Laboratory and Chairside Partnership for a Full-Mouth Restoration

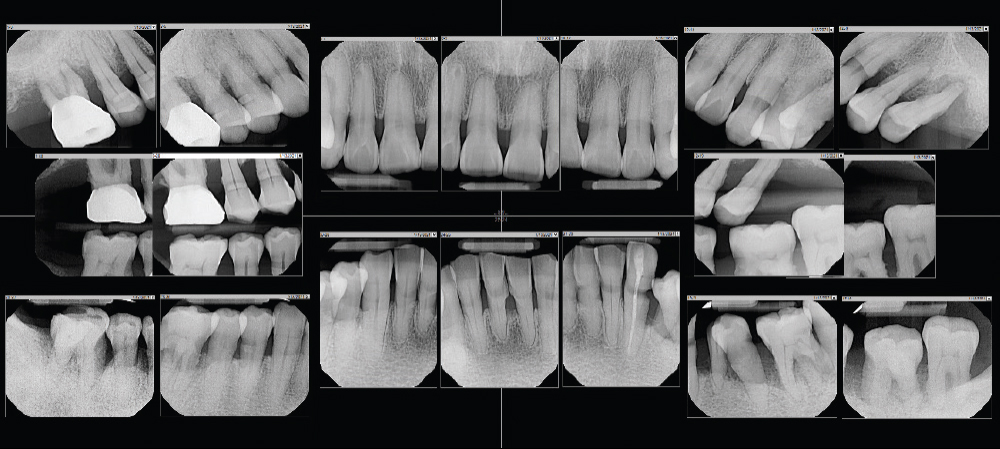
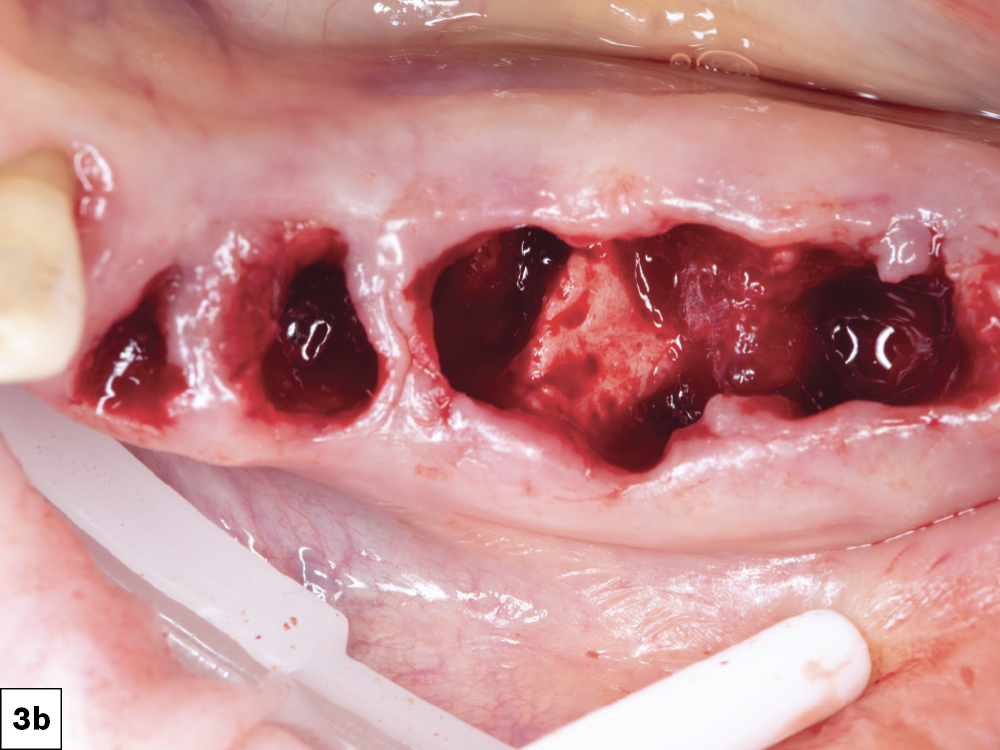
