Do’s and Don’ts of Intraoral Scanning for Implant Restorations (1 CEU)

The digital revolution has transformed how we approach implant treatment planning, placement and restorative execution. While digital scanning has become increasingly accessible and user-friendly, the difference between an unusable scan and an exceptional one often determines the success of the final restoration. The quality of the digital impression directly impacts everything: the accuracy of the surgical guide, the fit of the provisional and definitive restorations, and ultimately the long-term success of the implant.
This guide distills the essential principles that separate successful digital scanning from frustrating failures. Whether you are new to intraoral scanning or looking to refine your technique, understanding these fundamental do’s and don’ts will help you better utilize digital technology in your implant practice. From pre-scan preparation to post-processing protocols, we will explore the critical decisions that ensure your digital impressions serve as a reliable foundation for implant excellence.
PRE-SCAN PREPARATION
The most sophisticated scanning technology cannot compensate for inadequate clinical preparation. What happens before you ever pick up the scanner wand ultimately determines whether your digital impression translates into a restoration that fits, functions and lasts. Investing time in a thorough pre-scan assessment and preparation prevents the frustration of beautiful digital files that yield problematic restorations.
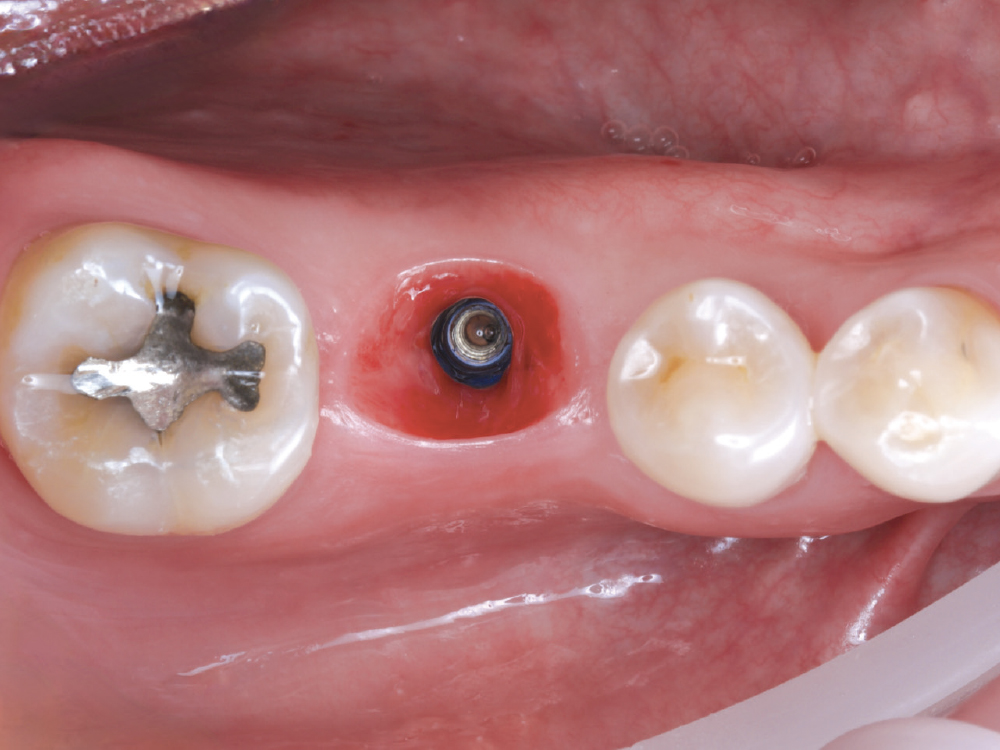
Verify the Emergence Profile. Contouring the soft-tissue architecture around the implant site to create an ideal emergence profile before scanning is essential. The tissue must be appropriately shaped to support the final restoration, and adequate healing time after contouring should be allowed to achieve stable, mature soft-tissue contours. A well-defined, digitally captured emergence profile translates directly into better-fitting restorations that integrate naturally with the surrounding tissues.
Verify the Path of Draw. Creating clear guide planes on adjacent teeth establishes a predictable path of insertion and helps minimize black triangles, which is critical for both single-implant and multiple-unit cases. Create an intentional path of insertion before scanning to guide laboratory fabrication, carefully considering the relationship between the long axis of the implant and the adjacent contacts. This foundational step ensures the restoration can be inserted and removed without binding or damaging adjacent structures.
