Complete Dentures: Troubleshooting Common Complaints

Whether you are delivering a complete denture to a first-time wearer or — even more challenging — fabricating a new prosthesis for a longtime edentulous patient, you are likely to experience patient complaints about sore spots, dislodging of the denture, and speech impairment. For the most part, such concerns can be addressed with just a little investigation and some simple adjustments. In this article, I will explain the methods I use to determine the cause of three common complaints, as well as where to make needed adjustments and which materials to use.
I’ll start with a simple caveat: We should never make any adjustments to a patient’s denture until we’ve determined the root cause of the issue. Making adjustments prematurely could compromise the overall fit and permanently damage the denture itself. Now, on to more specific trouble spots.
PATIENT CONCERN NO. 1: INSTABILITY DUE TO POOR FIT OR UNSATISFACTORY SEAL
It’s important with this particular complaint to ask the patient when these issues occur. Here are some of the most common answers:
During Initial Placement: This issue can be caused by a number of factors, foremost of which is overextended borders. Direct visualization can help identify overextended borders. If you are unable to identify the overextended areas, place disclosing wax along the borders of the prosthesis and have the patient perform the border-molding motions.
If the vestibular borders are acceptable, I will then check the posterior palatal seal (PPS). If the vestibular borders are acceptable but the PPS is overbulked or overextended, the denture may dislodge or cause discomfort. To check this, I have the patient say “Ahh” several times to help determine where the posterior extent of the denture should be and adjust accordingly. To evaluate if the posterior seal was overbulked, I reevaluate the posterior palate using a T-ball burnisher or a mirror to check how depressible the soft tissue is. Pressure-indicating paste placed on the intaglio surface of the denture can help identify the area where the posterior seal is over-bulked.