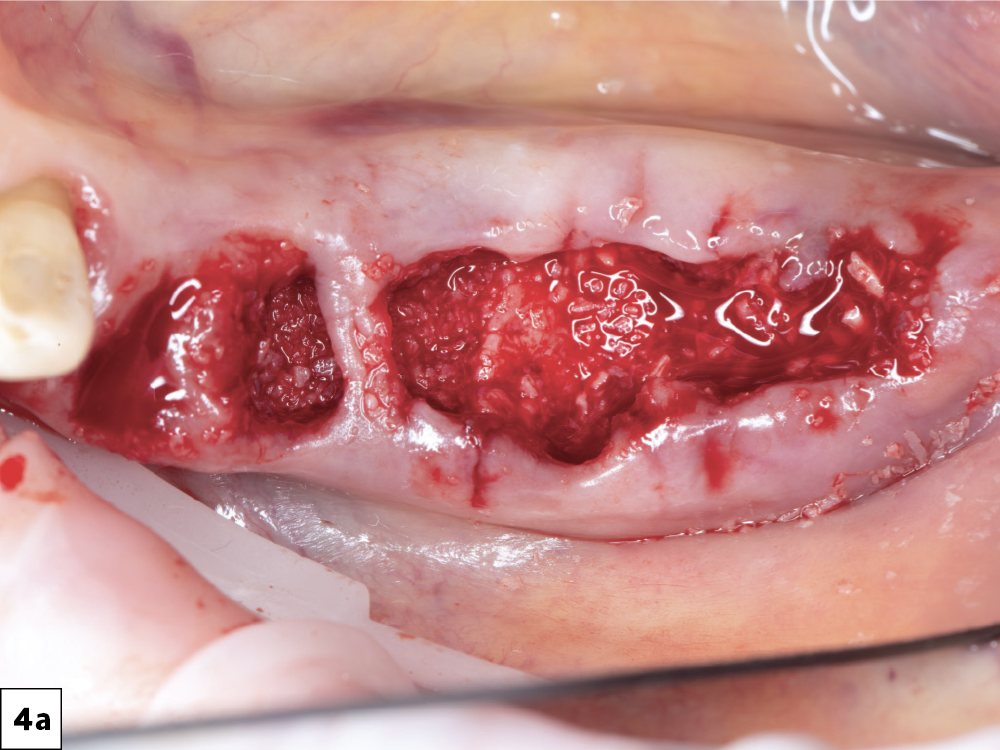
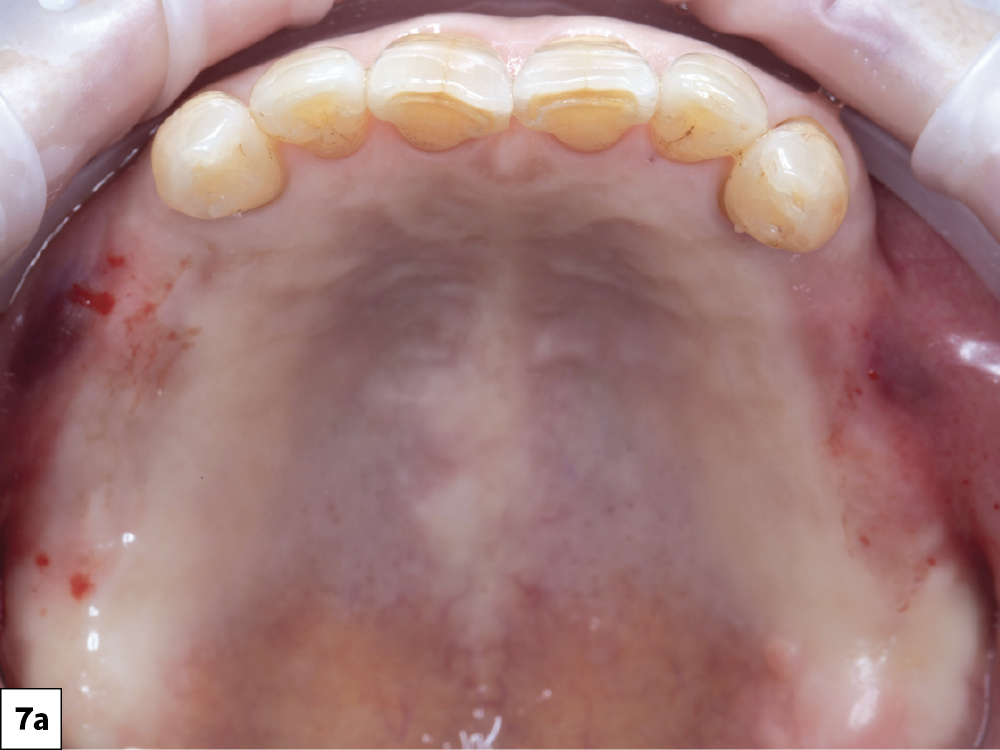
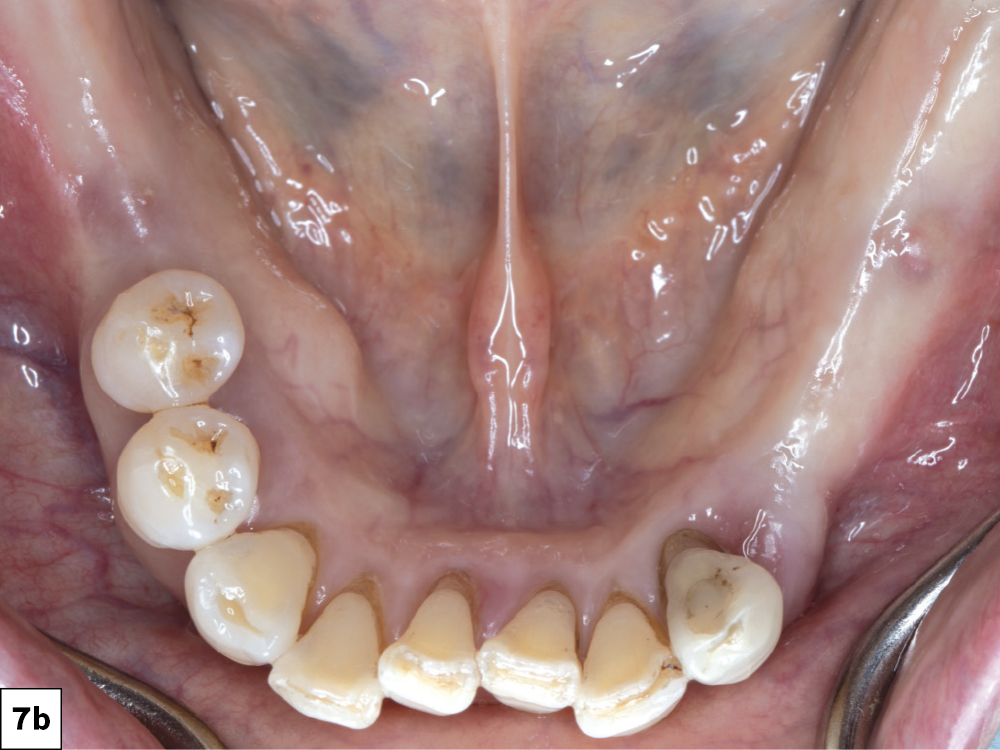
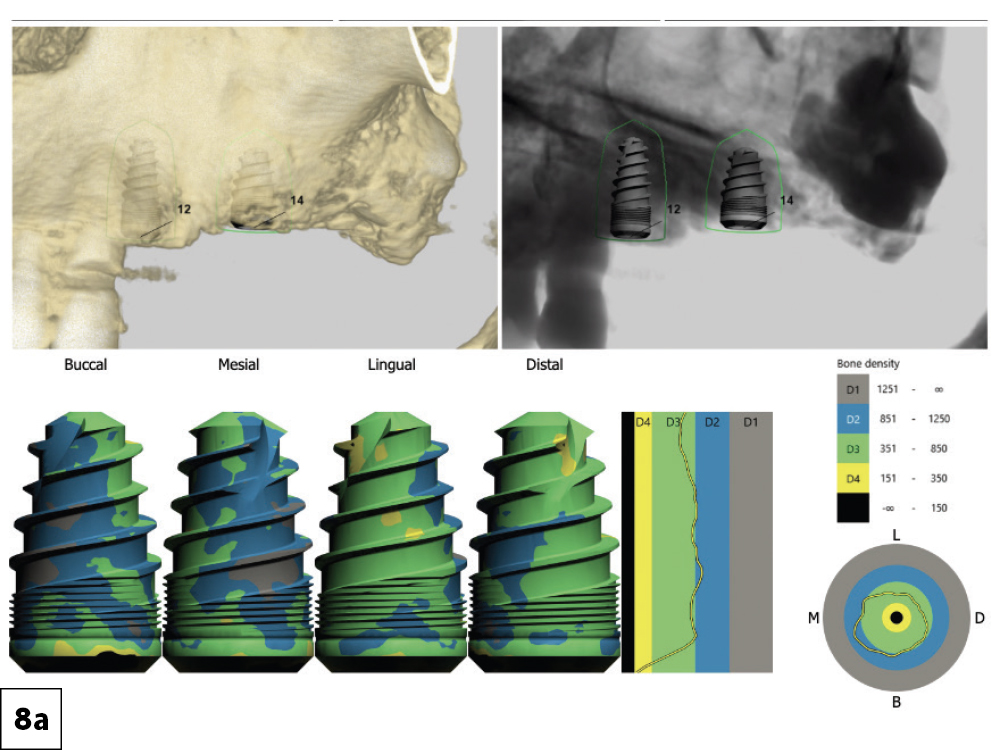
