Digital Implant Workflow: From Surgical Plan to Final Crown (1 CEU)
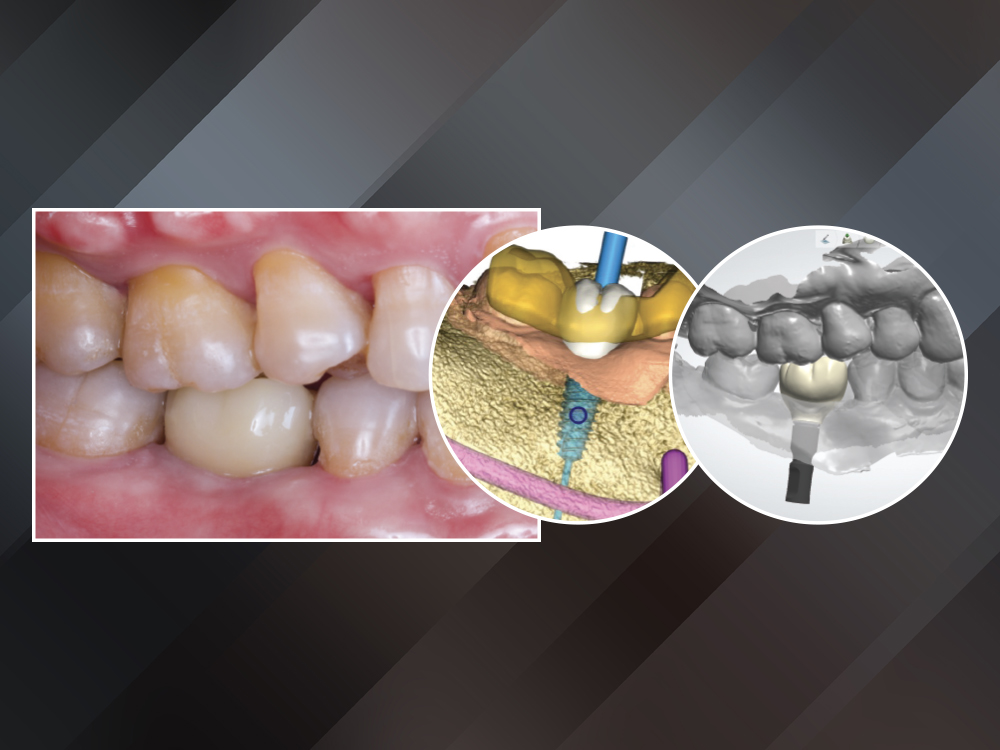
Ted Vo, a dental technician in the Glidewell implant department, came to our clinic because he had been missing tooth #30 for several years. He reported difficulty eating