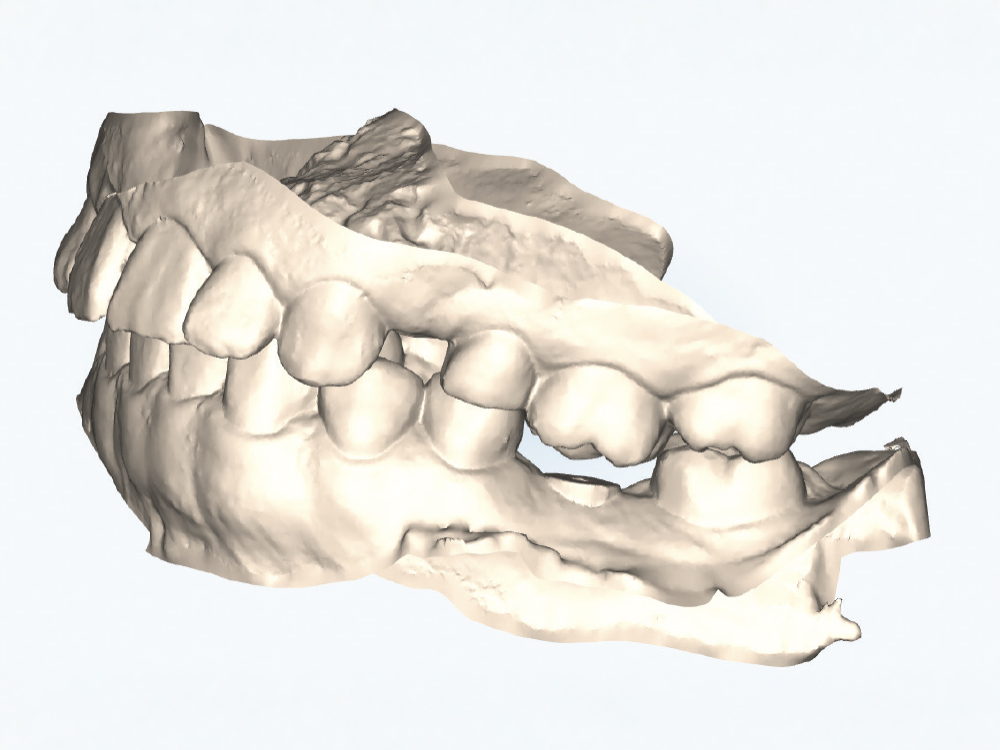
Clean Adjacent Teeth. All debris, plaque, and calculus must be removed from neighboring teeth before scanning, as the contamination will be captured in the digital impression and compromise accuracy. Pay special attention to interproximal areas and gingival margins where buildup tends to accumulate.
Assess Restorative Space. Evaluating the available vertical dimension before proceeding with scanning helps identify potential problems before they become costly mistakes. Look for supraerupted opposing dentition that may compromise restorative space and document any plunging opposing cusps that could interfere with implant restoration design. Communicate space limitations to the laboratory before fabrication begins and consider equilibrating or restoring opposing teeth if needed to achieve adequate clearance.

Assess Parafunctional Habits. Evaluating signs of parafunctional habits, including bruxism or clenching, provides critical information that influences material selection and occlusal design. Share these findings with the laboratory to inform restoration fabrication decisions, ensuring the final prosthesis is designed to minimize harmful excursive forces during function.
Don’t Rush the Pre-scan Clinical Assessment. Skipping proper evaluation leads to restorations that do not fit or function optimally. Time spent on pre-scan preparation prevents costly remakes and adjustments.
THE SCAN
As scanning technology continues to advance at a remarkable pace, best practices evolve alongside it. What worked optimally two years ago may have been superseded by more efficient protocols today. Staying current with your scanner’s capabilities and understanding the fundamental principles of digital capture ensures you are maximizing the technology’s potential while minimizing frustration and remakes.
