Socket Grafting and Immediate Implant Placement in the Esthetic Zone: A Case Study (1 CEU)

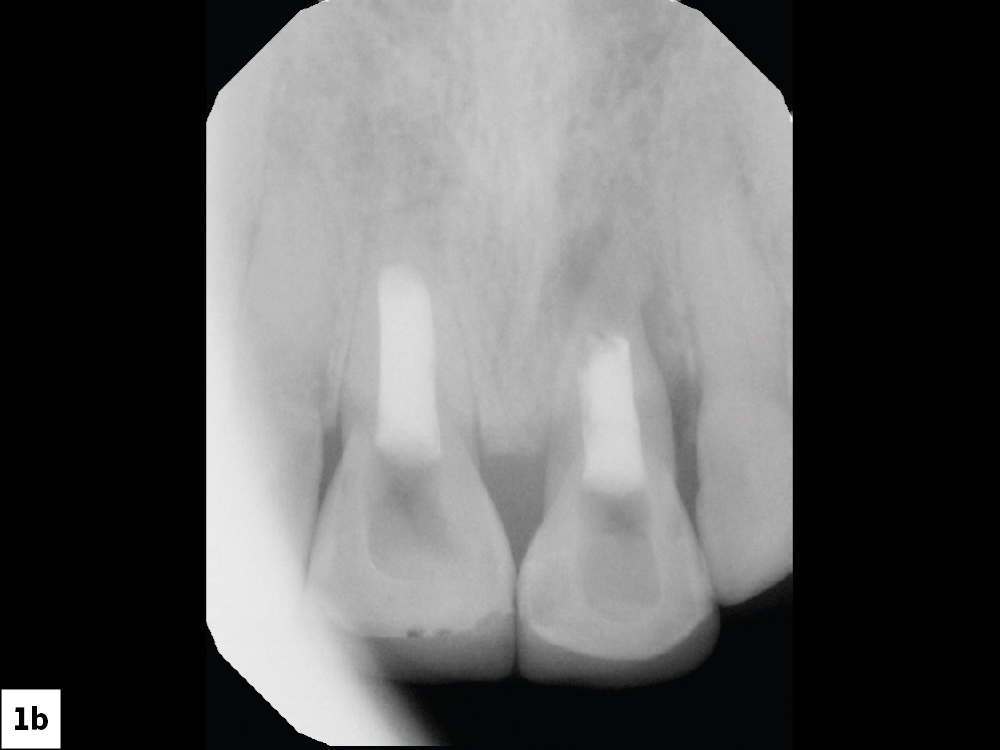
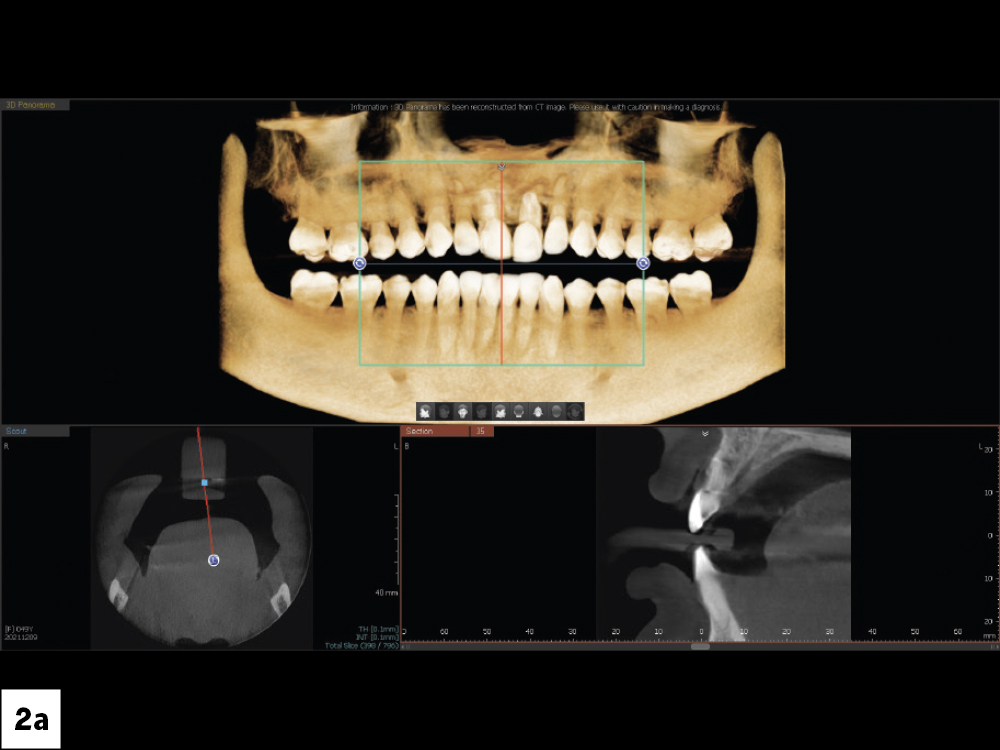
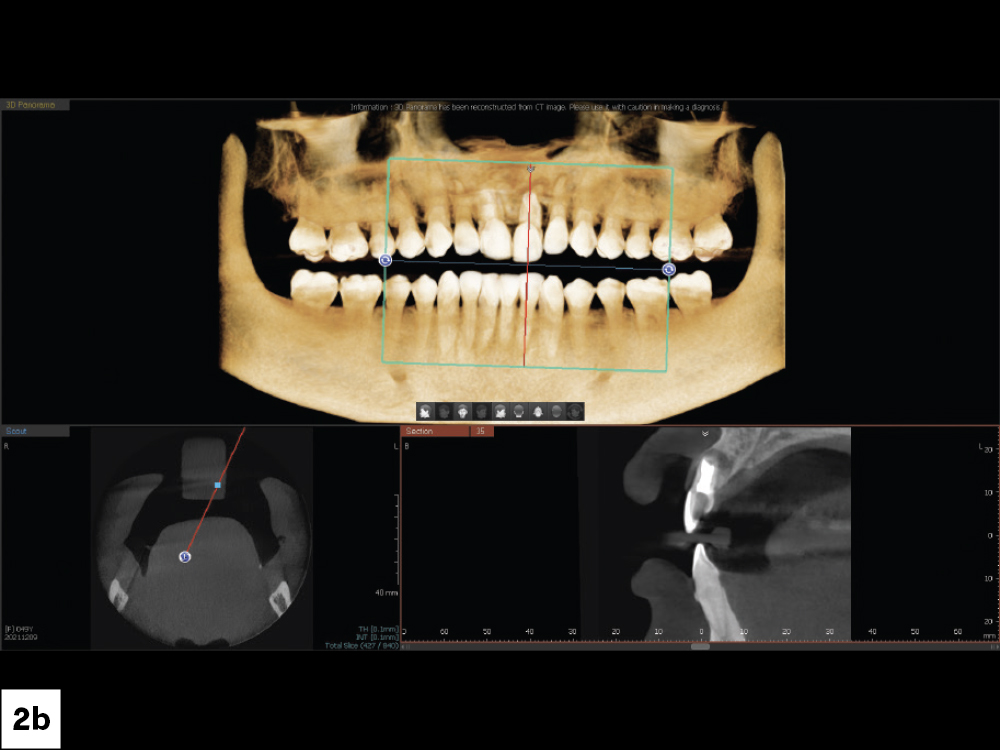