and was self-conscious about the edentulous space that sometimes showed when talking and laughing. Except for an occlusal amalgam restoration on #31, the adjacent teeth were healthy. My treatment plan called for an implant and a BruxZir® Esthetic Zirconia screw-retained crown, which the patient accepted.
CASE REPORT
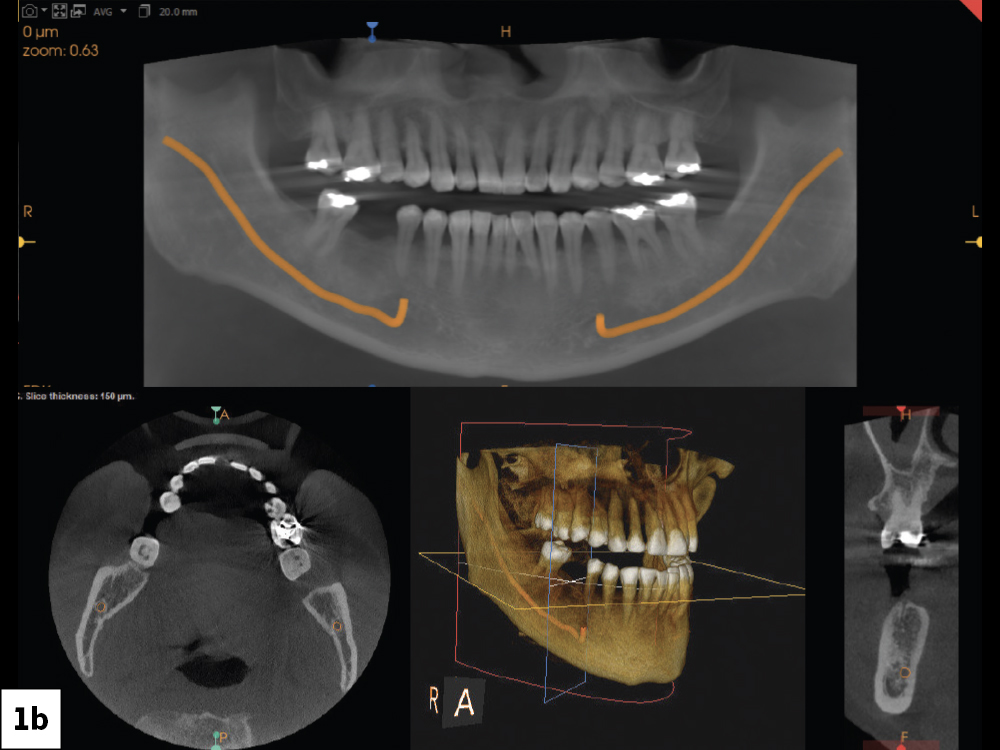
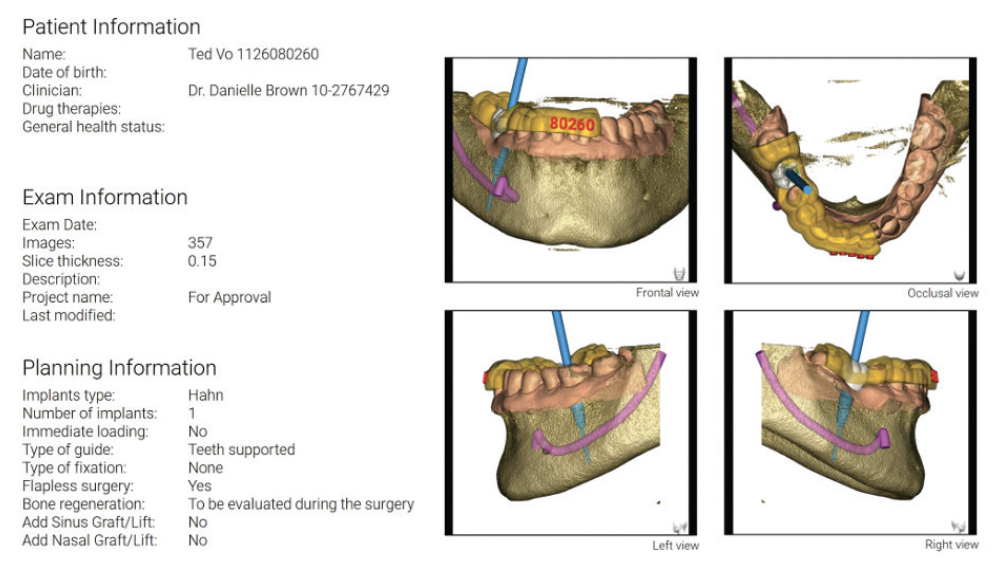
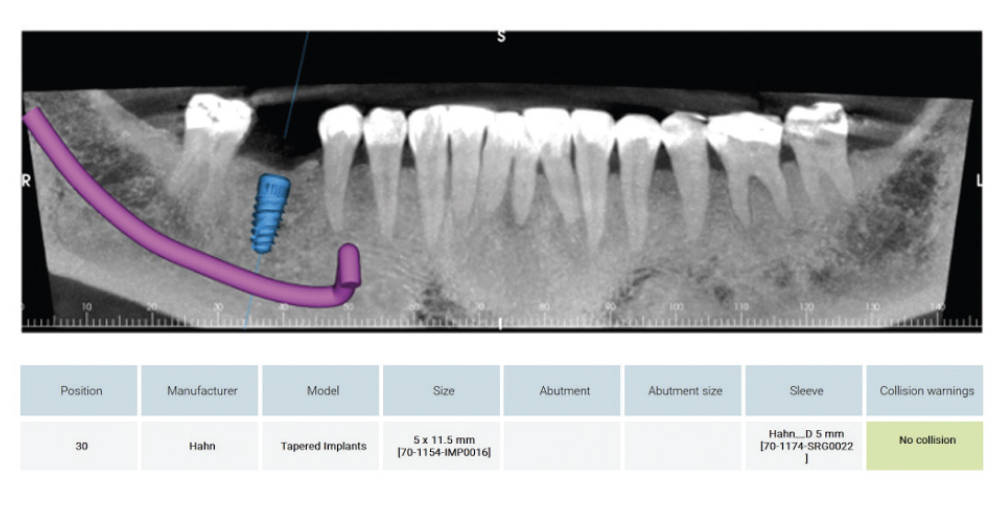
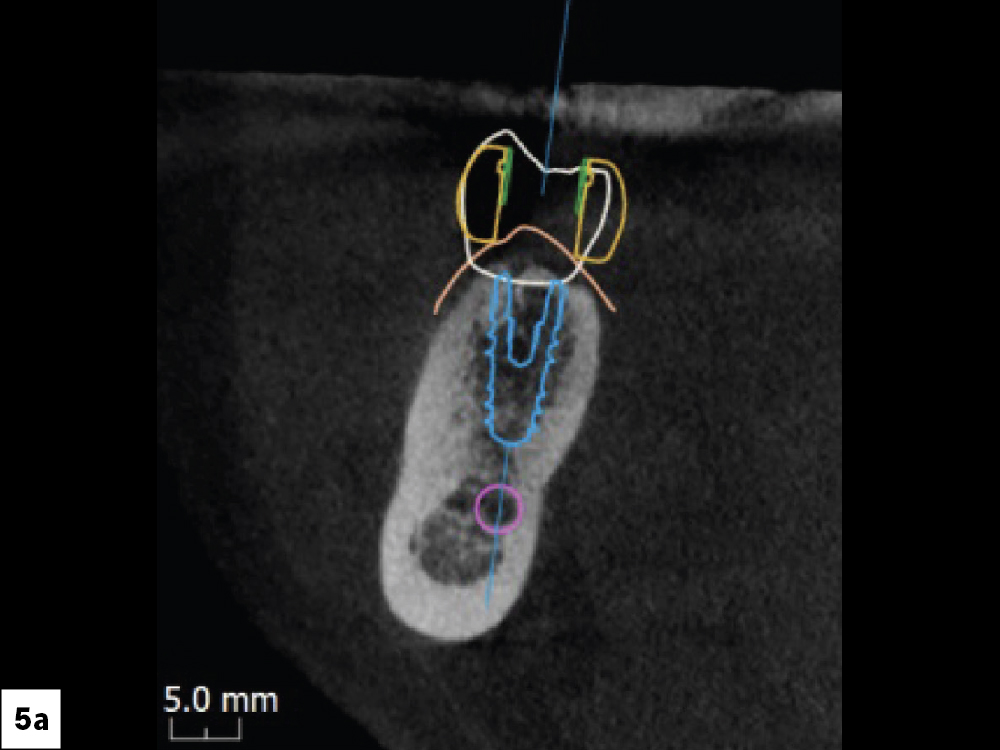
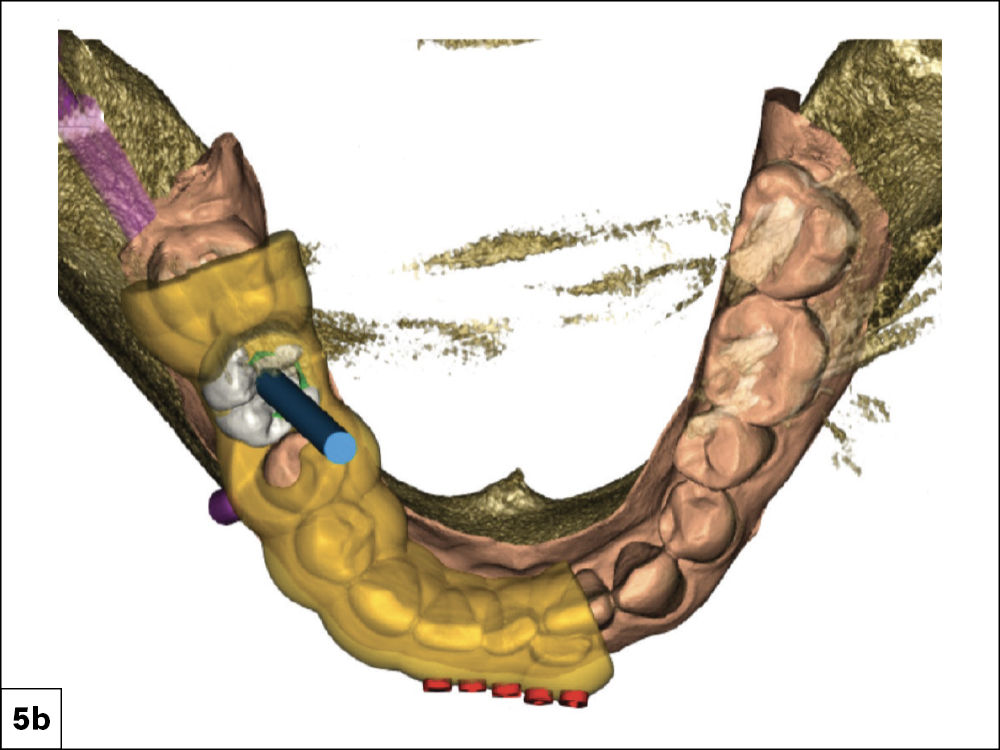
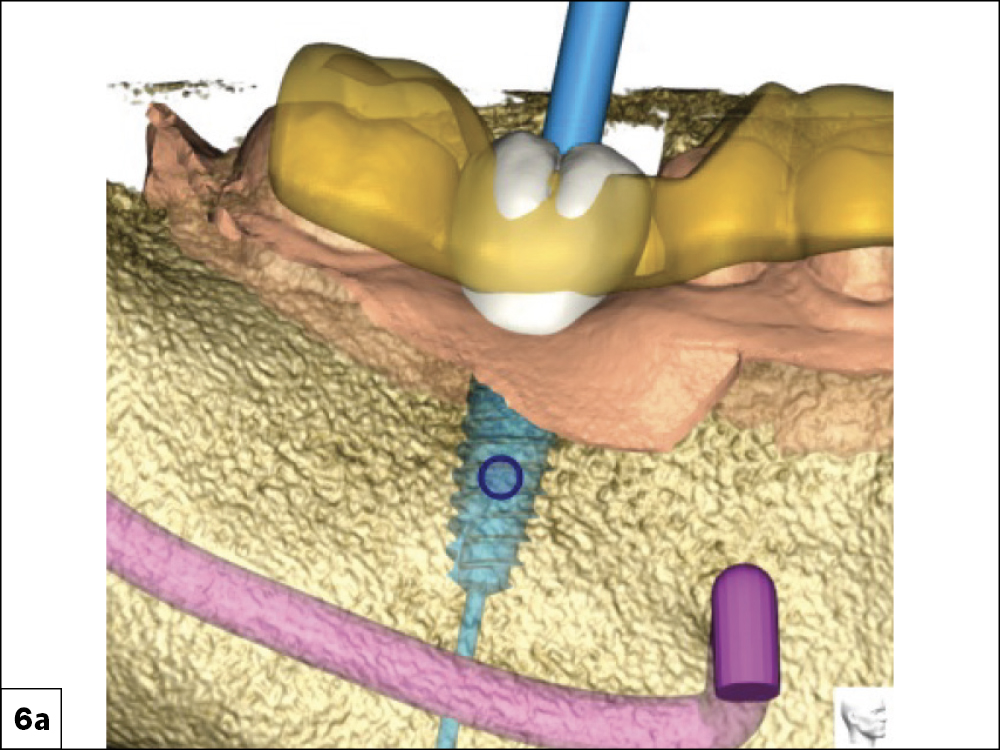
