Medical Evaluation: Part 2 — Systemic Disease and Oral Implants

Systemic diseases play a vital role in treatment planning and implant therapy for patients. A wide spectrum of systemic diseases may directly affect bone metabolism, wound healing, and ultimately the success of dental implant or bone graft procedures. The implant clinician must develop a strong foundation for understanding the direct relationship between systemic diseases and the planning and management phases of dental treatment. In Part 2 of this medical evaluation article series, several systemic diseases that directly affect the success of dental implants will be discussed. To learn about the preoperative evaluation of the dental implant patient, read Part 1 of this series in Chairside® magazine Vol. 16, Iss. 1.
DIABETES MELLITUS
Diabetes mellitus is a chronic medical condition that is reaching epidemic proportions throughout the world. Diabetes occurs when the body’s ability to produce or respond to the hormone insulin is impaired, thereby increasing the concentration of glucose in the blood (hyperglycemia). Glycemic control is a primary consideration for dental implant therapy. Elevated levels of glucose have been associated with micro- and macrovascular complications that may result in increased tooth loss, periodontitis, bone graft failure, implant failure and peri-implant disease. Therefore, it is imperative that the implant clinician determines the glycemic control of diabetic patients prior to treatment.
The ideal test to determine glycemic control is the hemoglobin A1c (HbA1c, glycated Hb, A1c), which represents the percentage of non-enzymatically glycated A1c hemoglobin bound to red blood cells. Because red blood cells have an average circulating life span of 60–90 days, the HbA1c value depicts the patient’s control over a three-month period. This test is more accurate in the assessment of diabetic control compared with a fasting blood glucose, which can give a false-positive or false-negative result. Ideal HbA1c values for diabetics is 6% with glycemic control in the range of 6%–7%. An increased failure rate of dental implants has been associated with poor metabolic control.1
Dental Implant Implications: Relative or absolute contraindication
- HbA1c less than 6%: No contraindication
- HbA1c greater than 6% and less than or equal to 8%: Relative contraindication
- HbA1c greater than 8%: Absolute contraindication
Antibiotics: Because of the high correlation between hyperglycemia and infection rates, the use of antibiotic prophylaxis is highly recommended. Ideally, a ß-lactam antibiotic (penicillins and cephalosporins) should be used preoperatively and postoperatively. In addition, a preoperative and postoperative chlorhexidine regimen will decrease morbidity with implants and bone grafting.
Oral steroids: Oral steroids will increase blood sugar and should be used with extreme caution in diabetics. A physician consult is recommended for patients under treatment for oral hypoglycemic or insulin-related medications.
Dental implants:2
a. Diet-controlled diabetic: Determine and maintain diabetic control
b. Hypoglycemic-controlled diabetic (oral): Determine and maintain diabetic control; stress reduction protocol
c. Insulin-controlled diabetic: Determine diabetic control; stress reduction protocol
THYROID DISORDERS

Thyroid disorders are the second-most common endocrine problem, affecting approximately 1% of the general population, principally women. Synthroid (levothyroxine) is one of the most commonly prescribed drugs in the United States. Because the majority of patients receiving dental implant treatment are women, a slightly higher prevalence of this disorder is seen in dental implant practices. The most common form of hypothyroidism is Hashimoto’s thyroiditis, which is an autoimmune disease whereby the immune system produces antibodies that attack the thyroid gland and create chronic inflammation, which in turn leads to insufficient levels of circulating thyroxine (T4). Decreased levels of T4 affect bone metabolism by decreasing recruitment and maturation of bone cells, and therefore reduces bone growth factors such as insulin-like growth factor.
Dental Implant Implications: Relative contraindication
Studies have shown that hypothyroid patients exhibit greater bone loss and a less favorable soft-tissue response after implant surgery, but no significant increased risk of failure. The patient should be informed of possible increased complications and strict thyroid control should be maintained.3
HYPERPARATHYROIDISM
Hyperparathyroidism results when there is an excess of parathyroid hormone (PTH) in the bloodstream caused by overactivity of one or more of the parathyroid glands that maintain calcium balance. The clinical manifestations of this disease vary widely depending on the severity. In the oral and maxillofacial regions, altered trabecular bone patterns may be present that result in mobility of the teeth and compromised bone density. An altered trabecular bone pattern with the appearance of ground glass may also occur.