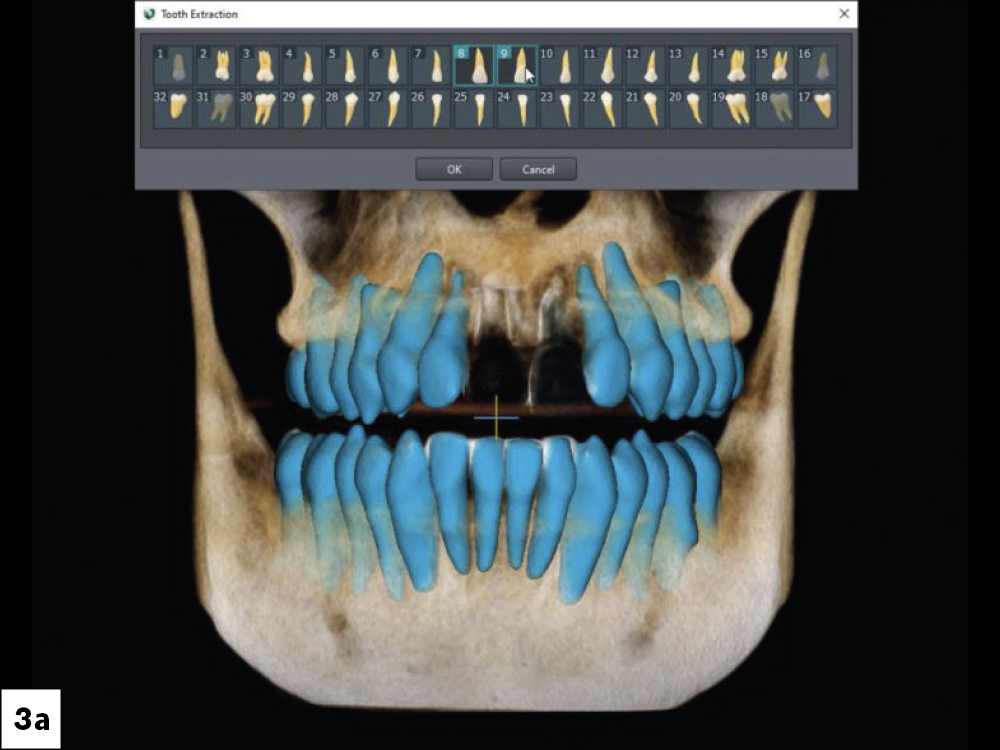
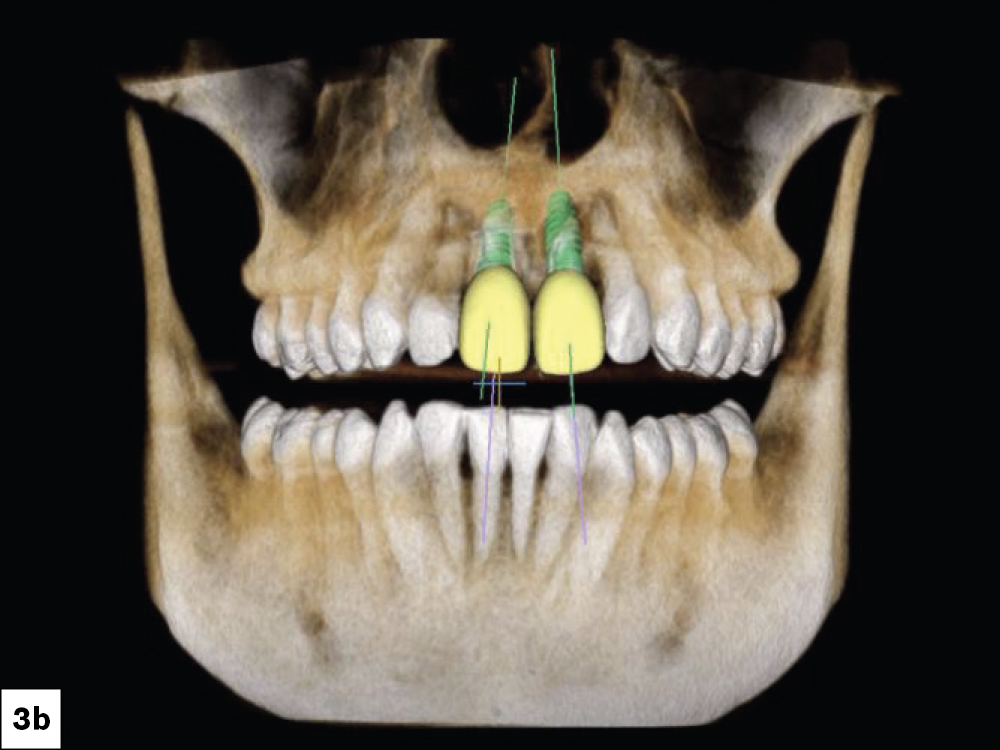
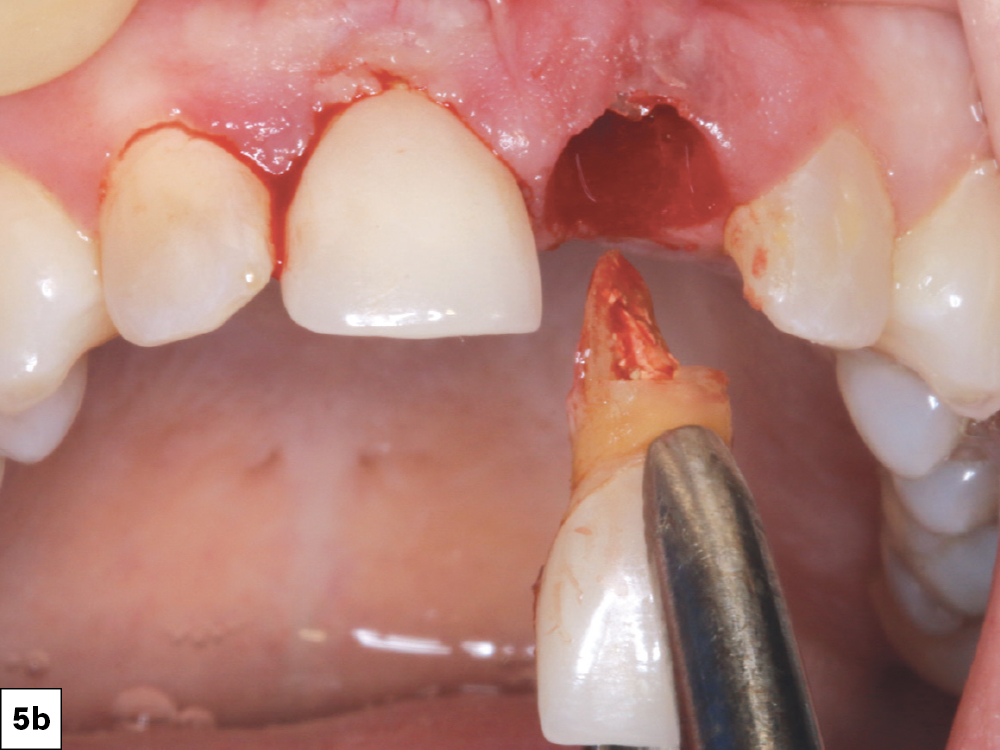
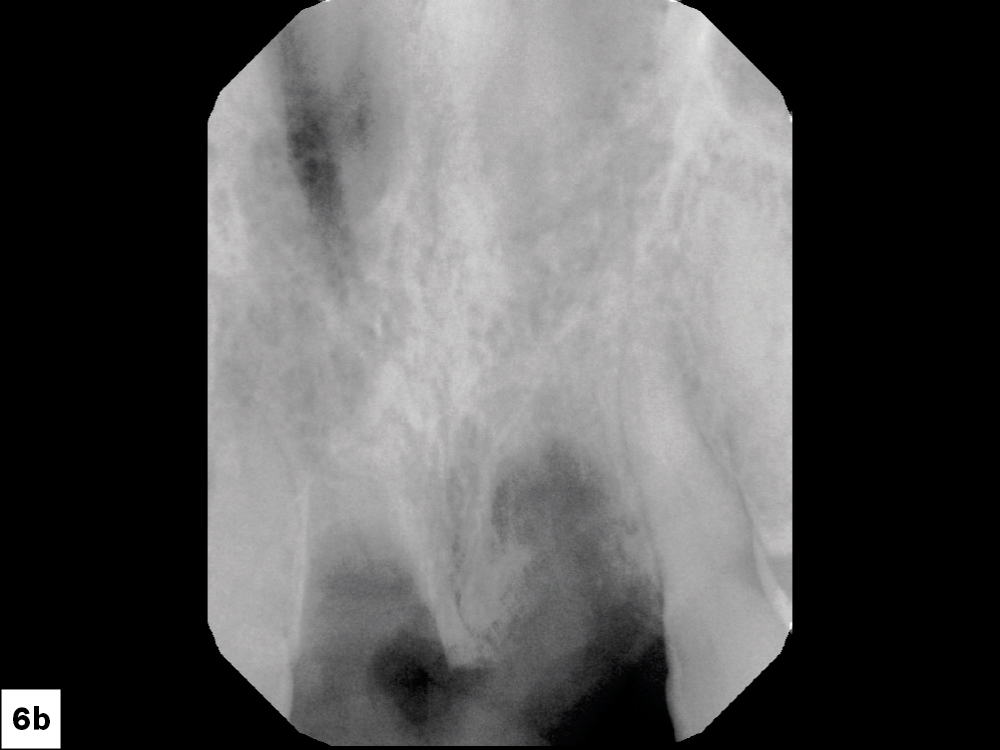
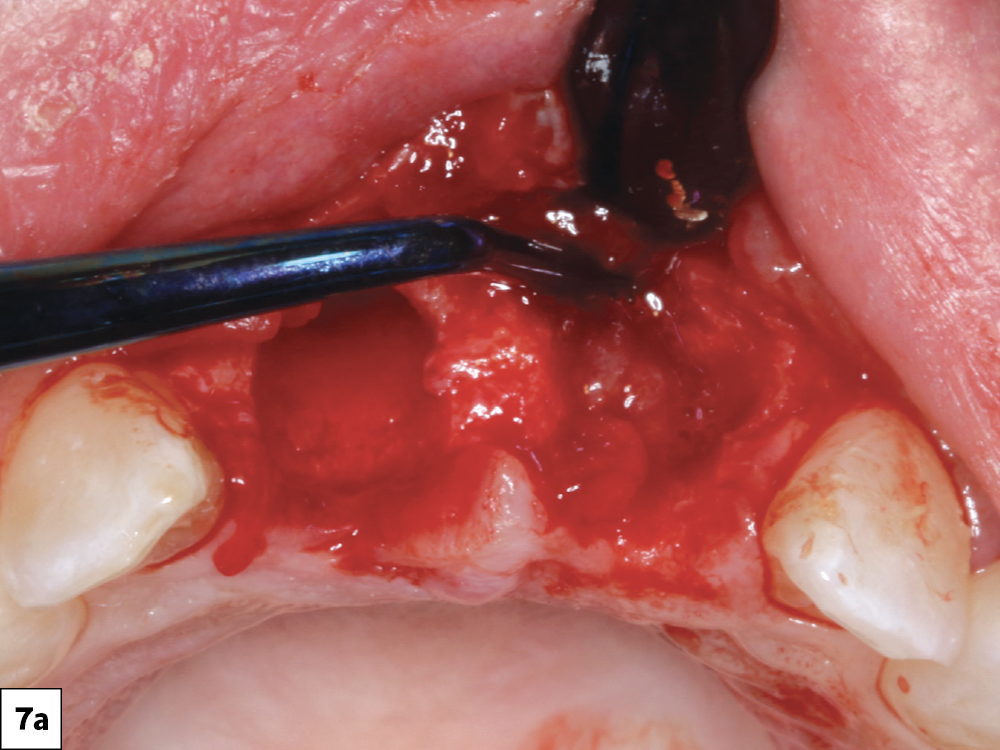
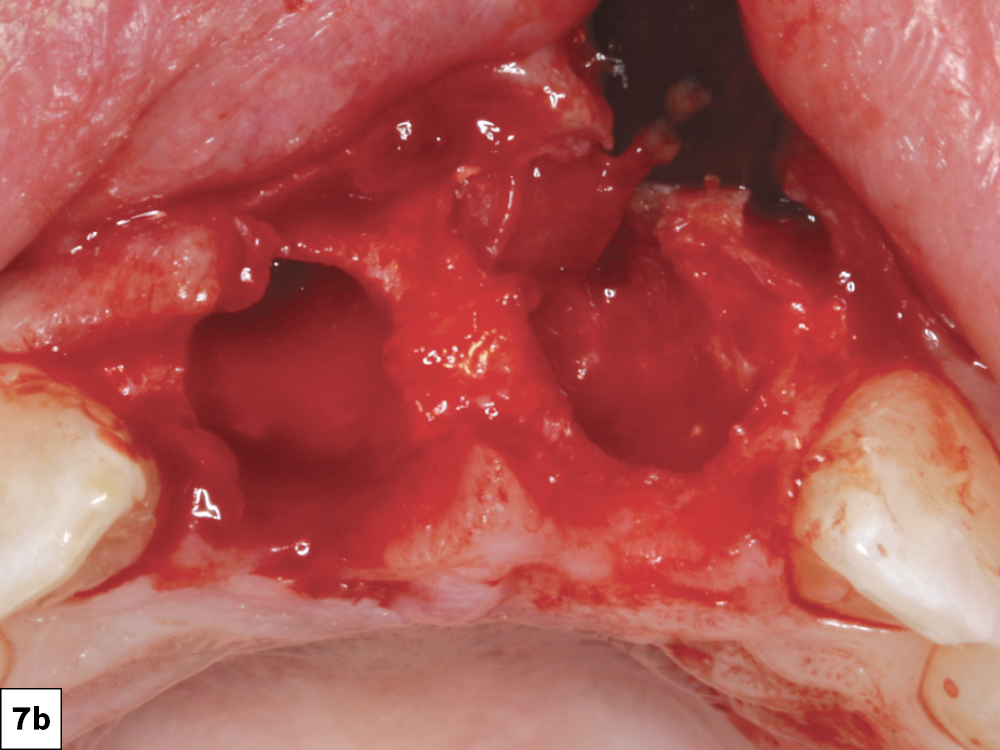