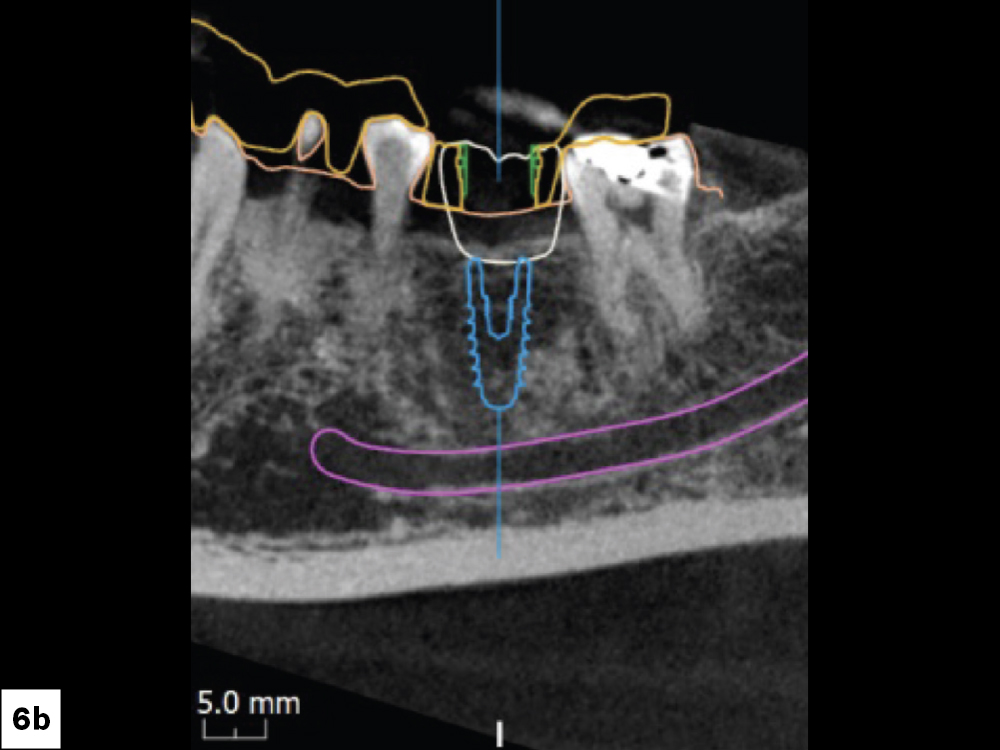
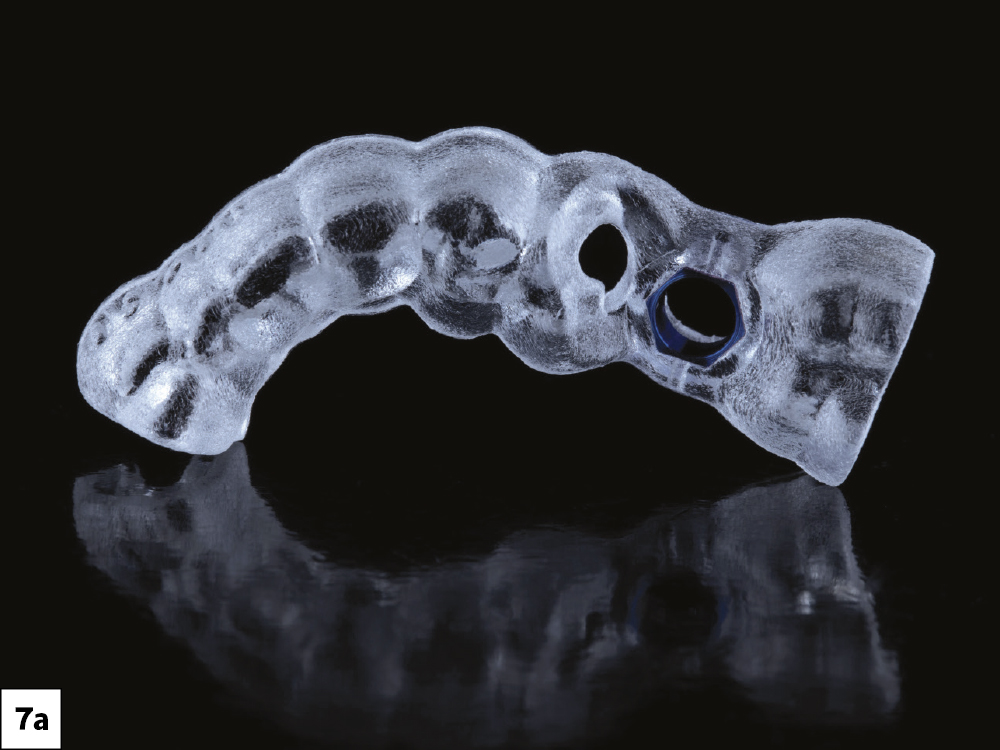
IMPLANT PLANNING (Appointment 1)
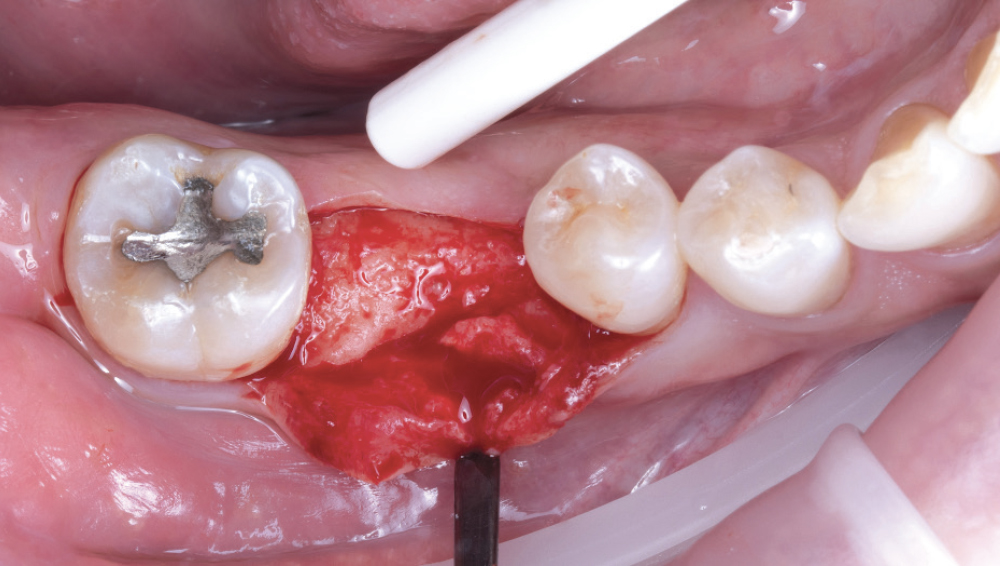
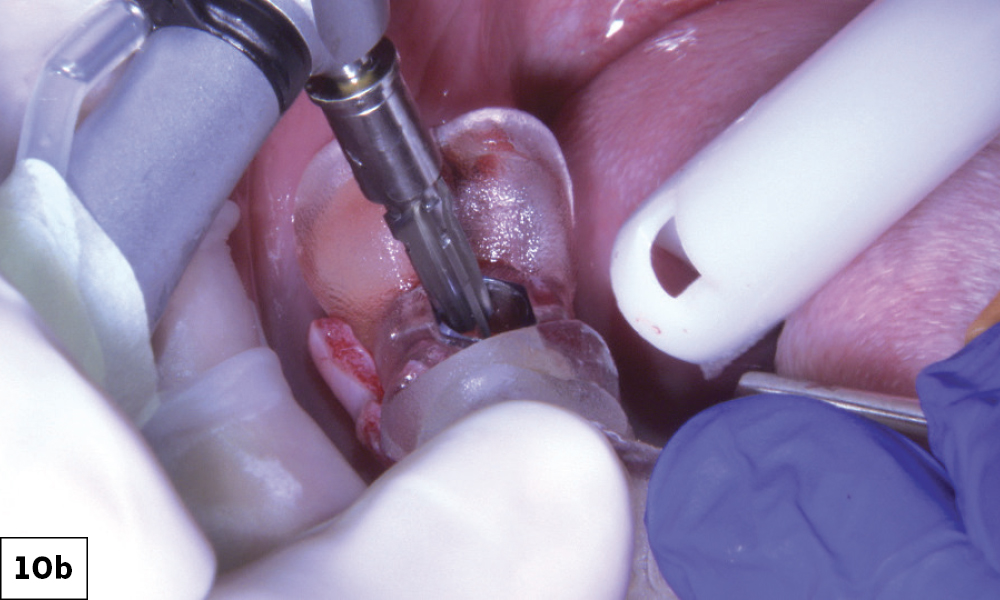
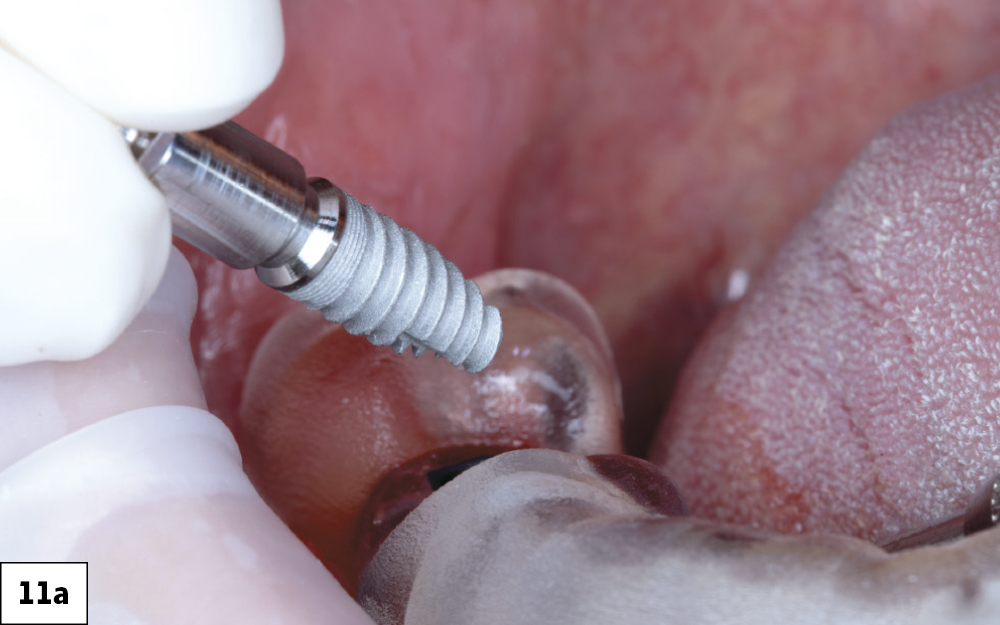
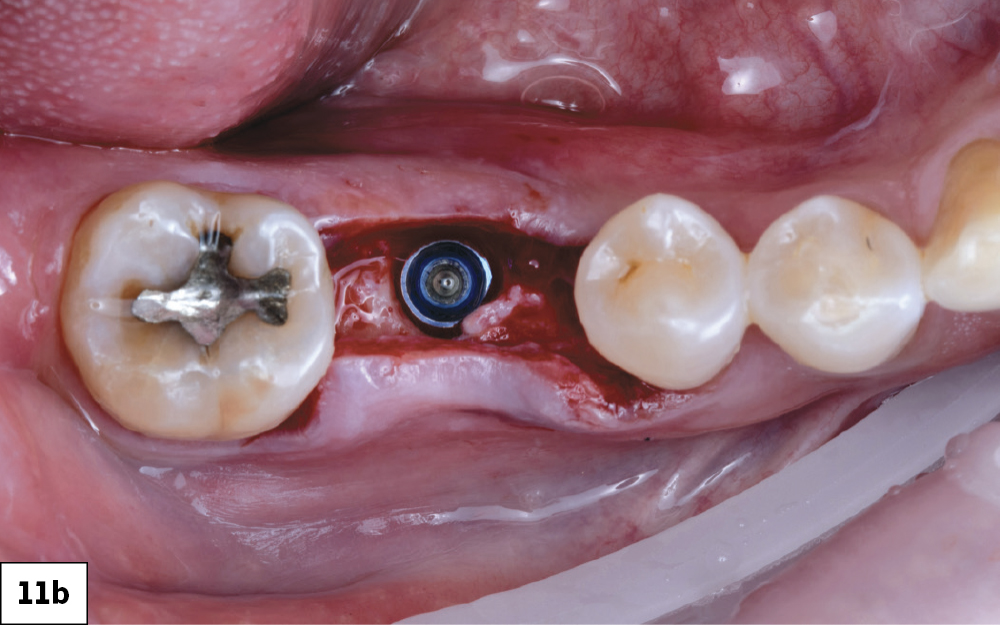
