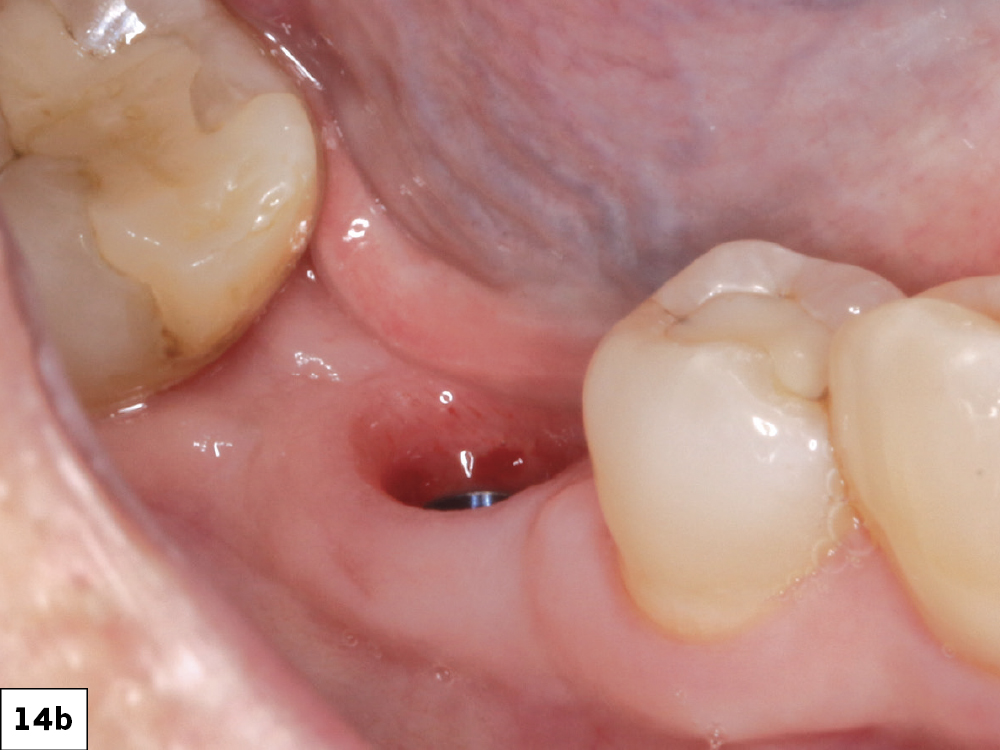
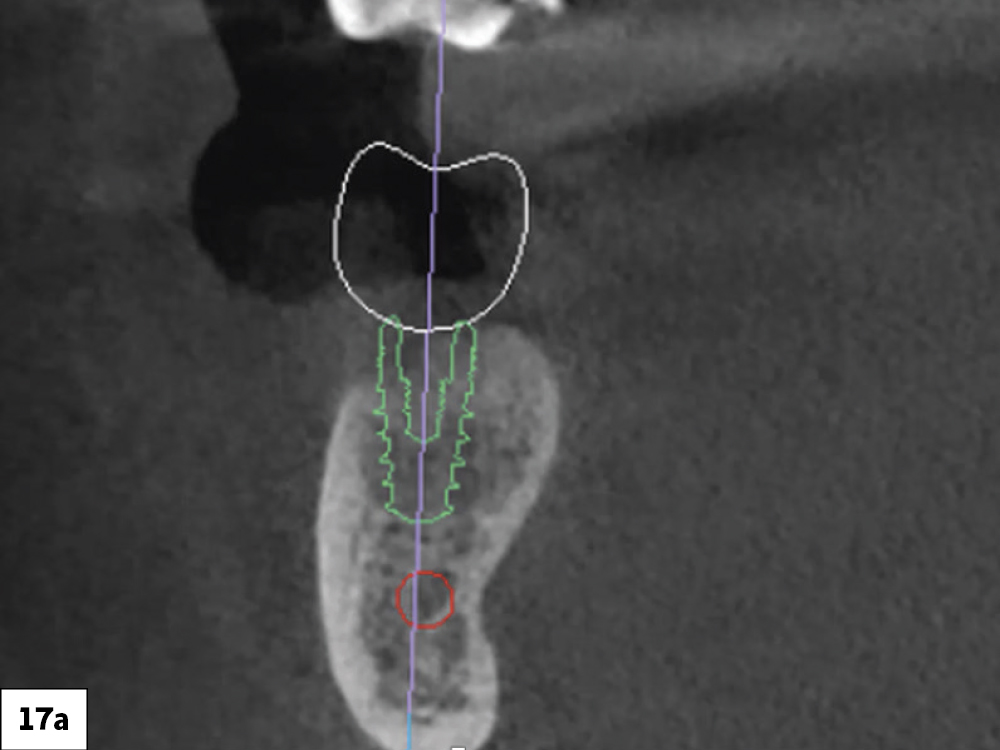
The patient in this case study presented with a failing, endodontically treated lower right first molar. At the time of tooth extraction, the clinician must decide whether to immediately place the implant or graft the site to ensure there will be adequate hard tissue for future implant placement. In this case, because I noted a defect in the facial wall of the socket, I