Dental Implant Implications: Relative or absolute contraindication
Dental implants and bone grafting are contraindicated (absolute) in areas of active bony lesions resulting from hyperparathyroidism. However, implant placement and bone grafting procedures may be initiated after treatment and healing of the affected areas. A thorough medical consultation and clearance is recommended.4
OSTEOPOROSIS
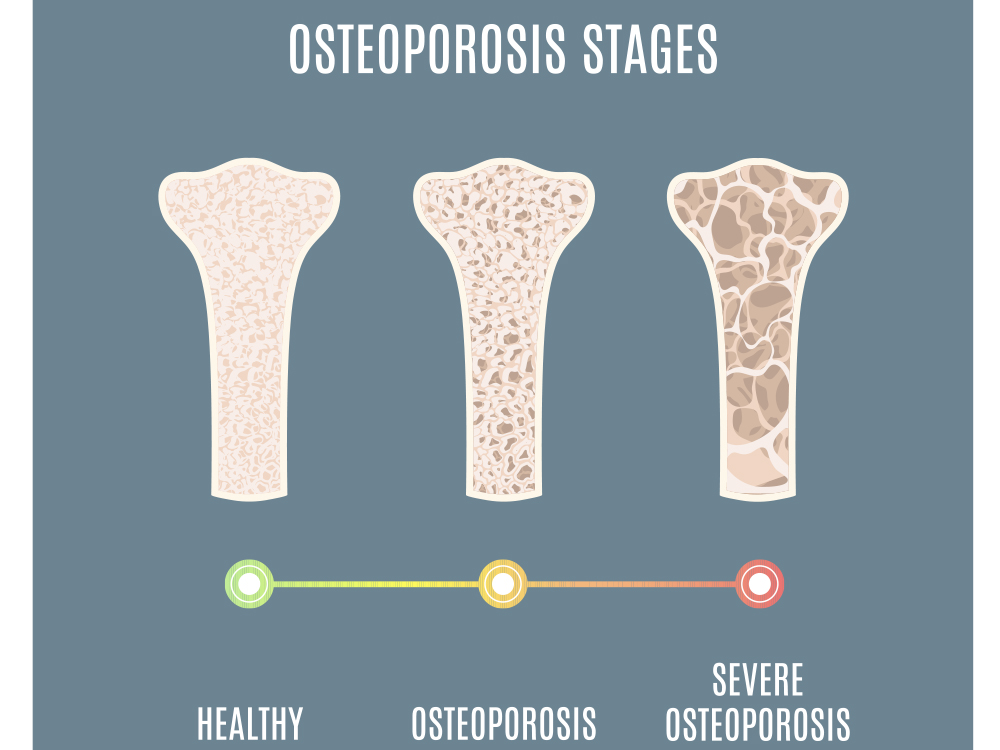
The most common disease of bone metabolism the implant clinician will encounter is osteoporosis, which is an age-related disorder characterized by a decrease in bone mass, increased microarchitectural deterioration and susceptibility to fractures. The World Health Organization (WHO) defines osteoporosis as a bone mineral density level more than 2.5 standard deviations below the mean of normal young women.
Dental Implant Implications: Relative or absolute contraindication
Surgical technique: Because of the poorer bone quality, under-preparation of the osteotomy site is recommended as this results in increased bone-implant contact. Immediate stabilization of dental implants is more difficult, and healing periods and implant surface characteristics should be selected to maximize performance in poorer-quality bone.
Bisphosphonates and monoclonal antibody use: Bisphosphonates and monoclonal antibodies are common medications for the treatment of osteoporosis, which may result in medication-related osteonecrosis of the jaw (MRONJ). Depending on the duration of treatment and specific medication, implant treatment may be a relative or absolute contraindication. Physician consultation is highly recommended with patients on these medications.
Peri-implantitis: A strong correlation has been shown between peri-implant disease and skeletal osteoporotic changes. A strict regimen of postoperative recall and soft- and hard-tissue evaluation should be followed.