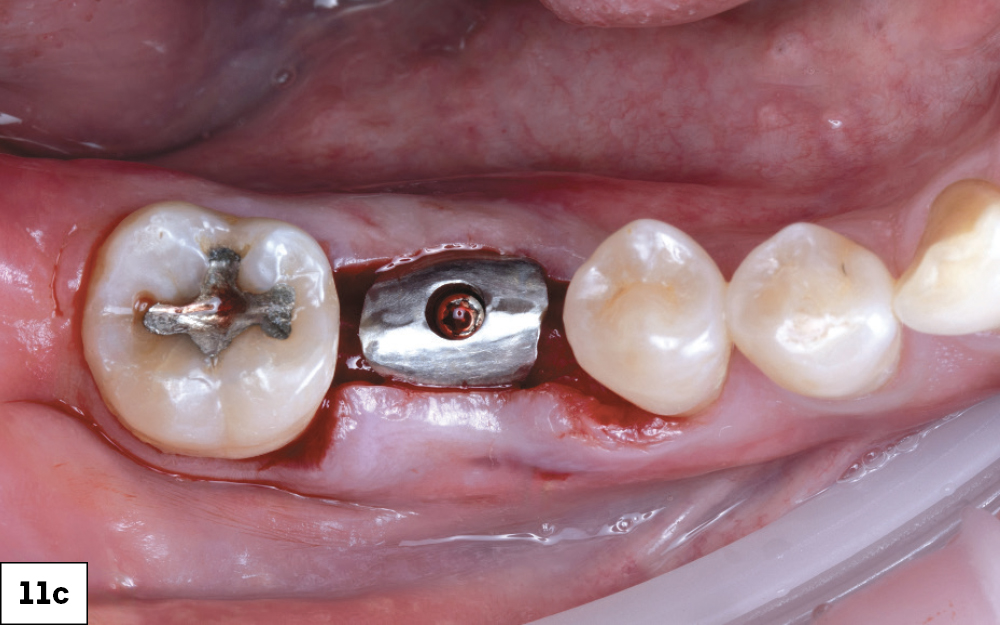
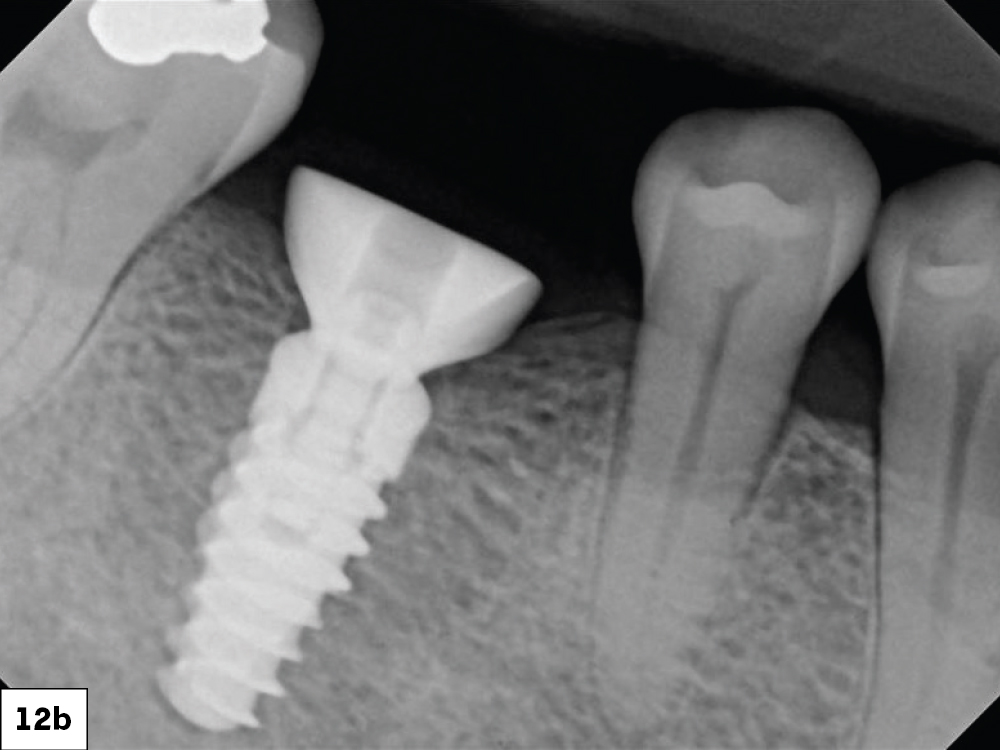
SURGERY DAY (Appointment 2)
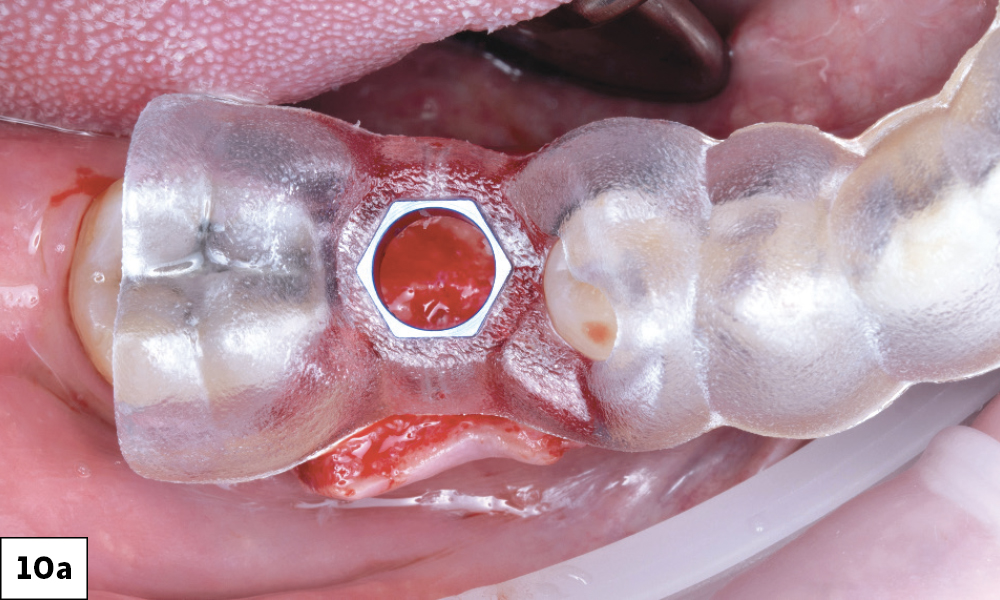
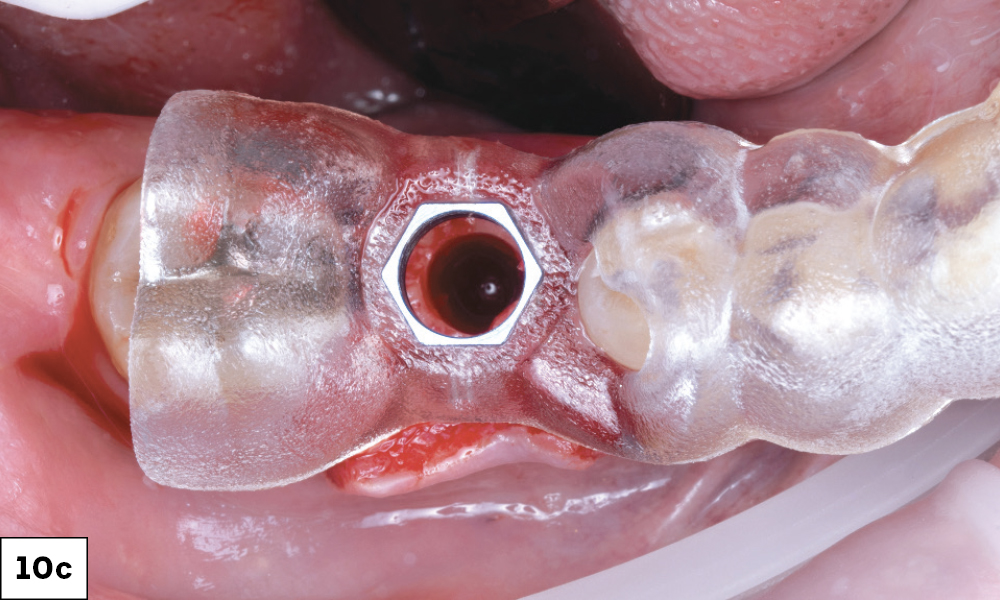
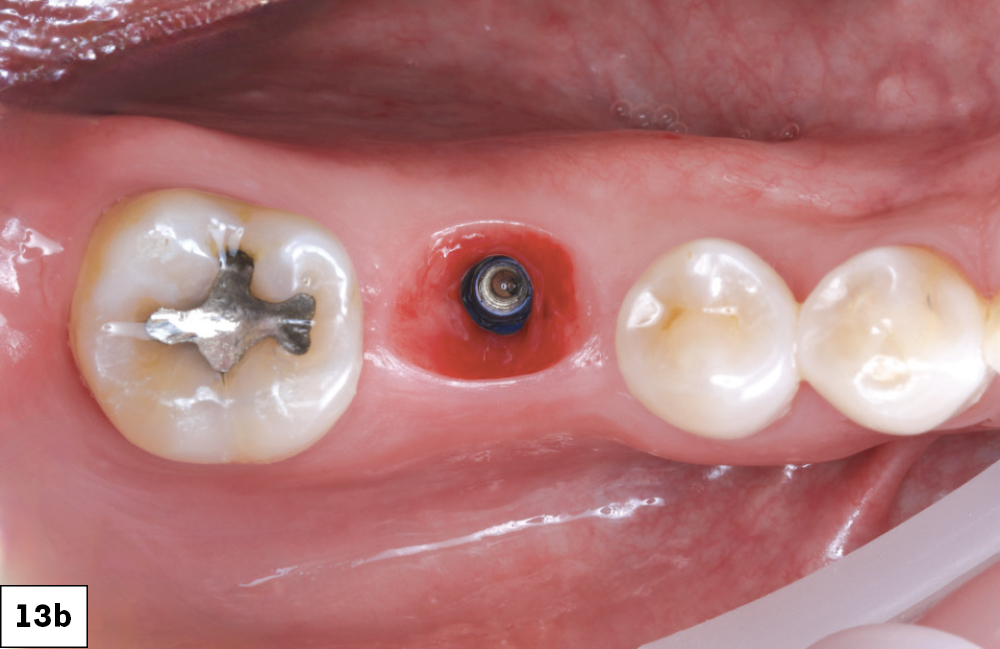
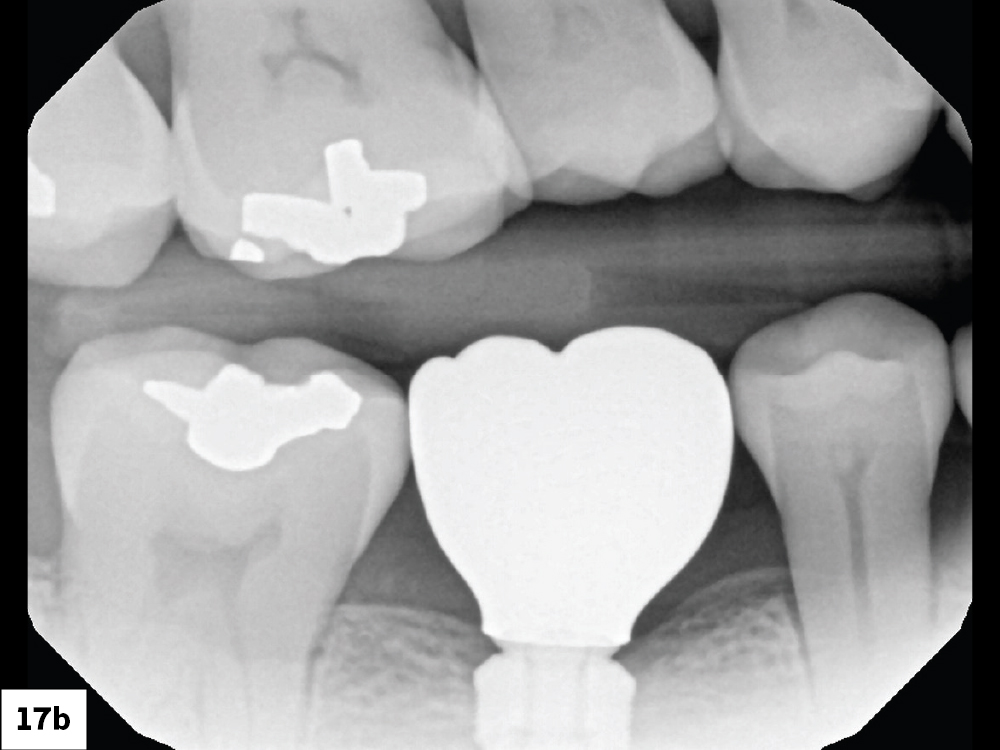