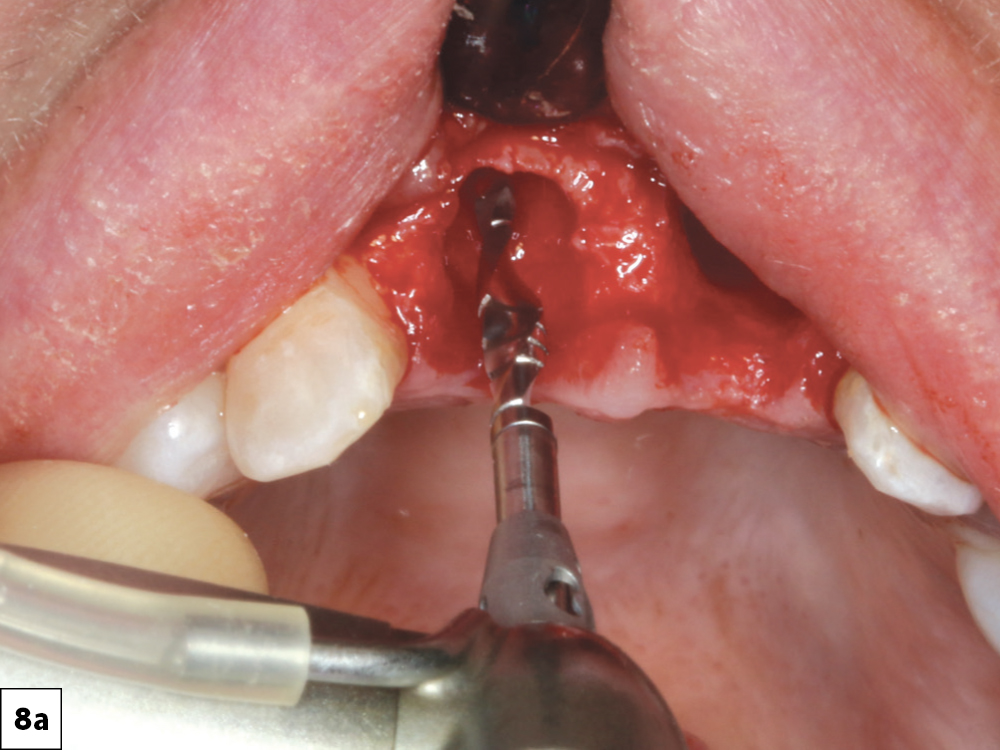
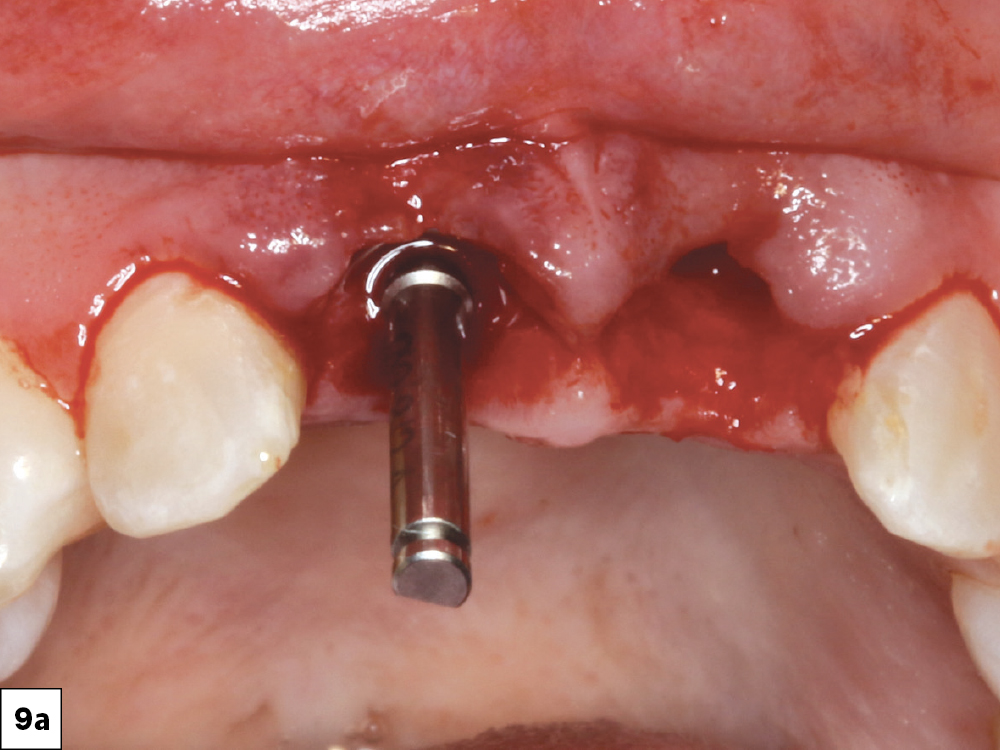
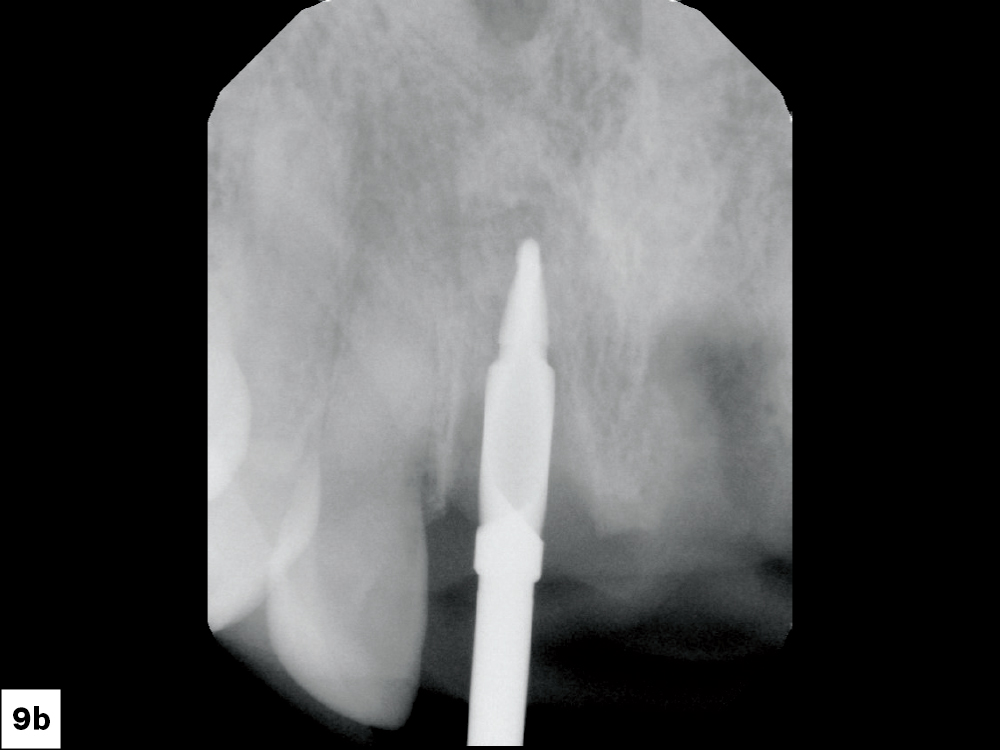
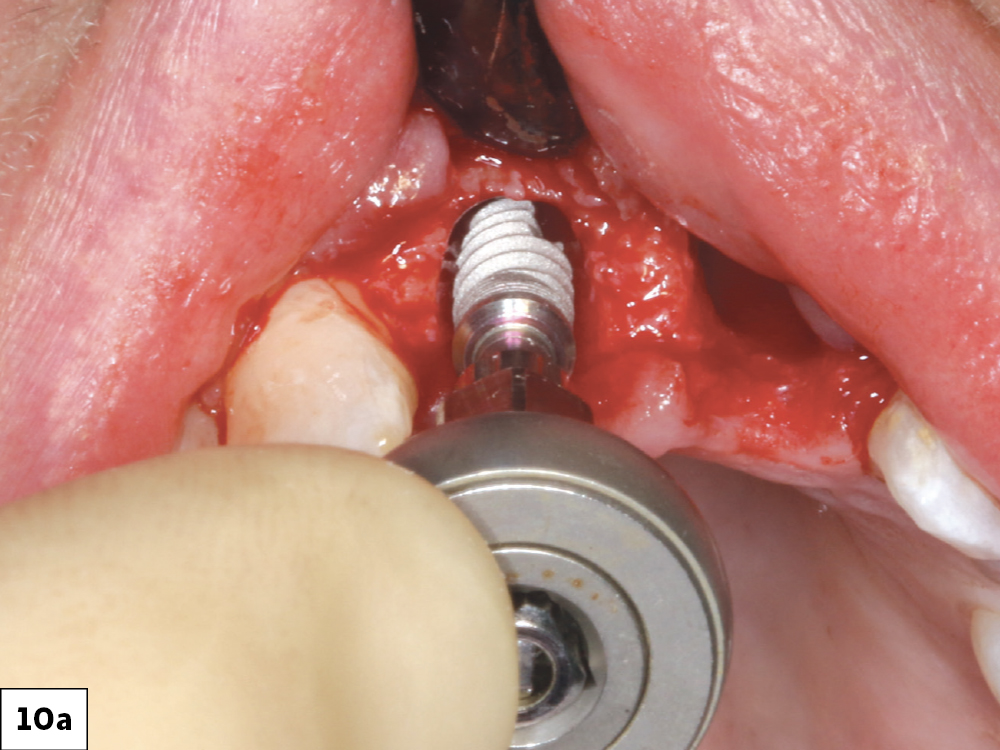
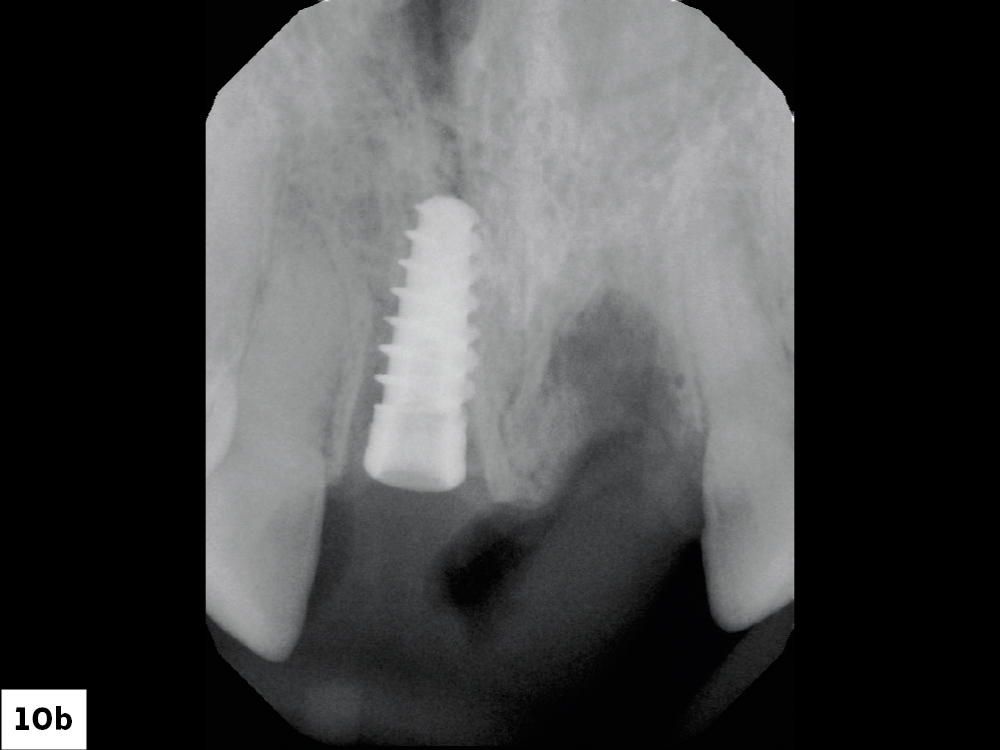