Progressive bone loading: Because of poorer bone quality, healing is compromised, which results in longer healing periods. Progressive bone loading techniques should be utilized during prosthetic rehabilitation. The poorer-quality bone is progressively increased to better-quality bone, which results in more favorable bone quality at the implant interface.1
FIBROUS DYSPLASIA
Fibrous dysplasia (FD) is a nonheritable, genetic disorder characterized by normal bone being replaced by immature, haphazardly distributed bone and fibrous tissues. The etiology of this bone disease is a gene mutation that prevents the differentiation of cells within the osteoblastic formation. FD can be further classified to involve one site (monostotic FD [MFD]), multiple sites (polyostotic FD [PFD]), or multiple locations (craniofacial FD [CFD]). CFD lesions are usually unilateral and occur twice as often in the maxilla versus mandible.
Dental Implant Implications: Relative or absolute contraindication
Postoperative healing: Healing after bone surgery in patients with FD is much different than for those with normal bone. The tissue is hypocellular, which leads to slow healing and an increased infection rate. These local infections may spread throughout the bone and result in more advanced complications.
Dental implants: Patients need to be well informed with a detailed informed consent of the possible morbidity and complications associated with dental implant treatment. Treatment should be based on active lesions (absolute contraindication) or non-active lesions (relative contraindication).1
OSTEOMALACIA (VITAMIN D DEFICIENCY)
Osteomalacia, which is caused by lack of vitamin D, results in less dense bone and is directly related to calcium deficiencies. Vitamin D is synthesized by the body in several steps involving the skin, liver, kidney and intestine. The kidney, in conjunction with PTH, activates vitamin D. With this deficiency, the intestinal uptake and mobilization of calcium from the bone is altered, resulting in hypocalcemia. This will lead to an increased PTH secretion, which increases the clearance of phosphorus, resulting in a decrease in the normal mineralization process.
Dental Implant Implications: Relative contraindication
Treatment for osteomalacia (vitamin D and calcium) is usually successful, with radiographic changes seen months after treatment. Therefore, implant treatment should be postponed until the disease is not active and well controlled.5
XEROSTOMIA
Xerostomia (dry mouth) may have direct or indirect effects on dental implants and bone grafting procedures. A decrease in salivary flow is accompanied by a change in its composition. An increase in mucin and a decrease in ptyalin result in a more viscous and ropy saliva. This results in increased biofilm formation, which allows for a favorable environment for bacterial growth.
Dental Implant Implications: Relative contraindication
Dental implants: Strict use of prophylactic antibiotics and chlorhexidine should be maintained for surgical procedures.
Fixed vs. removable prosthesis: Soft tissue-borne overdentures (RP-5) are contraindicated because of the susceptibility to oral lesions and irritation from tissue-borne implant prostheses. Ideally, patients should be treated with a totally implant-supported overdenture (RP-4) or a fixed prosthesis (FP-3), with no tissue pressure.
PREGNANCY
Elective dental implant surgery procedures are contraindicated for pregnant patients. The radiographs and medications that may be required for implant therapy and the increased stress are all reasons the elective implant surgical procedure should be postponed until after childbirth.
Dental Implant Implications: Absolute contraindication
Elective dental implant therapy should be delayed until after pregnancy. A medical clearance should be obtained before any invasive treatment.1
RADIATION THERAPY
Although the survival rate of patients with head and neck cancer has increased over the last 20 years, it remains one of the deadliest forms of cancer. Aggressive treatment includes surgery, radiation, chemotherapy or a combination therapy that inevitably leaves the patient with compromised anatomy and physiologic functioning. Patients are left with many deficits, including oral mucositis, xerostomia, compromised healing and reduced angiogenesis. This is a direct result of changes in the vascularity and cellularity of hard and soft tissue, damage to the salivary glands, and increased collagen synthesis that results in fibrosis. Because of these detrimental effects on the bone, wound repair and healing are significantly reduced after surgical procedures. When exposed to high levels of radiation, bone undergoes irreversible physiologic changes that include narrowing of the vascular channels (endarteritis), diminished blood flow and loss of osteocytes. In time, the bone becomes non-vital, which leads to limited remodeling and healing potential.
Dental Implant Implications: Relative or absolute contraindication
The most significant risk of placing implants into irradiated bone is osteoradionecrosis (ORN), which is an irreversible devitalization of irradiated bone that is characterized by necrotic, soft bone that fails to heal properly. The pathophysiologic mechanism is an imbalance in oxygen demand and oxygen availability, which is caused by endarteritis of the blood vessels. Clinical symptoms include pain, exposed necrotic bone, pathologic fractures and suppuration. Studies have shown the overall incidence of ORN after radiotherapy to be from 3% to 22%.