determined that a grafting procedure and healing period were required prior to implant placement.
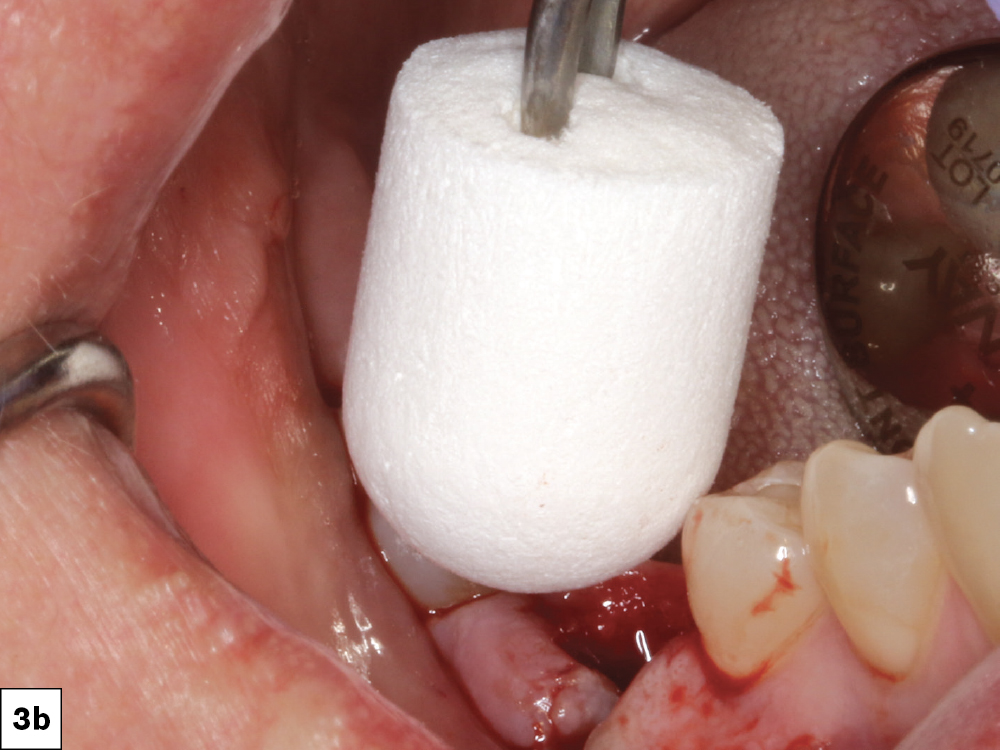
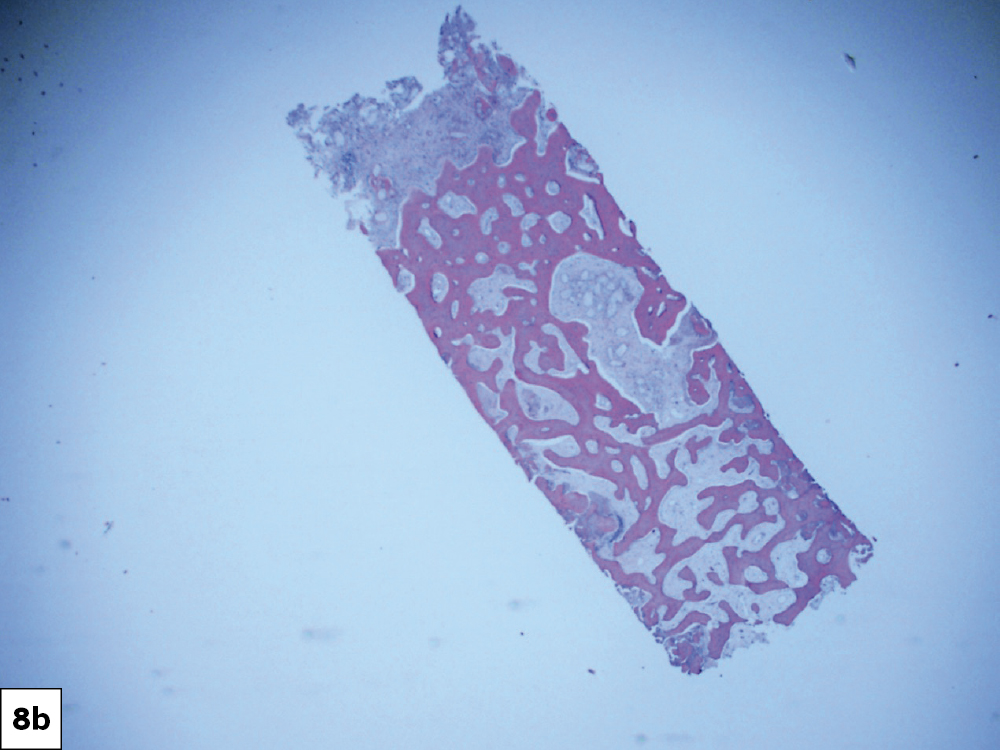
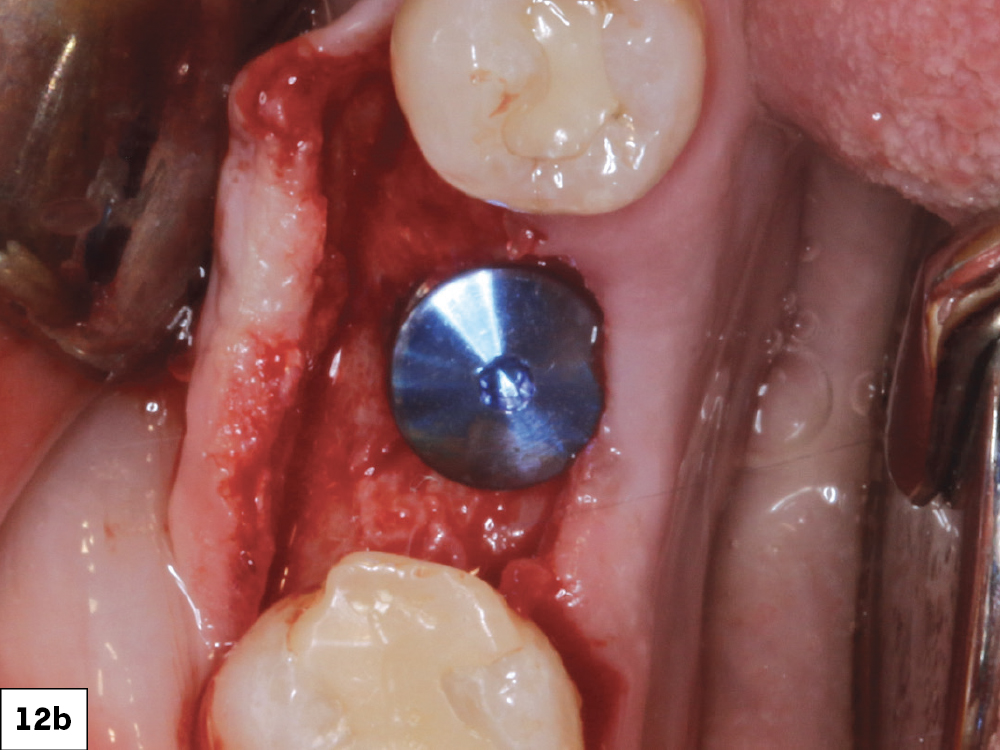
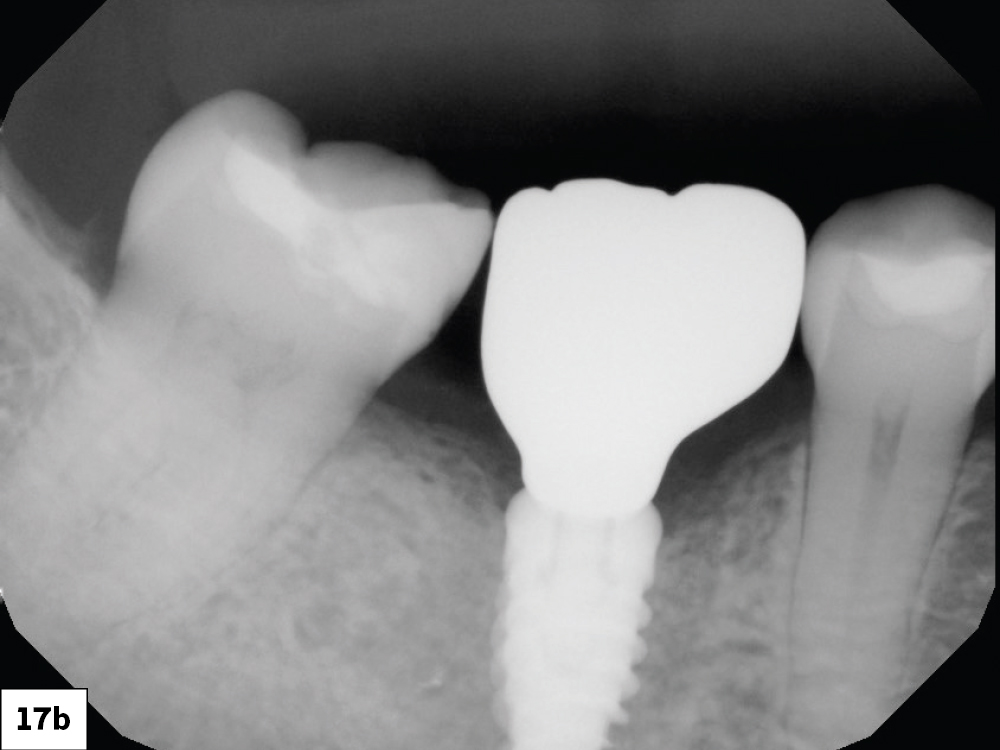
An OsteoGen® Plug (Glidewell Direct; Irvine, Calif.) was the material of choice for this socket grafting procedure due to its quality and predictability. The final restoration of the integrated implant was placed using a BruxZir® screw-retained crown fabricated by the team at Glidewell to support the optimal emergence profile.
At the time of tooth extraction, the clinician must decide whether to immediately place the implant or graft the site to ensure there will be adequate hard tissue for future implant placement.
CONCLUSION
Recognizing when socket grafting is necessary for the long-term health of an implant restoration is a vital part of implant dentistry. With the methods used in this case study, dentists can be better equipped to provide quality care for their patients. By providing the necessary bone grafting materials, instruments, implants and precise-fitting restorations, Glidewell Implant Solutions enables doctors to perform implant procedures with ease and repeatability.
OsteoGen is a registered trademark of IMPLADENT, LTD. Reli and REDISORB are registered trademarks of Myco Medical Supplies, Inc.