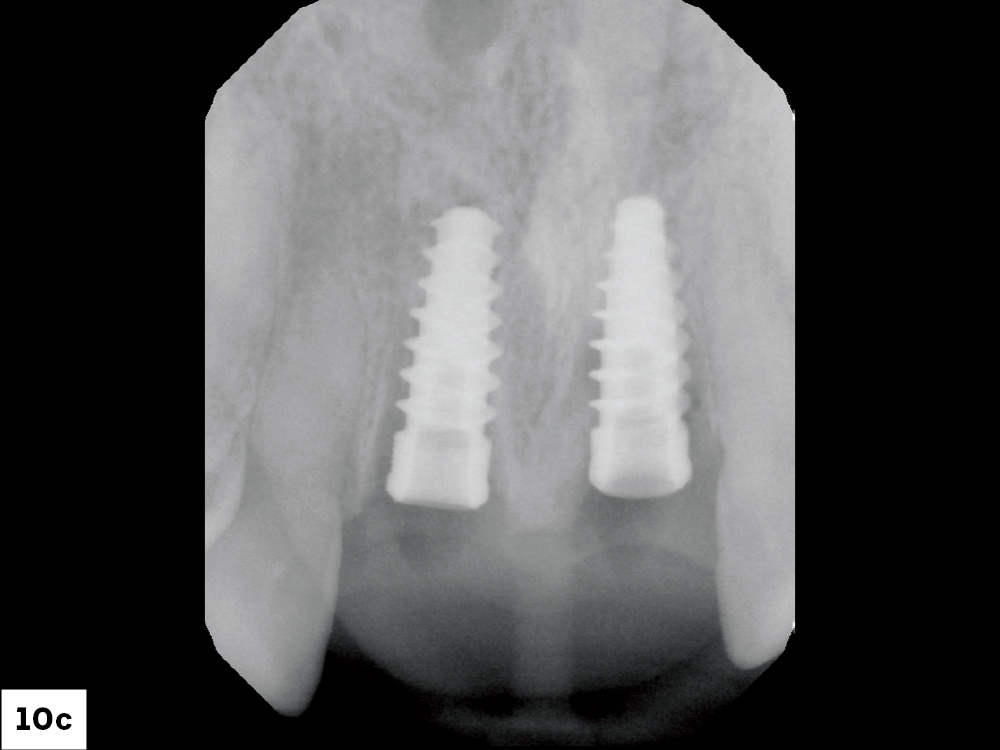
This patient presented with the chief complaint of mobile, endodontically treated maxillary central incisors. Her history revealed the traumatic avulsion and reimplantation of these teeth during her adolescence. Significantly she also had a high smile line with several millimeters of gingival display, a common hurdle dentists encounter. In a case like this, designing and executing the optimal treatment plan that results in long-term implant stability and good esthetics is the ultimate challenge. In fact, determining whether this case should be undertaken is the first and most crucial step.
CASE STUDY
CONCLUSION
It’s vital to be able to recognize which cases to accept and which cases require more experienced hands. By following the steps outlined in this case and adopting a measured approach with CBCT analysis, doctors can feel confident in selecting the right cases for their practice. Whether it’s a single-tooth implant placement in the posterior or a more demanding anterior restoration, good case assessment and the support of an experienced lab can help provide the best results for one’s practice.