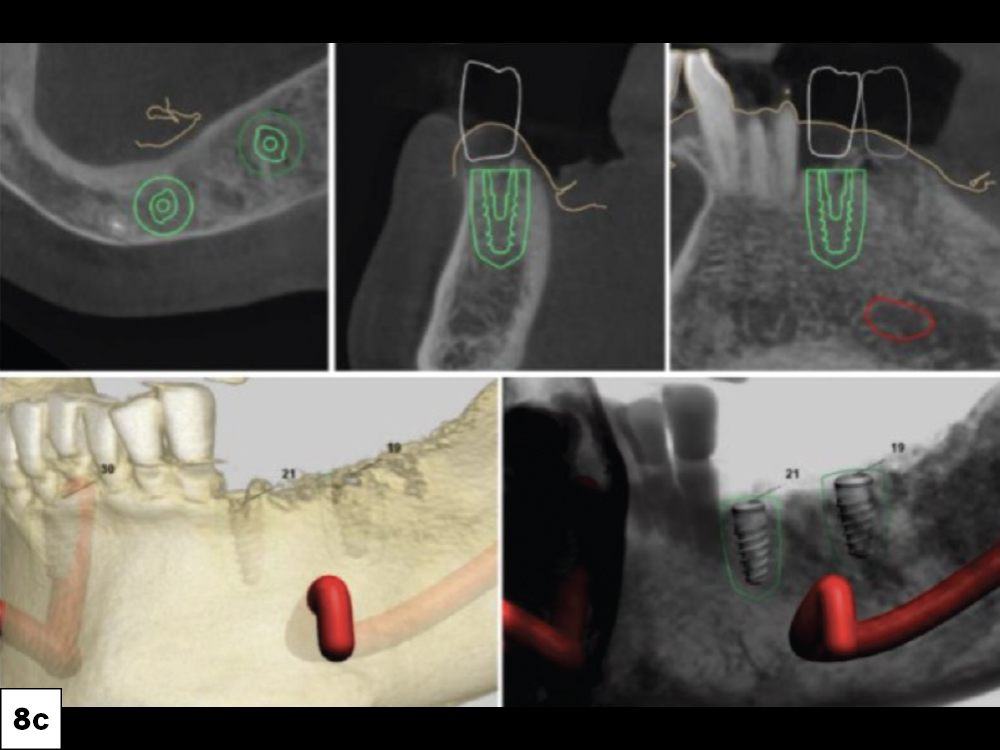
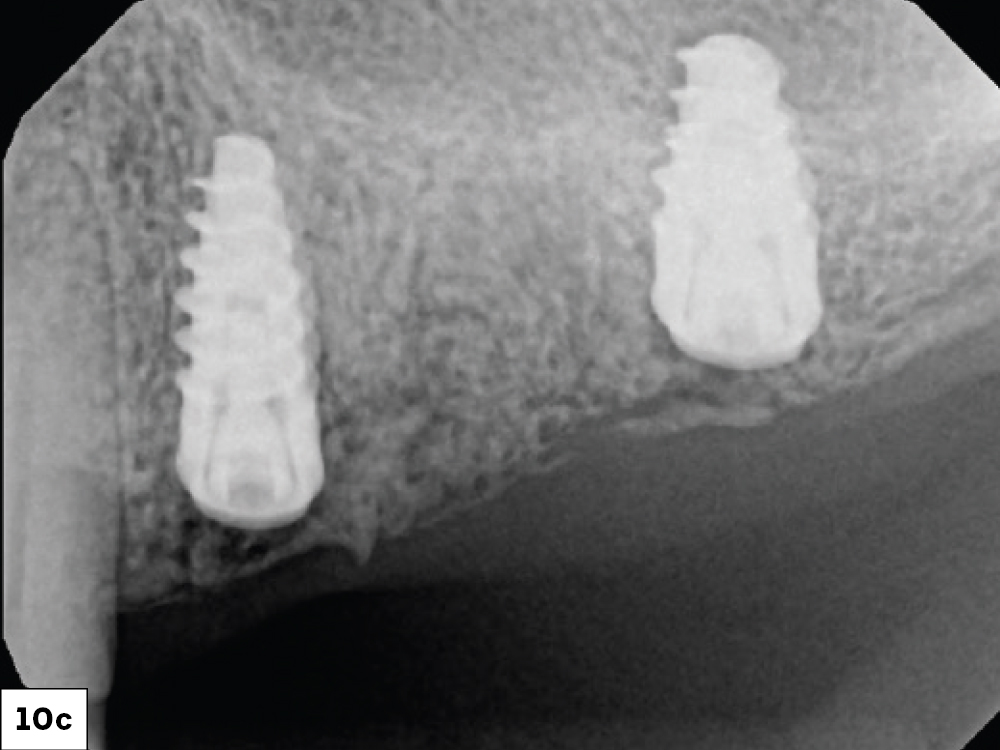
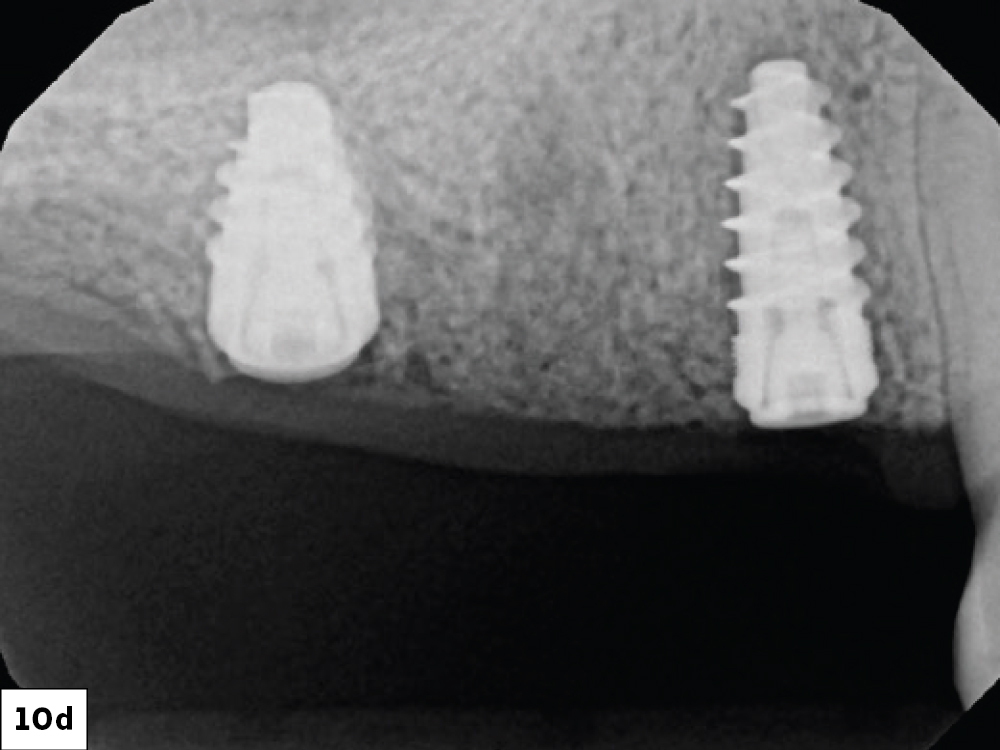
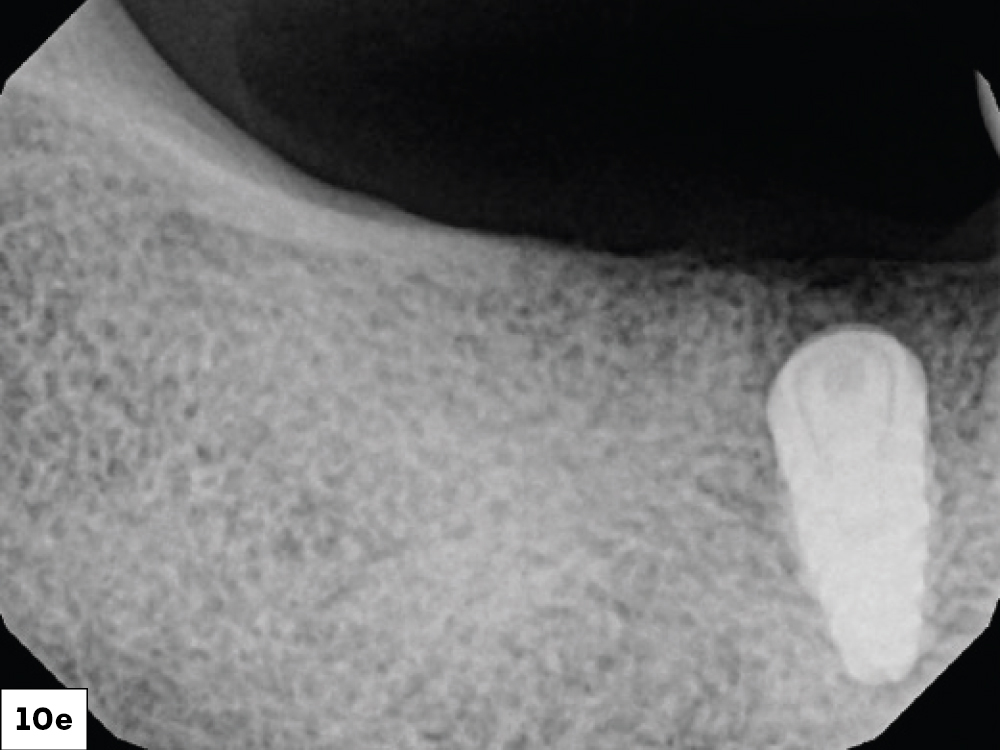
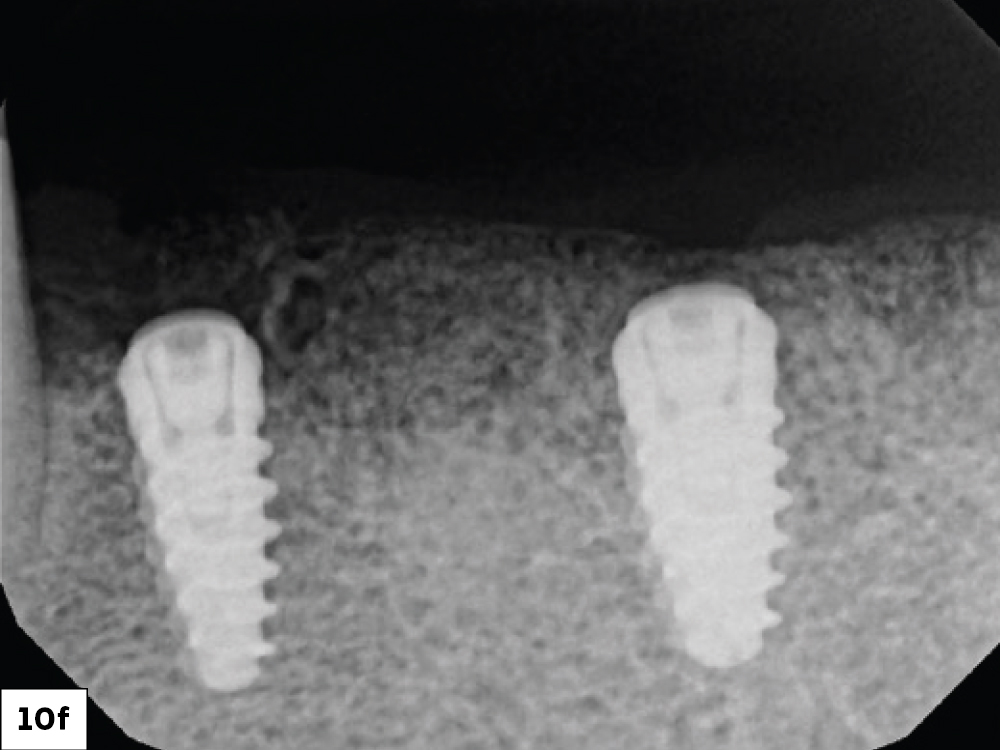
