A Long-Delayed Full-Mouth Restoration (1 CEU)
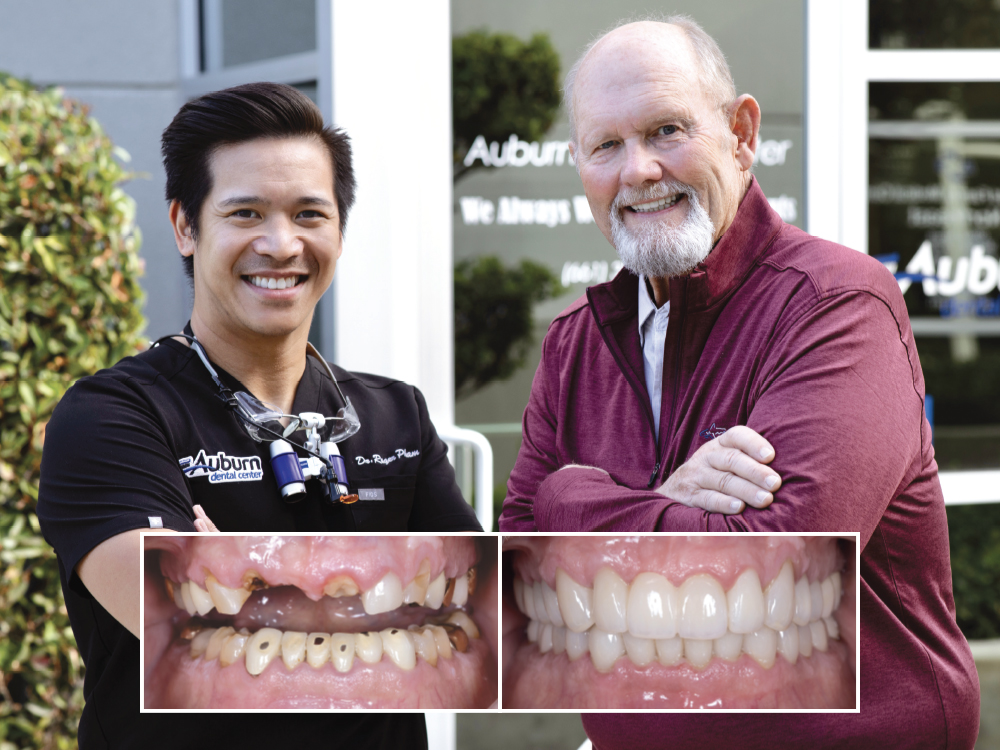
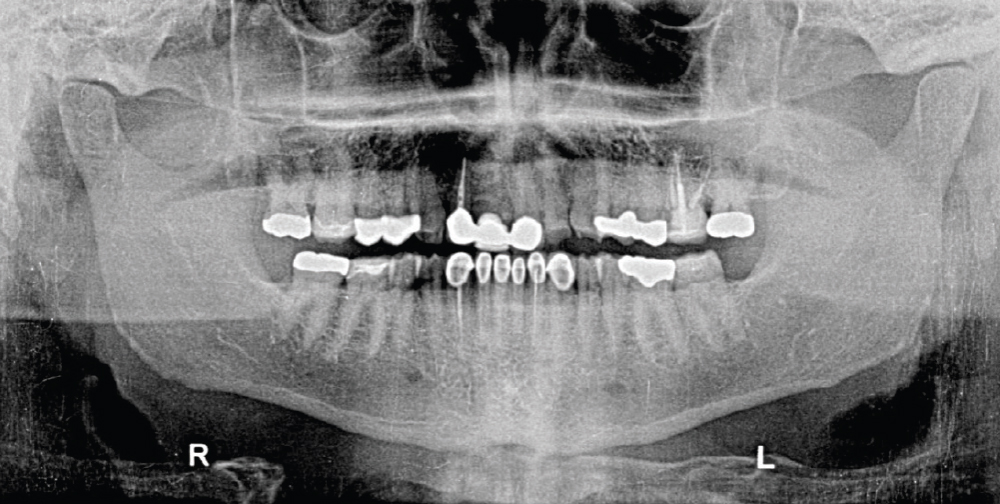
Tim is a recently retired schoolteacher who came to my practice looking for help. For decades, he had focused his attention on his students, ensuring that they had the scholastic tools for success. But, in his retirement, Tim realized he had been putting off addressing his worsening oral health. When Tim’s anterior bridge came off, he realized additional patchwork would not solve his dental concerns.
I discussed with Tim the possibility of a comprehensive and definitive full-mouth restorative solution. With more time and improved financial resources in retirement, he agreed.
CASE REPORT
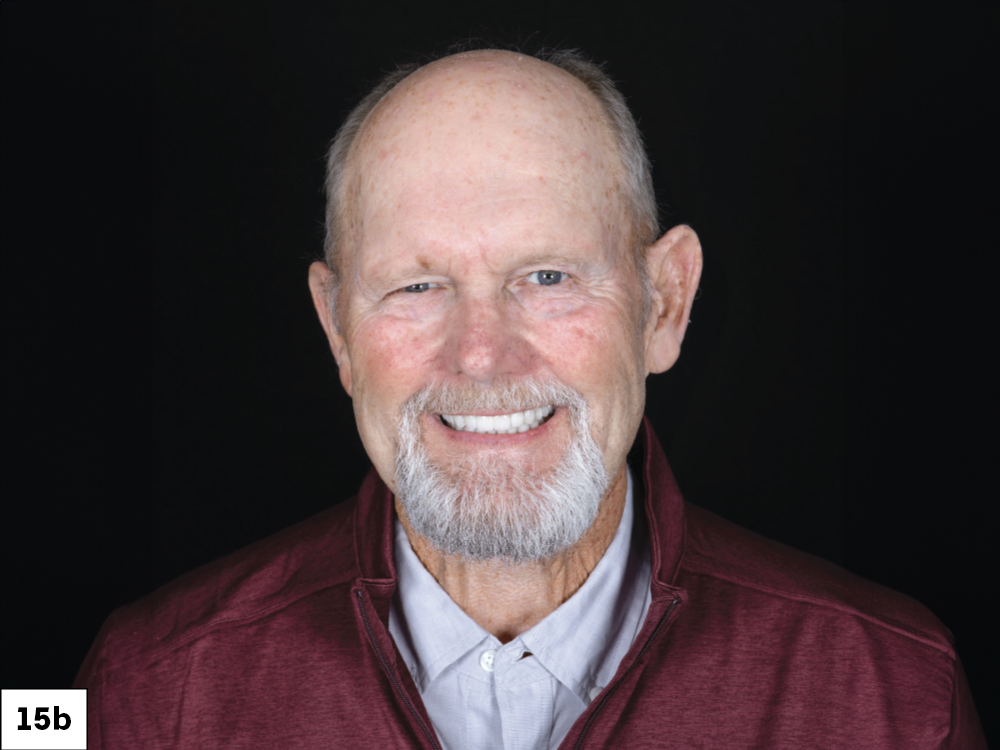
CONCLUSION
Tim was extremely pleased with the functional and esthetic results achieved. For a variety of reasons, patients often put off finding a definitive solution for their dental challenges. The valuable lesson here is that dental patchwork has limitations, and that by discussing treatment options with your patients you will find that they will often approach you when they’re ready.