Another common cause of a poor maxillary denture fit is a prominent median palatine suture. In some cases, especially if a very light-viscosity VPS impression material was used, the denture may have too much extension into the suture, which can prevent adequate settling of the denture. Check this area carefully with pressure-indicating paste, and adjust accordingly.
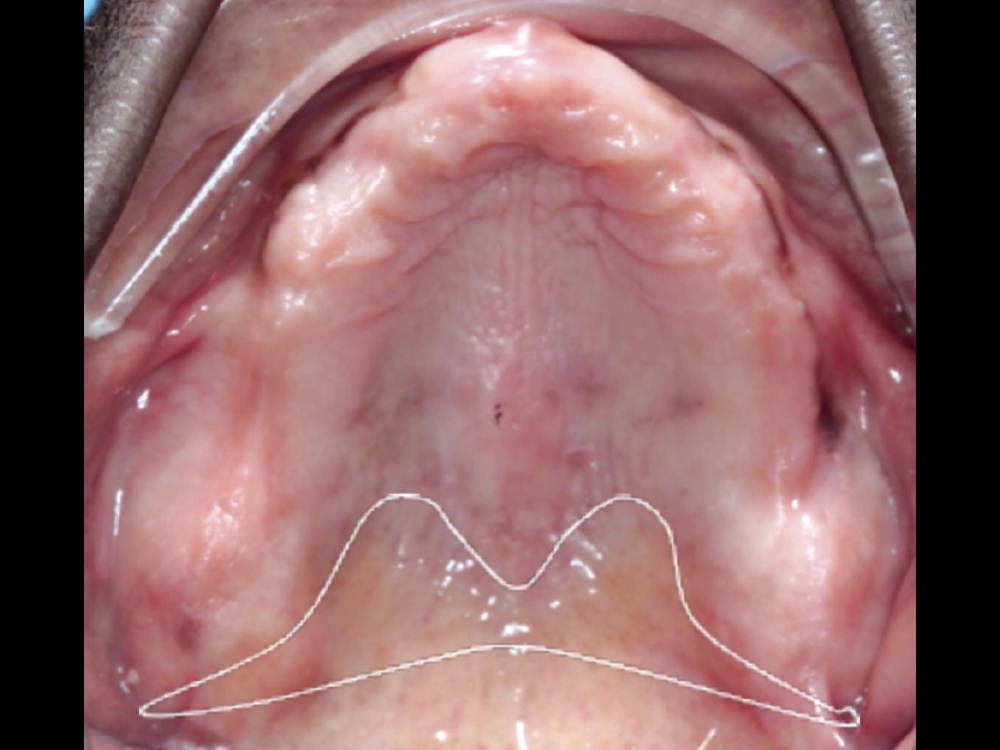
Outlined in white, the posterior palatal seal is an area that must be evaluated if a patient is having trouble with their denture staying in place.
If the denture extends too far into the median palatine suture (shown here in white), a poor fit can result. This can be checked with pressure-indicating paste and adjusted if needed.
When Chewing: Denture movement during chewing is frequently caused by: 1) overextension, especially in frenal attachment areas; 2) an over-bulked buccal flange; 3) incorrect tooth positioning; and 4) improper chewing habits.
In order to evaluate overextension in the frenal areas, I will often place the maxillary denture in the patient’s mouth, hold it up with one finger on the mid-palate area, and use my other hand to gently pull the cheek directly laterally. If the denture is overextended, the denture will drop immediately. Sometimes this is even better at showing overextensions than repeating border-molding motions.
An over-bulked maxillary buccal flange can interfere with chewing because, as the patient’s mandible moves left and right, the coronoid process can come into contact with the denture. Test this by placing the denture and having the patient move their jaw left and right. If this area is over-bulked, either the patient will feel as though they don’t have enough room to move their jaw, or the denture will dislodge.
Improper tooth positioning can also cause denture dislodgement during chewing. This is a harder issue to correct as it may require resetting the teeth. Thus, it’s important to keep this in mind during your try-in appointments. If the plane of occlusion is too high or too low compared to the tongue, the food bolus is unable to reach an area where it can be chewed. This results in patients moving their tongue in extreme motions to move the bolus to the chewing surface, causing dislodgement.
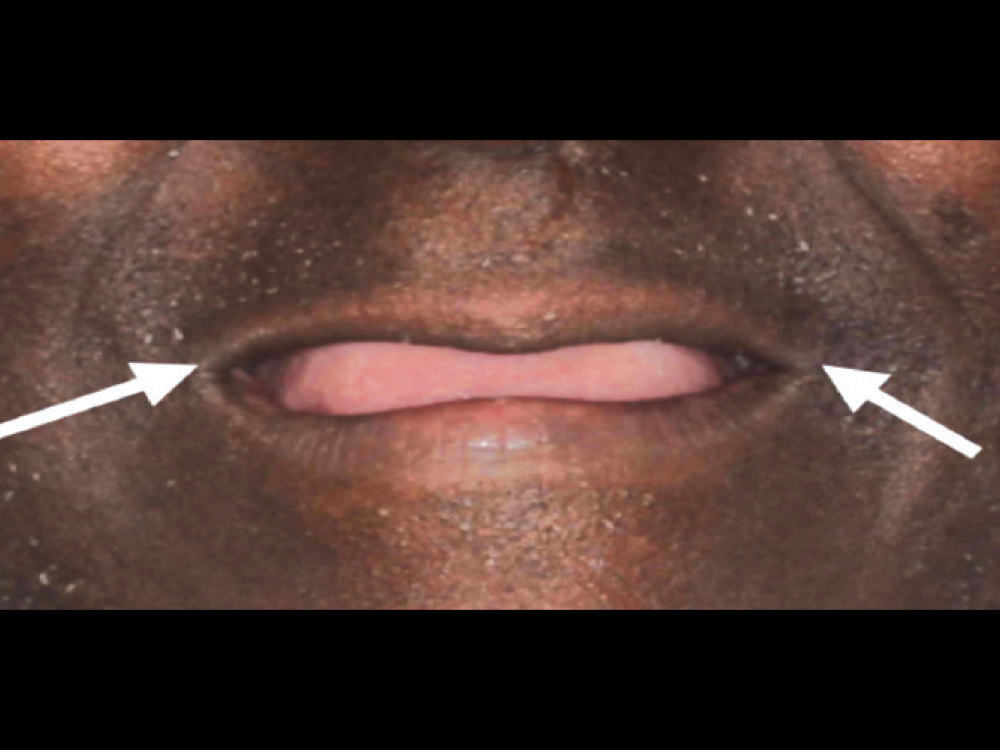
Use the commissures of the lips as your guide for occlusal plane level. It often will match up with the height of the tongue.