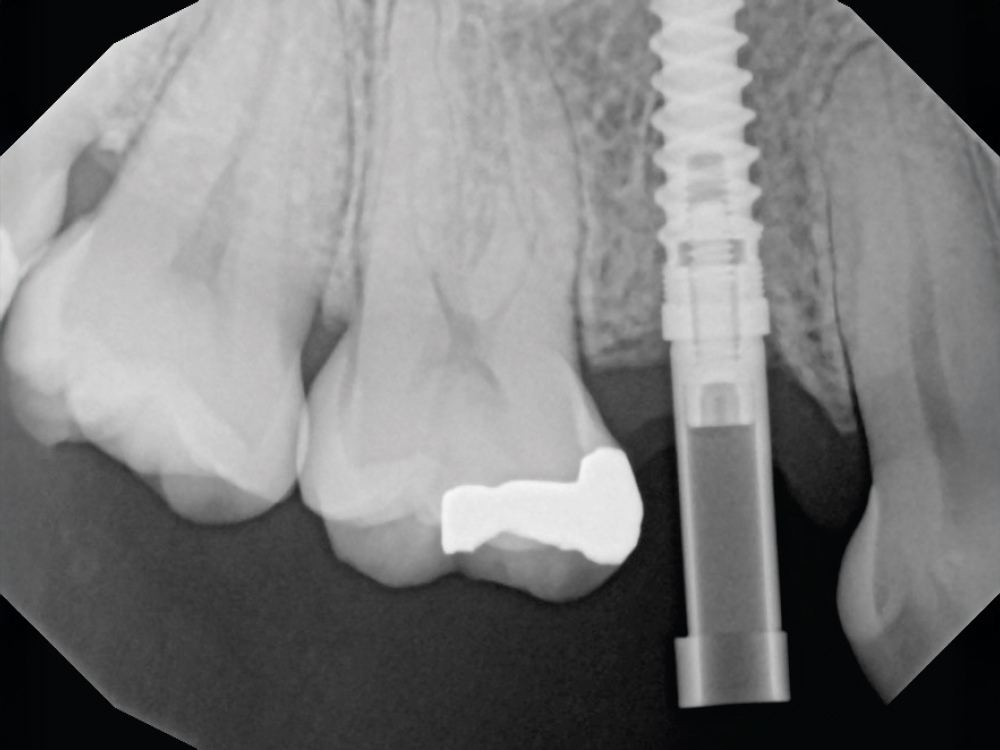
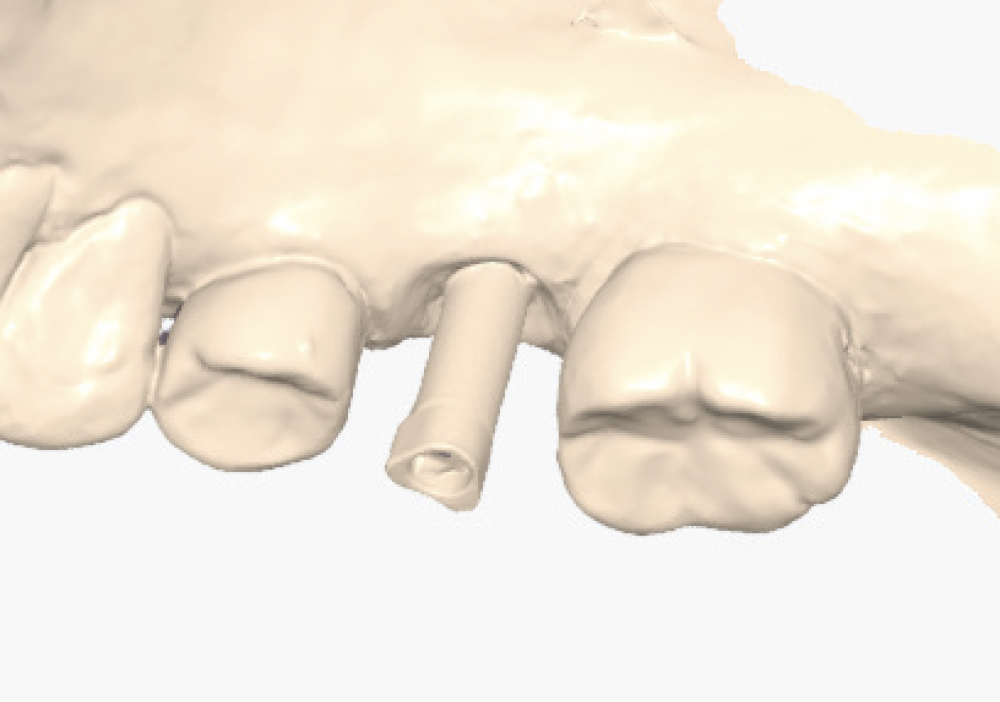
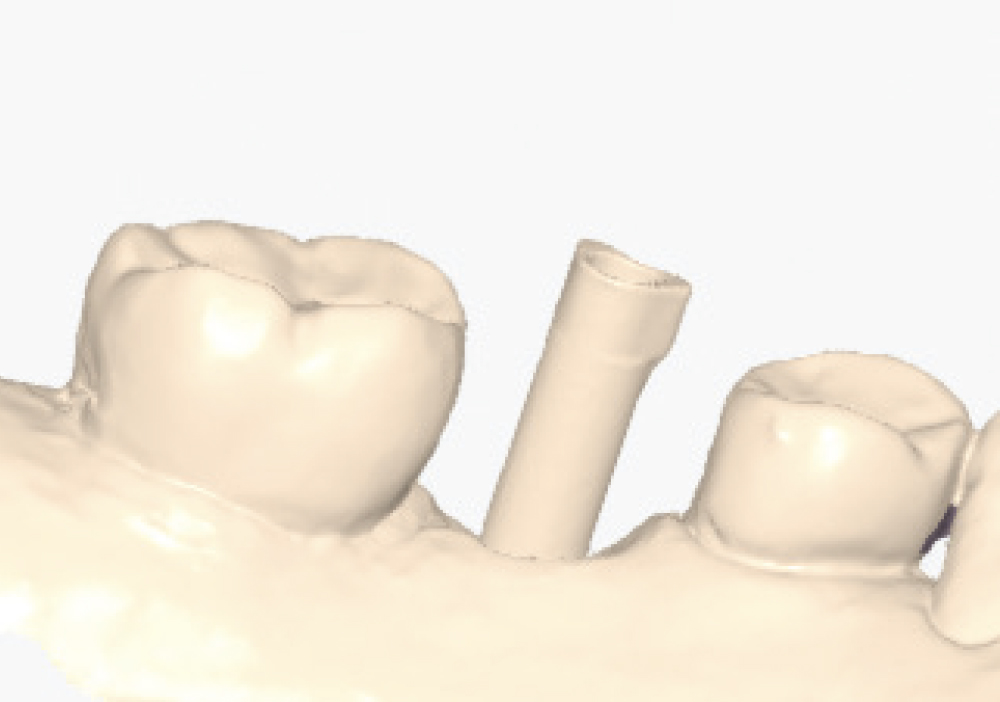
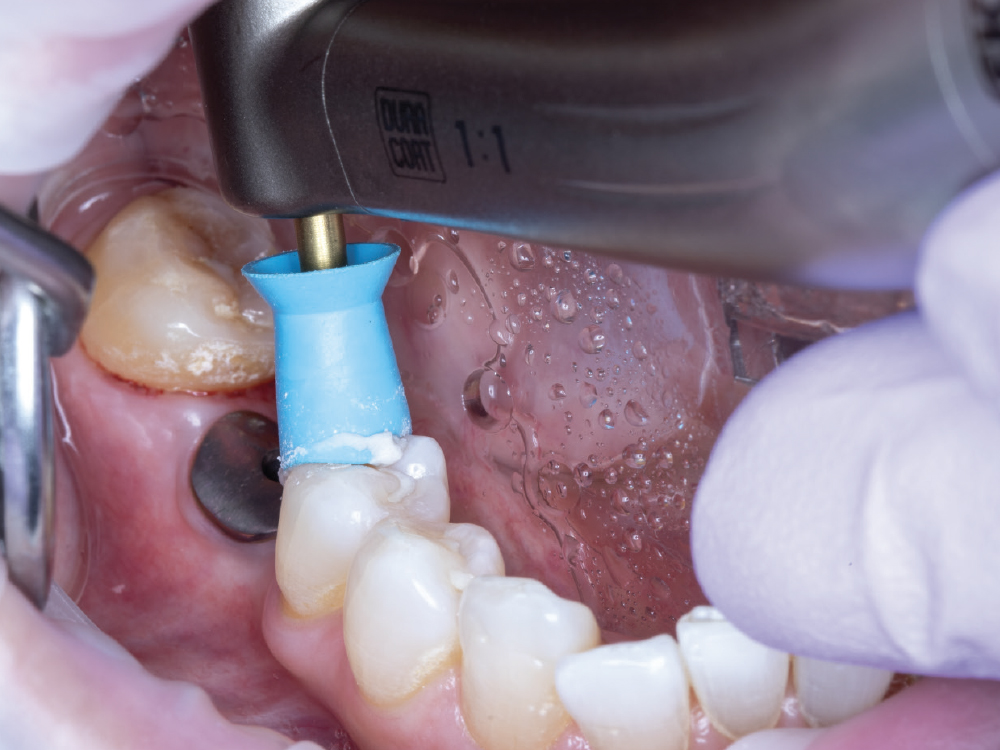
Verify Complete Scan Body Seating. Confirm the scan body is fully seated to the implant before scanning — how it seats is precisely how the final restoration will seat. Use a radiograph if there is any question about complete seating, as an incompletely seated scan body will result in a restoration that does not fit, regardless of scan quality. Apply firm finger pressure or use a seating instrument, then verify there is no rocking or movement. Check for any tissue interference preventing complete seating and address it before scanning.