Past radiation treatment: Caution must be emphasized with patients who have had past radiation therapy because earlier forms of radiation therapy (pre-1980s) were non-collimated, in contrast to current higher-energy levels that are less destructive. This more destructive radiotherapy has been shown to cause progressive endarteritis, which increases over time.
Amount of radiation exposure: The presently available literature states that implant placement surgery may be completed on patients who have been irradiated at doses lower than 50 Gy. Studies have shown that implants placed in patients with a cumulative radiation effect of 18 to 20 (approximately 48 to 65 Gy standard fractionation) have a rather high success rate. Other reports have shown that doses above a cumulative radiation effect of 40 (approximately 120 Gy standard fractionation) exhibit a high degree of failure. A medical consultation and clearance should be completed before any type of treatment, along with detailed informed consent.6
SMOKING
In the U.S., an estimated 42.1 million people, or 18.1% of all adults age 18 years or older, smoke cigarettes. Smoking has been directly related to many oral diseases, including periodontal disease and dental implant-related complications. Studies have shown that over 7,000 different gases and chemicals are found in cigarette smoke, such as nitrogen, carbon monoxide, carbon dioxide, ammonia, hydrogen cyanide, benzene and nicotine. In tissues, carbon monoxide displaces oxygen from hemoglobin molecules because of its stronger affinity. Multiple retrospective studies have shown that smokers experience almost twice as many implant failures compared with nonsmokers. In addition, it has been shown that smoking is directly related to increased incision line opening.
Dental Implant Implications: Relative contraindication
Implant and bone grafting failure: Meta-analysis studies have shown a definite correlation between smoking and failure rates of implants and bone grafts, as well as a strong correlation between smoking and peri-implantitis.1
Informed consent: Because of the detrimental effects of smoking on implants, it is recommended that patients be informed in detail about the risks of smoking. These possible consequences include increased marginal bone loss after implant placement and the presence of peri-implantitis.
Smoking cessation: Smoking cessation before and after implant surgery is strongly recommended because it has been shown to decrease implant morbidity. The patient is instructed to cease smoking for two weeks before surgery to allow for the reversal of increased blood viscosity and platelet adhesion. Ideally, smoking cessation is continued for eight weeks after implant surgery, which coincides with the osteoblastic phase of bone healing.
ALCOHOL
Ethyl alcohol is one of the most widely used mood-altering drugs in the world. Approximately 17 million U.S. adults aged 18 and older have an alcohol-use disorder. Alcohol interferes with coagulation on multiple levels, leading to decreased platelet production (thrombocytopenia), impaired platelet function (thrombocytopathy), and diminished fibrinolysis. Patients who use alcohol after surgery are more susceptible to intraoperative and postoperative bleeding complications. Use of alcohol leads to significant alterations of cell-mediated immune systems. Alcohol-induced immunosuppression results in a decrease in delayed-type hypersensitivity (DTH), which is a preoperative indicator for postoperative infectious complications. In addition, alcohol use leads to decreased bone formation, increased resorption and decreased osteoblast function, resulting in decreased bone density and integration issues. Alcohol has also shown a direct effect on dental implant healing as studies have reported greater marginal bone loss and implant failure.7
Dental Implant Implications: Relative contraindication
Informed consent: Make sure patients are well informed of the potential increased morbidity associated with alcohol use. Patients should refrain from using alcohol for a minimum of two weeks postoperatively or until the incision line closes.
PSYCHOLOGICAL DISORDERS

Providing dental implant care to patients with psychological problems is very challenging for clinicians. This group of patients is prone to oral health issues because of poor oral hygiene, poor compliance and adverse medication effects. Additionally, many of the drugs used to treat patients with psychological disorders — including tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs) and monoamine oxidase inhibitors — are associated with drug interactions. Oral manifestations of these diseases and medications include an increase in caries and periodontal disease, increased smoking, xerostomia, chronic facial pain, parafunction (bruxism and clenching) and temporomandibular joint dysfunction.1
Dental Implant Implications: Relative contraindication
Many psychotherapeutic drugs interact with medications that are commonly prescribed in implant dentistry. Clinicians must be aware of drug-drug and drug-disease interactions with respect to the patient’s medical history. Most interactions are related to the potentiation of the sedative and anti-cholinergic actions of the psychotherapeutic drugs.