If the patient is new to wearing a denture, patient education and encouragement may be needed. Instruct the patient to split the food bolus in two and chew with both sides. This can help to stabilize the denture during the chewing process. It’s a good practice to encourage your patients to start with soft foods and move toward harder or chewier foods as they gain more confidence with their new prostheses.
When Occluding: Denture instability can result from malocclusion, such as: 1) premature contacts; and 2) when the maximum intercuspation is not in harmony with the patient’s centric relation. Initially, check the denture for even bilateral contacts using a horseshoe-shaped articulating paper. If an area is still bothering the patient, a thinner articulating paper such as AccuFilm® (Parkell; Edgewood, N.Y.) can be used to more accurately identify the high spot. If the patient’s bite is not repeatable, it may be necessary to perform a clinical remount and return the denture to the lab to adjust or reset the occlusion.
PATIENT CONCERN NO. 2: SORE SPOTS
The good news about areas of discomfort caused by the patient’s denture is that the source can be readily determined based on the location of the sore spots. In most cases, the situation is easily remedied.
Vestibule: Sores in the vestibular area are frequently caused by overextended borders or rough spots in the base. Identifying the overextended areas with disclosing wax and shortening those border areas of the denture are often all that’s necessary to alleviate the cause of the sores.
Posterior Palatal Seal: A sore spot in the area of the PPS can be caused by a sharp edge, or if the PPS is too deep or overextended. Run a gloved finger along the edges to see if there are any sharp or jagged spots. If you can feel it through your glove, the sharp or rough edge should be rounded or smoothed. If the PPS is too deep, pressure-indicating paste can be used to identify over-bulked areas. If the denture is overextended toward the throat, the patient may complain of a sore throat. Visualize the transition between the movable and immovable tissues by having the patient say “Ahh.” The denture should not extend past this point.