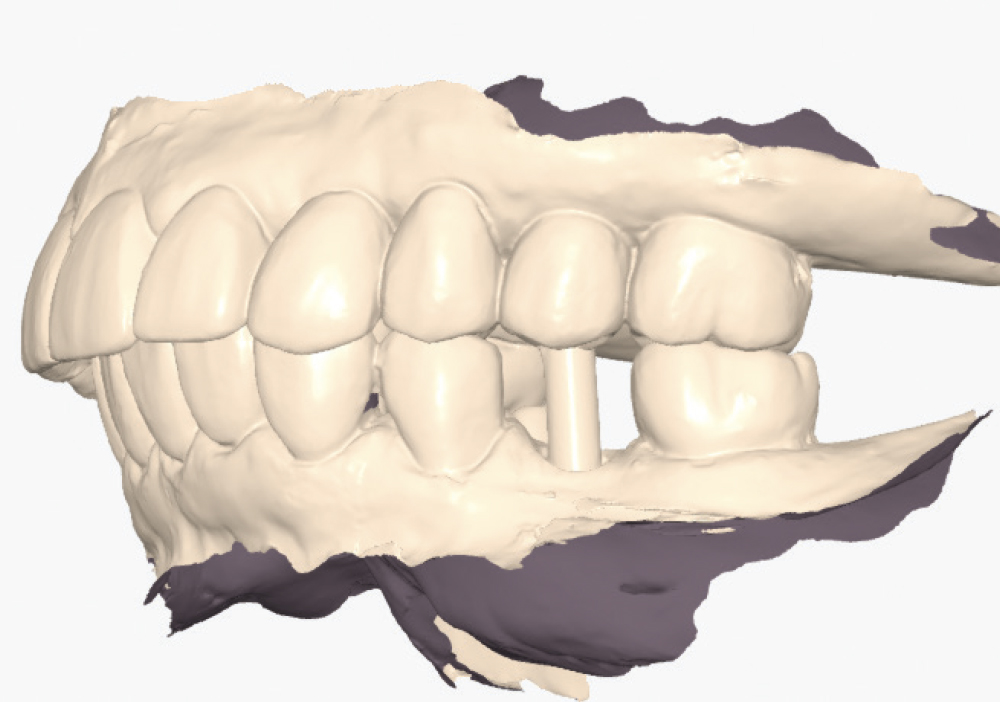
Capture Adjacent Contacts Strategically. For easily accessible sites, scan with the scan body in place to capture all relationships simultaneously. For difficult-to-reach posterior sites or tight interproximal spaces, consider capturing contacts with the healing abutment in place first. The healing abutment provides easier scanner access to critical interproximal and occlusal contact areas, and this two-stage approach ensures you do not sacrifice contact accuracy for scan body visibility. Document both scans and verify that contact relationships are clearly defined.
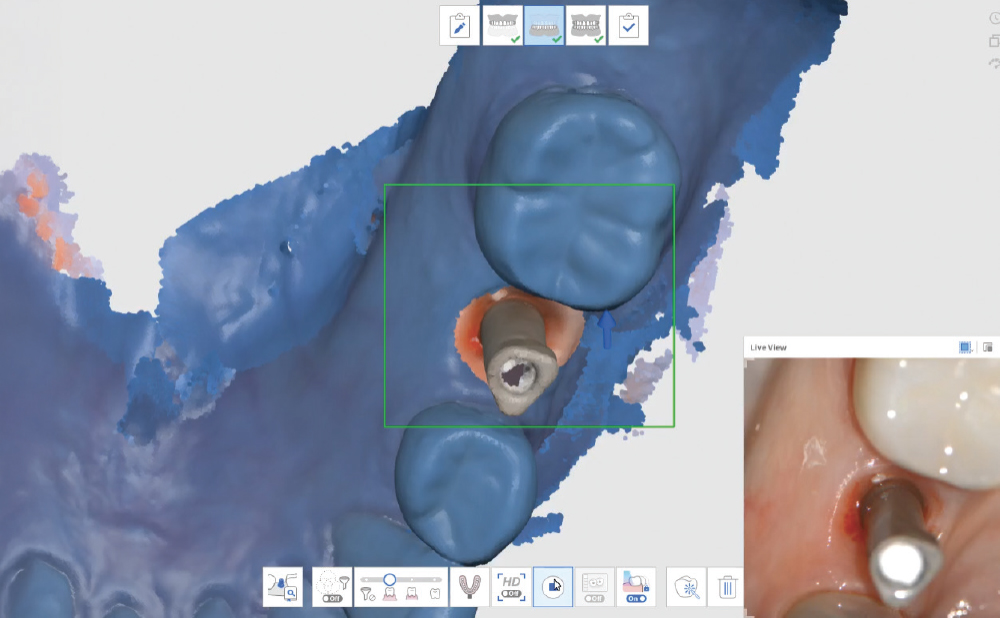
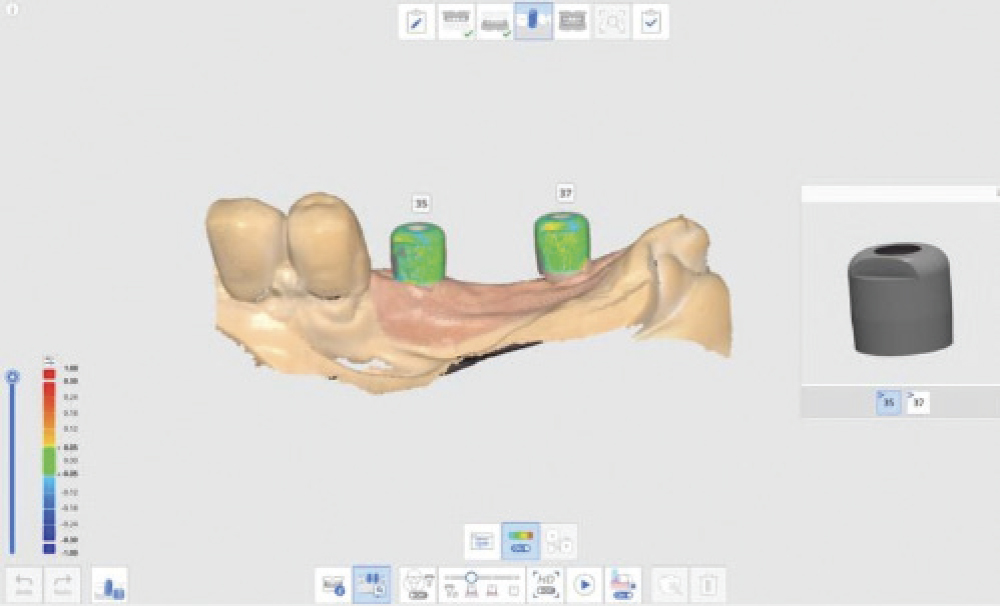