TITANIUM ALLERGY
Hypersensitivity to titanium is an ever-increasing reportable complication in medicine today. There are many case reports of titanium alloy hypersensitivity, including failures of total hip prostheses, titanium-implanted cardiac pacemakers, surgical clips and dental implants. With respect to dental implants, there appears to be an allergic correlation with titanium implants, which unfortunately is not fully understood because of limited research. In the dental literature, reports of allergic reactions to titanium implants are minimal. However, it is widely accepted that the true incidence of titanium hypersensitivity is underreported, mainly from a poor understanding of failure or allergy.
Dental Implant Implications: Relative contraindication
Titanium hypersensitivity is usually diagnosed by signs and symptoms that may include a rash, urticaria, pruritus, localized soft-tissue inflammation, swelling in the orofacial region, oral or facial erythema, eczema lesions of the face, or hyperplastic peri-implant mucosa. In some cases, implant failure may result, usually as early implant failure (rapid exfoliation). Clinical reports have associated titanium allergy with multiple implant failure in the same patient. To test for a true titanium allergy, the lymphocyte transformation (blood) test (LTT) or Memory Lymphocyte Immuno-Stimulation Assay (MELISA®) have been shown to detect sensitization to titanium in patients. In addition, the MELISA test is capable of determining which metals may be tolerated and which may initiate undesirable immune responses. If a true allergy is determined, then titanium-based implants are contraindicated and the use of zirconia implants may be considered.8
SJÖGREN’S SYNDROME
Sjögren’s syndrome is an autoimmune disease in which immune cells attack and destroy exocrine glands that produce saliva and tears. This disorder affects an estimated 4 million people in the U.S., 90% of whom are female, and has an average age of onset in the late 40s. The classic symptoms of Sjögren’s syndrome are xerostomia and xerophthalmia (dry eyes). Because of the xerostomia, patients are more susceptible to decay and the mucous membranes become atrophic and friable. With the lack of salivary secretions, complications may arise with the use of a tissue-borne prosthesis. Therefore, implant-supported prostheses are recommended as they decrease soft tissue-borne prosthetic sore spots and discomfort. The healing response and integration of implants have been shown to be successful in patients with Sjögren’s syndrome.
Dental Implant Implications: Relative contraindication
There are no contraindications for dental implants in patients with a history of Sjögren’s syndrome. However, it is advantageous for the prosthesis to be non-tissue borne (FP-1, FP-2, FP-3 and RP-4) to minimize soft-tissue complications associated with xerostomia.
SYSTEMIC LUPUS ERYTHEMATOSUS
Systemic lupus erythematosus is a chronic, potentially fatal autoimmune disease in which the immune system attacks cells and tissue in almost any part of the body. There are three main types of lupus in adults. The majority of patients have systemic lupus, which occurs at a rate eight times higher than other forms and causes the immune system to attack cells and tissue in several areas of the body. Lupus occurs in both men and women, but almost 90% of the cases are in women. Most related symptoms can be controlled with corticosteroids and immunosuppressive drugs.1