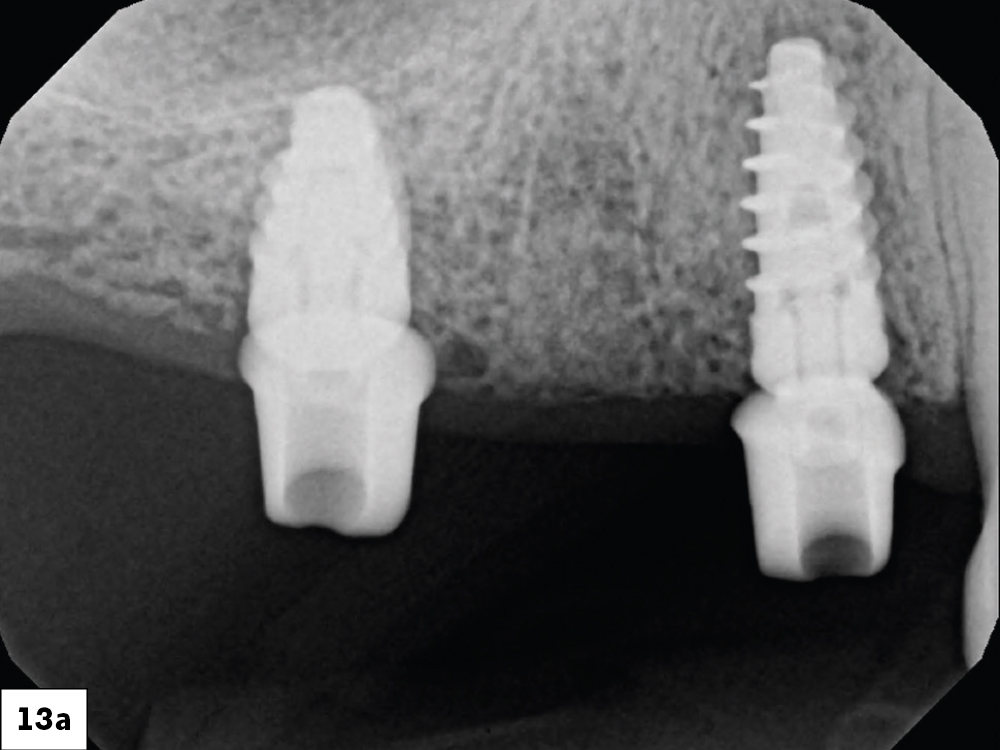
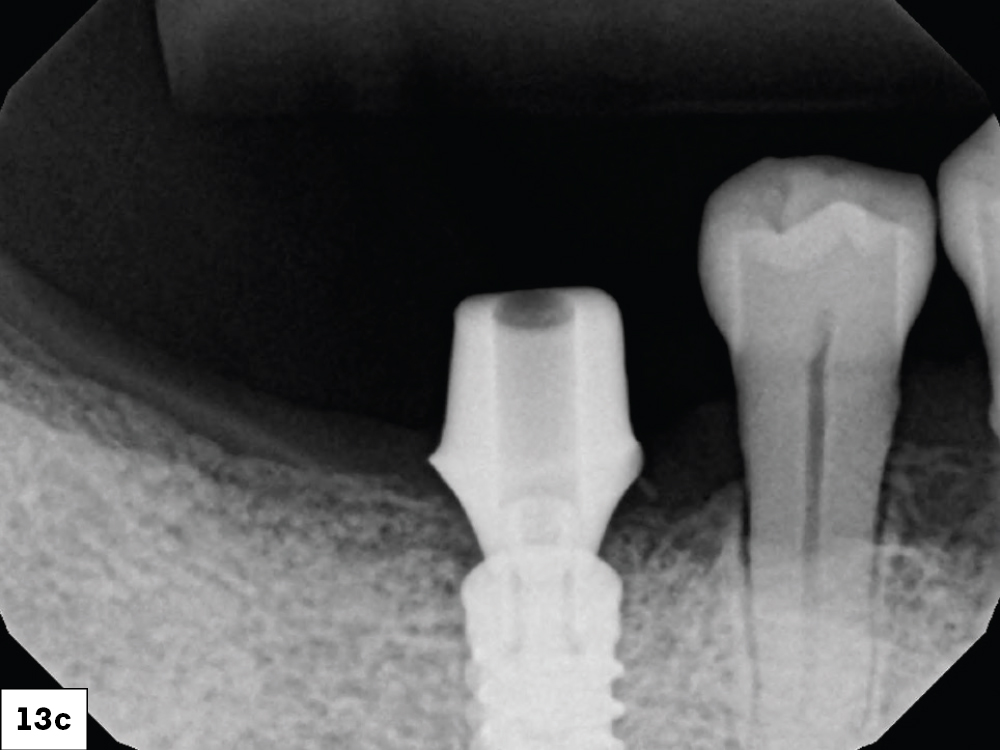
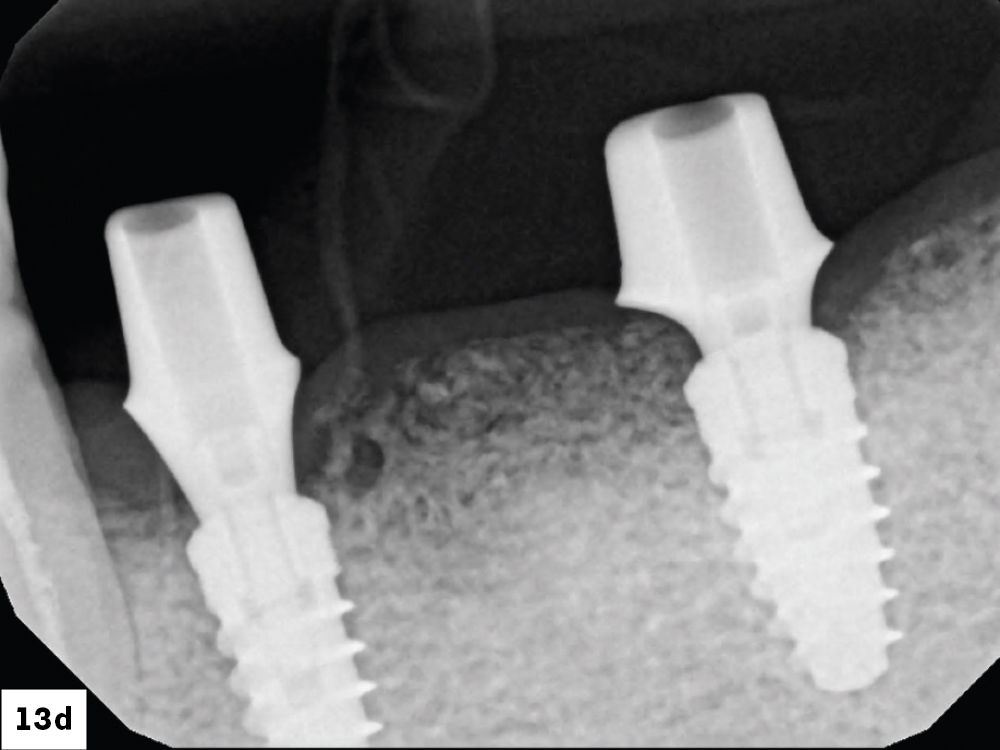
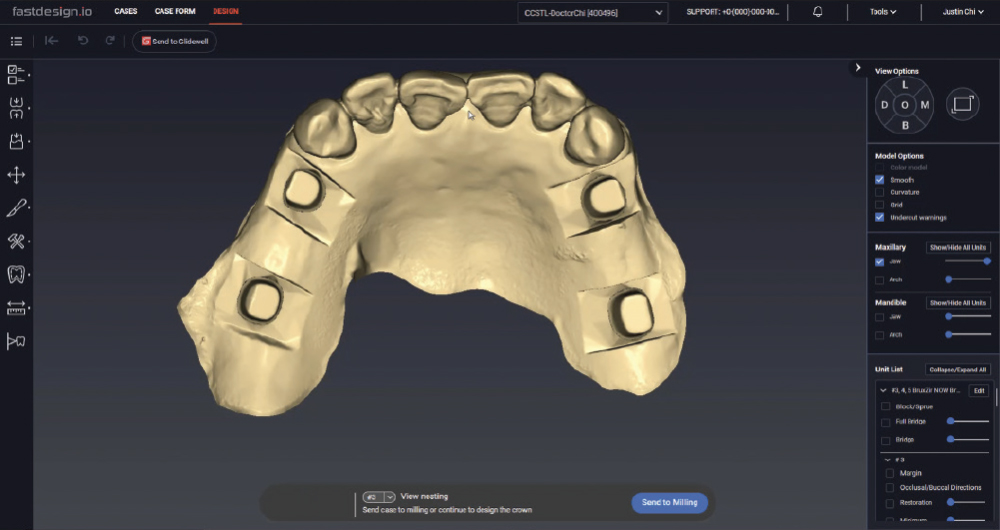
Obtaining the best outcome for our patients demands meticulous planning and attention to detail. In this article, I will highlight the advantages of combining both the laboratory and chairside processes to digitally plan and complete a complex full-mouth case.
CONCLUSION
Advanced technologies like cone-beam scanning, digital treatment planning and 3D printing, allow clinicians and lab professionals to work in concert. As these workflows have become increasingly accessible and user-friendly, clinicians have a more predictable pathway for achieving success with full-mouth restorations.
All trademarks are property of their respective owners.