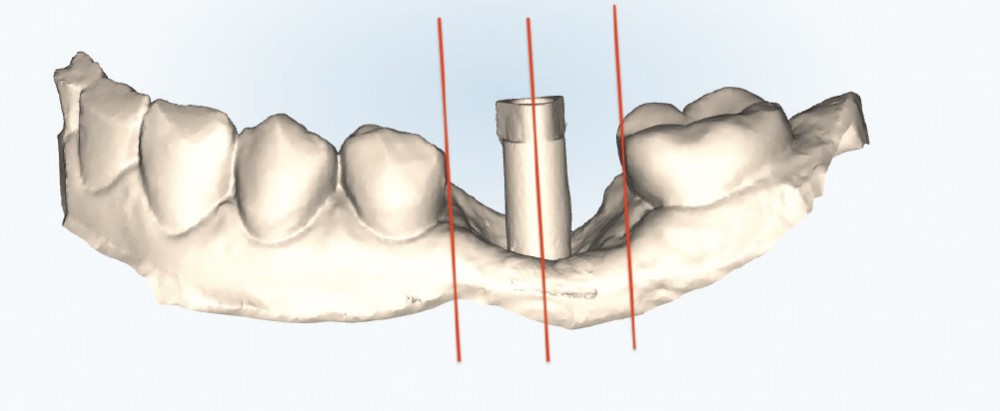
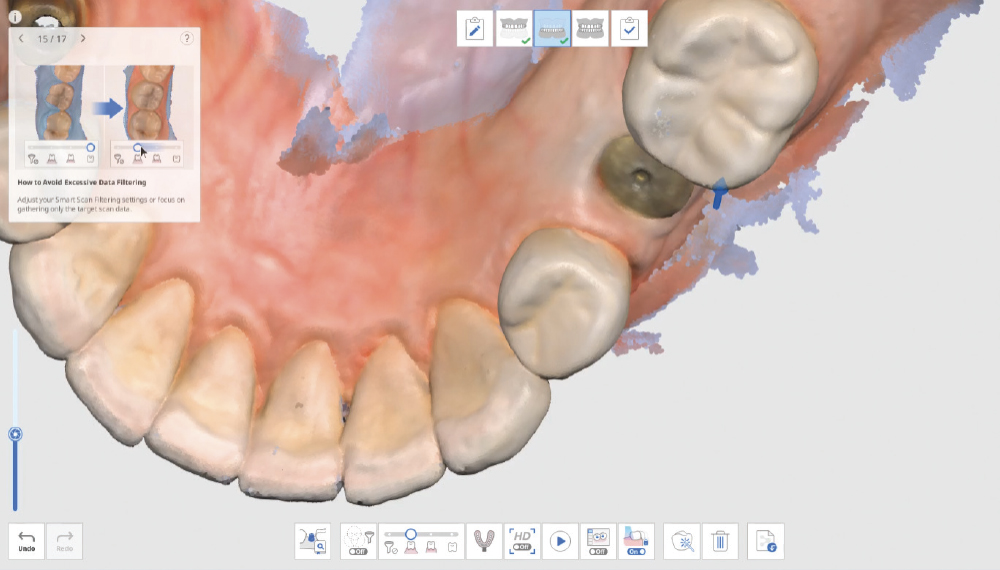
Thoroughly Scan the Scan Body Geometry. Complete, high-resolution capture of the scan body is non-negotiable. This is how laboratory software determines the precise three-dimensional position and angulation of the implant. The software matches the scanned scan body with its library file to establish the implant location in space. Scan from multiple angles to ensure all identifying features and surfaces are captured, as incomplete scan body data leads to misaligned restorations regardless of how perfect the rest of the scan appears. Verify that all reference markers, grooves, or geometric features are clearly visible in the acquired scan.