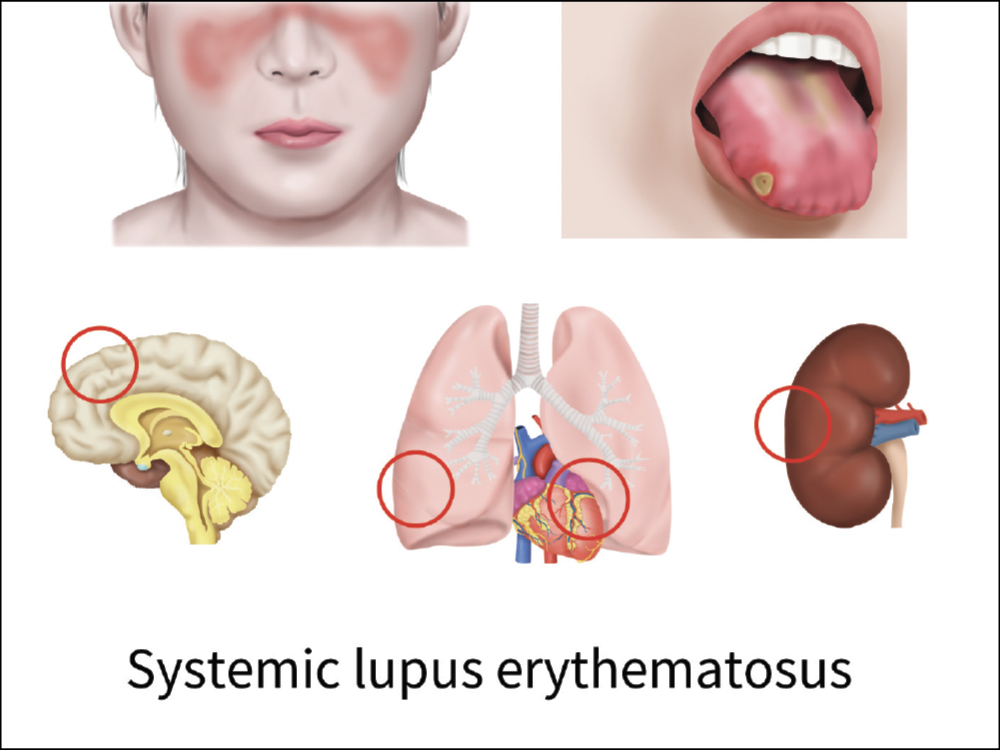
Dental Implant Implications: Relative contraindication
There is no direct contraindication to dental implant treatment in systemic lupus erythematosus patients. However, caution should be taken for possible associated organ damage and the use of high doses of corticosteroids and immunosuppressive drugs, which may contraindicate dental implants in those individuals.
SCLERODERMA
Scleroderma is a chronic autoimmune disease characterized by excessive deposits of collagen that cause musculoskeletal, pulmonary and GI involvement. The disease is most common in women between the ages of 30 and 50. There are two main types: localized and systemic. Localized scleroderma usually attacks the skin and on occasion the muscle and joints, but it spares the internal organs. These patients usually have discolored patches on the skin (morphea). There is no cure for scleroderma. Treatment usually includes non-steroidal anti-inflammatory drugs (NSAIDs) and immunosuppressant medications.
Dental Implant Implications: Relative contraindication
Numerous reports have discussed the successful treatment of scleroderma patients with dental implants. A fixed prosthesis is recommended because of the inability to retrieve a removable prosthesis due to possible dexterity problems. However, a high percentage of these patients are being treated with immunosuppressive drugs, which may contraindicate implant therapy.1
RHEUMATOID ARTHRITIS
Rheumatoid arthritis (RA) is a chronic, inflammatory autoimmune disease that causes the patient’s immune system to attack the muscles and joints of the body. It is more prominent in the early stages in the fingers, wrists, feet and ankles rather than the larger joints, such as the shoulders, hips or knees. RA is different from osteoarthritis, which is caused by wear and tear as well as previous injuries. In RA, the disease affects the lining of the joints, which increases pain and swelling, and results in significant bone erosion and deformity of the joints. The inflammation in RA can affect other organs in the body. Methotrexate, a drug used to treat cancer, is commonly used to treat RA. Studies have shown the detrimental effect of this medication on bone by delaying bone healing. However, other studies have concluded that low-dose methotrexate treatment does not affect titanium implant osseointegration.

Dental Implant Implications: Relative or absolute contraindication
There is no direct contraindication for dental implants in patients who have RA. Because of the lack of mobility and dexterity, a fixed-implant restoration is indicated. Special attention should be given to the patient’s current medications because immunosuppressive, glucocorticoid therapy and biologics may contraindicate implant treatment.1
HUMAN IMMUNODEFICIENCY VIRUS
Human immunodeficiency virus (HIV) is a retrovirus that is responsible for acquired immunodeficiency syndrome (AIDS), which causes the immune system to be depressed, leading to life-threatening opportunistic infections. There is no cure for either HIV or AIDS; however, revolutionary new antiretroviral medication and protease inhibitors developed since 1996 have now been able to eliminate active viral load titers from the bloodstream. Many patients demonstrate complete suppression of the virus while taking the medication. Although not a cure, the inactivity improves survival and limits the effect on other organs.