Example of inflammation from fungal infection where a partial denture contacts the oral mucosa. Encourage the patient to avoid this by removing the denture each night and using a denture cleanser. Treatment may require a nystatin prescription.


Once the cause of the sore spot is identified, the denture is adjusted and polished to eliminate the problem.
Single Areas on the Ridge: There are several potential causes for single sore spots on the crest of the ridge, primarily premature occlusion or the presence of nodules or voids in the denture base. The former can be solved by checking occlusion as recommended previously. A clinical remount of the dentures may be needed for patients who have a hard time finding a repeatable occluding position. Nodules on the intaglio surface can be felt with a gloved finger and gently removed with an acrylic bur. Small voids in the denture base can be carefully filled with a chairside hard-reline material.
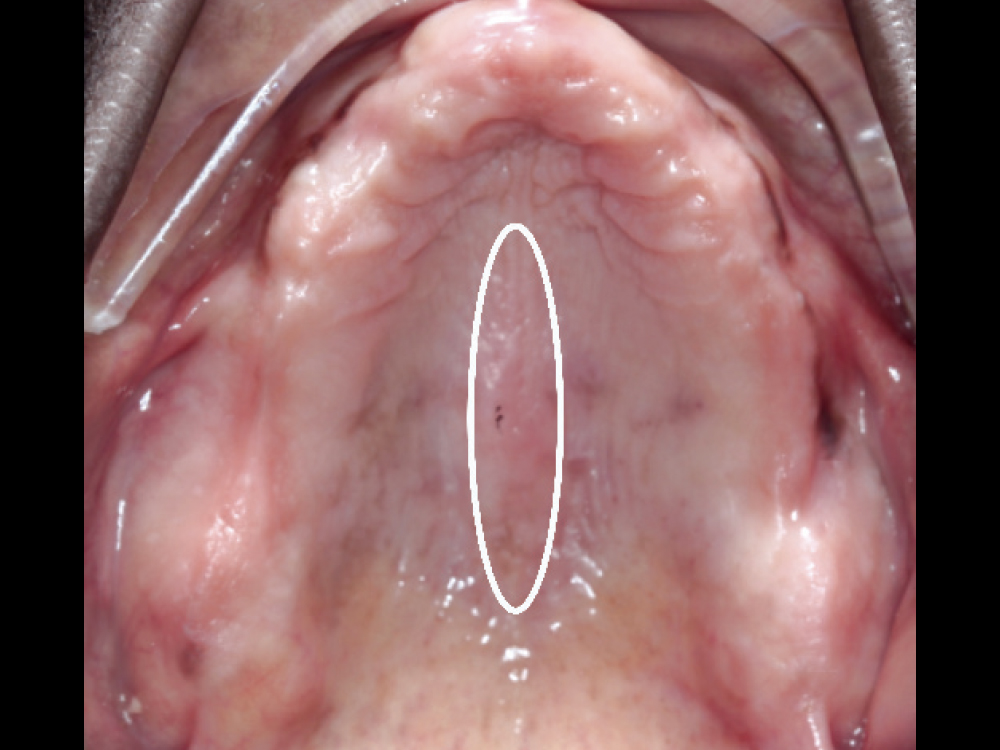
Overall Area of the Ridge: Generalized soreness on the ridge could be an indication that the vertical is open too much or that the tissue has overgrown due to papillary hyperplasia. First, reassess the vertical dimension of occlusion, evaluating the facial esthetics and phonetics. If the speaking space was violated, a remake of the denture is necessary to correct the vertical. When the soft tissue on the ridge shows signs of papillary hyperplasia, the cause is typically an ill-fitting denture base. In these cases, a tissue conditioner should be utilized to help the tissue rebound before proceeding to fabrication of a new prosthesis or hard-relining the current denture. If the patient has generalized redness, soreness and white patches that wipe off easily, it is usually due to an oral fungal infection. This can be prevented with proper denture hygiene, including removal and cleansing of the denture each night, and treated with antifungal medications.

A poorly fitted mandibular denture can lead to excess tissue growth known as epulis fissuratum, which can necessitate surgical correction. This can be prevented by routine adjustments and relines or fabrication of a new prosthesis when indicated.

Example of excessive vertical dimension of occlusion. When patients complain of generalized soreness along the ridge, the vertical dimension should be reassessed and, if necessary, the denture remade.
PATIENT CONCERN NO. 3: PHONETIC CONCERNS
Disruptions in phonetics are signs that alterations are necessary to improve the denture fit. Here are some of the most common phonetic concerns associated with dentures.
Whistle on “S” Sound: This issue is caused by the absence of sufficient space for the tongue between upper bicuspids. The solution is to remove and relocate the denture bicuspids toward the buccal or, if there is adequate room, grind out more area for the tongue. In some instances, the denture base is built up too thick. To determine which area requires adjustment, carefully place pressure-indicating paste palatal to the bicuspids. After checking the phonetics, remove material from the base in the area where the paste has been displaced.

If the patient whistles on an “S” sound during your phonetics check, remove material palatal to the bicuspids to free up some additional tongue space.
Lisping on “S” Sound: This concern is essentially the opposite of the whistling “S” in that its cause is too much room for the tongue between the upper bicuspids. To test for this, add a piece of wax palatal to the bicuspids and check phonetics. If successful, adding chairside acrylic to the denture base will help narrow that palatal space.

Indistinct “Th” and “T” sounds can be corrected by thinning out the palatal area of the anterior.
CONCLUSION
Clinicians providing complete dentures will inevitably encounter patient complaints about fit and function. Addressing these concerns typically involves identifying the cause of denture instability, sore spots or phonetic complications, and making the necessary alterations to the patient’s prosthesis. It is imperative that the clinician carefully determines the source of the issue prior to making any adjustments to prevent compromising the overall fit of the denture.