KEEP AN EYE ON AI
AI-assisted technology is a feature available with some chairside technologies to automatically detect and capture scan body geometry, which can significantly speed up the scanning process and improve accuracy. However, it’s crucial to understand how your scanner merges this AI-captured scan body data with the rest of your acquired scan, as various systems handle this integration differently and may have specific requirements or limitations. Before utilizing an AI feature on your scanner, contact your laboratory to confirm that you’re capturing all the necessary information in a format they can properly process, ensuring seamless case workflow and avoiding potential remakes.
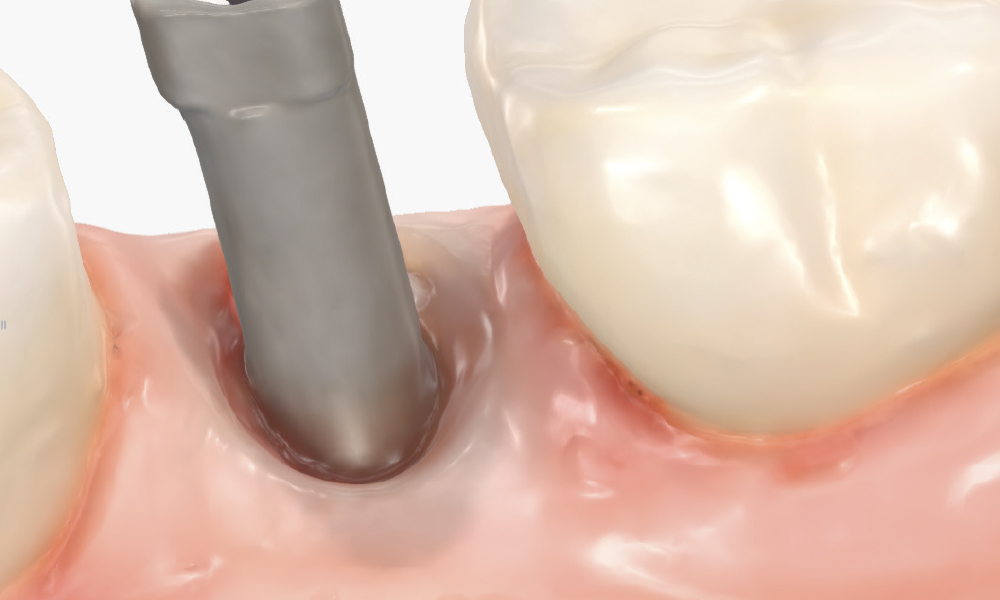
Capture the Surrounding Soft Tissue Immediately. Scan the peri-implant soft-tissue architecture as soon as the scan body is placed, before the tissue collapse occurs. Gingival tissues begin to collapse and distort within minutes of scan body insertion, and the initial tissue contours are critical for creating proper emergence profiles. Work efficiently but thoroughly to document the tissue topography in its most accurate state.