Dental Implant Implications: Relative or absolute contraindication
Numerous reports have shown successful dental implant therapy in HIV patients; however, there is insufficient data to determine the association between HIV infection and the success of dental implants. Special care (medical consultation) must be taken to evaluate the current status of the patient’s immune system and the potentially toxic medications the patient is taking.9
ELDERLY (INCREASED AGE)
Studies have shown that elderly patients are more prone to systemic diseases and comorbidities. They also have potentially longer healing periods, more challenging bone conditions (quality and quantity), increased susceptibility to drug interactions and increased dental implant morbidity. In addition, decreased renal function, decreased gastric motility and isolated systemic hypertension are all potential medical issues. The implant clinician must understand the physical, metabolic and endocrine changes, and the effects associated with the elderly patient, before initiating implant treatment. Age is most certainly a prognostic factor in implant failure and morbidity. However, advanced age is not an absolute contraindication to implant therapy. It is imperative that the clinician obtain a detailed medical history and list of medications before completing a dental treatment plan. Patient education along with modification in medication use, surgical technique, soft- and hard-tissue healing times, and careful assessment of postoperative complications is required.1
Dental Implant Implications: Relative contraindication
Delayed bone healing: Clinical studies have shown a direct correlation between delayed bone healing and increasing age. Most likely the etiology results from a reduced number of osteogenic cells and reduced systemic and localized blood flow to the healing site. Therefore, longer healing periods along with progressive loading protocols are recommended.
Bone quality: Both the quality and quantity of bone is affected by aging. Histomorphometric and microradiographic studies have shown that after the age of 50, a marked increase in the cortical porosity leads to decreased bone mass. Loss of bone mineral content has been estimated to be approximately 1.5% per year in females and 0.9% in males.10
Implant failure rate: Studies have shown an increased risk of implant failure as a result of many age-related factors, including compromised bone quality and quantity, implant length, treatment protocol and edentulous locations. Other studies have shown patients greater than 60 years of age were twice as likely to have adverse outcomes.
Adaptation to implant prostheses: Elderly patients have been shown to have increased difficulty in adapting to the final implant prostheses. Post-insertion issues such as general adaptation, muscle control, hygiene difficulty, tissue inflammation and overdenture seating are significant in the older population. Patient education and final expectations should be discussed in detail before initiating treatment.1
ADOLESCENCE (DECREASED AGE)
Dental implants are commonly used to correct the congenital absence of teeth in adolescents, and studies have shown this to be a very reliable and predictable treatment option. When a clinician is presented with an adolescent patient, there must be a degree of caution as to the ideal time that implant therapy should be commenced. The concern is that placement of implants too early may lead to the implants interfering with normal growth and development, potentially causing esthetic issues. If placement of an implant is completed before craniofacial growth is complete, possible interruption of facial growth and esthetic issues (infraocclusion or labioversion) can result.