FOUR-MONTH FOLLOW-UP (Appointment 3)
The patient returned four months after implant placement to begin the prosthetic phase of the process.
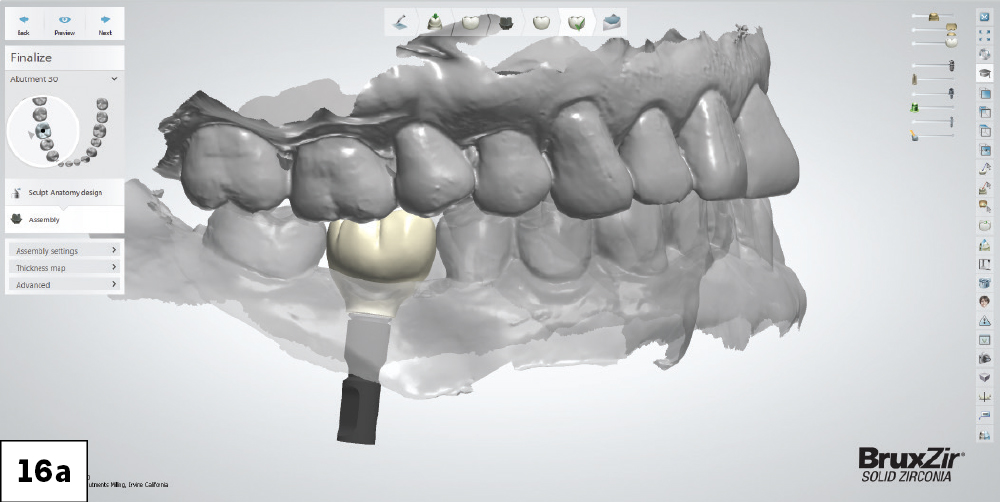
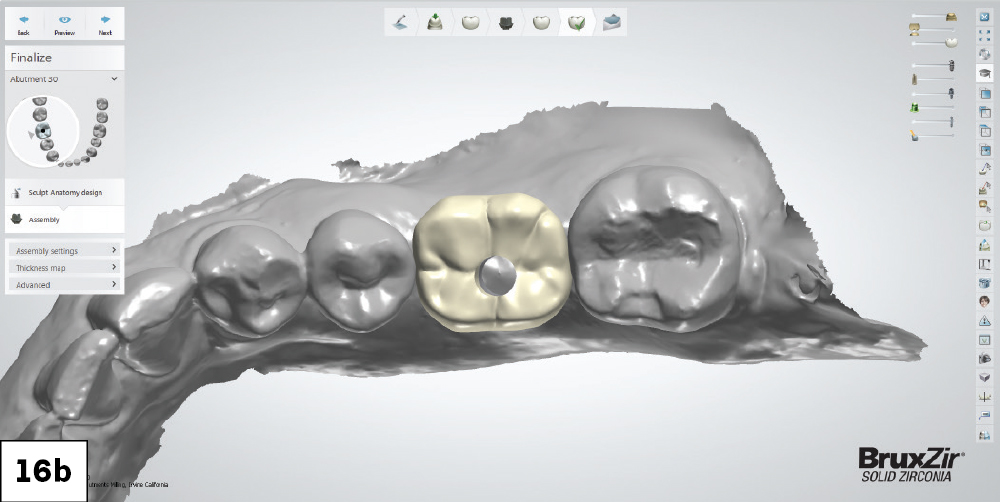
DEFINITIVE RESTORATION AND OUTCOME (Appointment 4)
(We allowed two weeks between impression and delivery)
CONCLUSION
More streamlined surgical and restorative workflows, including the use of custom components in the Glidewell Tooth Replacement Solution, means more precision, convenience, and long-term success for these essential procedures. The selection of a BruxZir Esthetic screw-retained crown helped deliver a permanent, functional, esthetic result that the patient was extremely happy to receive.
Biotex is a trademark of Citagenix, Inc. Penguin RFA is a registered trademark of Integration Diagnostics Sweden AB.