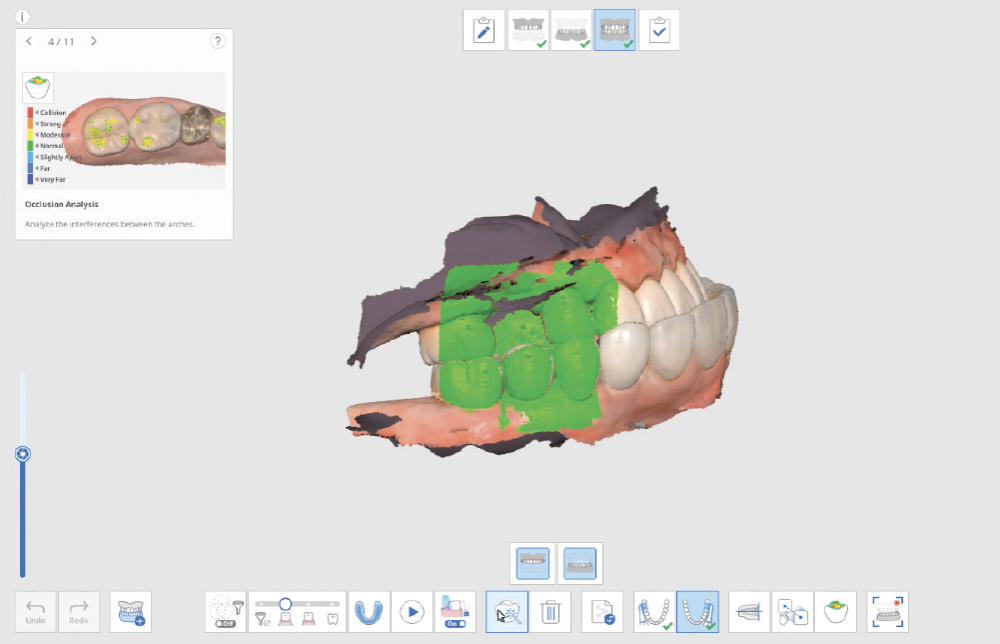
Capture Interocclusal Registration Without the Scan Body. Remove the scan body before capturing the bite registration, as it alters the occlusal relationship and can create an artificial bite record. The bite registration should reflect the patient’s natural occlusal condition, without interference from implant hardware, to ensure accurate articulation in the digital workflow. Capture the bite in maximum intercuspation with stable, reproducible contact.
Verify the Scans Before Dismissing the Patient. Review all critical areas while the patient is still in the chair, ensuring complete scan body capture, accurate contacts, adequate tissue detail, and proper bite registration. Zoom in on critical areas to verify resolution and completeness. It takes only two minutes to verify a scan, but potentially days before a patient is able to return to your practice. Use the scanner’s analysis tools to identify distortions or artifacts.
Don’t Trust Your Scan Without Verification. Screen visualization during scanning does not guarantee complete data capture, and small gaps, artifacts, or distortions may not be evident during active scanning. Discovering scan deficiencies after the patient leaves wastes everyone’s time. Make verification a non-negotiable final step at every scanning appointment.
Don’t Assume All Scanners Work the Same Way. Each scanning system has unique optimal techniques and workflows, and what works perfectly on one platform may be suboptimal on another. Stay current with your specific scanner’s software updates and technique recommendations by attending manufacturer training and user group forums to learn evolving best practices.
Don’t Send Questionable Scans to the Laboratory. If there are doubts about scan quality, address them before submission. Laboratories can only work with the data provided — they cannot fabricate accuracy that was not captured. Communication with the lab technician about scan concerns prevents delays and frustration, and a five-minute rescan is always faster than a remake.
RX SUBMISSION
When submitting a digital implant case to the lab, always send a complete lab prescription that includes essential implant information:
- Implant manufacturer/system name
- Platform size and diameter
- Desired restoration type (such as a screw-retained crown, cement-retained crown, or custom abutment with crown)
- Shade selection to ensure the final restoration matches the patient’s natural dentition
Providing this complete information upfront prevents delays, reduces the need for follow-up calls, and ensures the lab can fabricate the correct components for your case.
THE PATH FORWARD
Digital scanning technology continues to evolve. However, the fundamental principle remains constant: The quality of the digital impression directly determines the quality of the final restoration. Mastering these do’s and don’ts means that, regardless of the intraoral scanner used, the results will be predictable.
Practice and Ask Questions. Excellence in digital scanning is not achieved through technology alone — it requires good training, clear communication and deliberate practice. While there will always be some learning curves and occasional challenges, having a strong working rapport with your laboratory team and establishing clear protocols helps you navigate setbacks with confidence.
CONCLUSION
The real potential of digital scanning lies in consistency. Single-unit cases may seem straightforward, but they are often where small mistakes happen. By creating clear protocols within your practice and empowering your team with proper training, you can avoid common pitfalls and produce digital implant scans that translate into successful restorations.