Dental Implant Implications: Relative or absolute contraindication
In determining the ideal time for implant placement, the patient or family must be educated on craniofacial growth compared with chronologic age. Chronologic age is a poor indicator of dental development and facial growth, and the timing of implant placement should coincide with growth cessation. In the literature, there are many methods of determining completion of craniofacial/skeletal growth: chronologic age, complete dental development, voice changes, hand-wrist radiographs, cervical vertebral maturation and superimposition of lateral cephalometric radiographs. The most reliable and safest (no radiation exposure) method has been shown to be when the patient begins to exhibit a lack of growth in stature (less than 0.5 cm/year).1
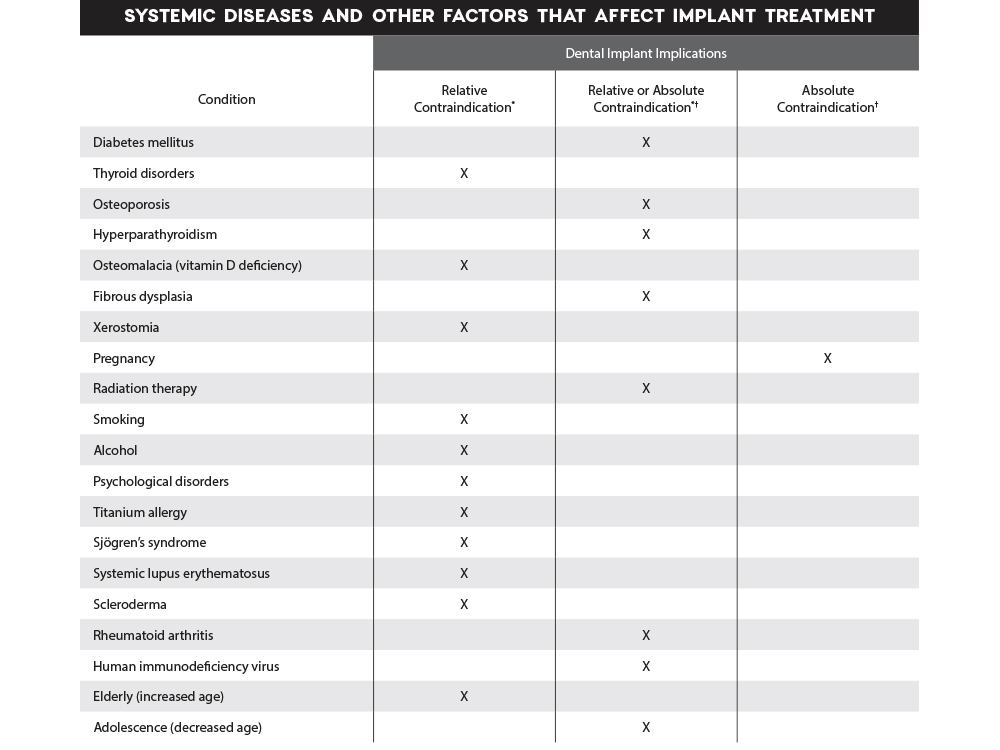
Relative contraindication is a condition that necessitates caution and is acceptable as long as the benefits outweigh the risks. In most cases, precautions need to be taken and the intended procedure may require some degree of modification to ensure safety and success.
†Absolute contraindication is a condition that may result in major and significant medical problems with a high incidence of implant or bone graft failure. The risk of performing the procedure clearly outweighs any possible benefit. Undertaking procedures when these conditions are present is inadvisable.
CONCLUSION
There is a broad array of systemic conditions that may have a direct impact on dental implant procedures. Depending on the severity of the disease, most conditions may be considered as no contraindication, relative contraindication or absolute contraindication. It is imperative that the implant clinician obtain a detailed medical history and in many situations obtain a medical consultation and clearance prior to treatment.
MELISA is a registered trademark of MELISA Diagnostics Ltd.
References
- ^Resnik RR. Misch’s 4th edition contemporary implant dentistry e-book. Elsevier Health Sciences; 2020.
- ^Resnik RR, Misch CE. Misch’s avoiding complications in oral implantology e-book. Elsevier Health Sciences; 2017.
- ^Attard NJ, Zarb GA. A study of dental implants in medically treated hypothyroid patients. Clin Implant Dent Relat Res. 2002;4(4):220-31.
- ^Henrikson P. Periodontal disease and calcium deficiency: an experimental study in the dog. Acta Odontol Scand. 1968;26:Suppl 50:1-132.
- ^Bryce G, MacBeth N. Vitamin D deficiency as a suspected causative factor in the failure of an immediately placed dental implant: a case report. J R Nav Med Serv. 2014;100(3):328-32.
- ^Anderson L, Meraw S, Al-Hezaimi K, Wang HL. The influence of radiation therapy on dental implantology. Implant Dent. 2013 Feb;22(1):31-8.
- ^de Deco CP, da Silva Marchini AM, Marchini L, da Rocha RF. Extended periods of alcohol intake negatively affects osseointegration in rats. J Oral Implantol. 2015 Jun;41(3):e44-9.
- ^Egusa H, Ko N, Shimazu T, Yatani H. Suspected association of an allergic reaction with titanium dental implants: a clinical report. J Prosthet Dent. 2008 Nov;100(5):344-7.
- ^Shetty K, Achong R. Dental implants in the HIV-positive patient — case report and review of the literature. Gen Dent. Nov-Dec 2005;53(6):434-7.
- ^Moy PK, Medina D, Shetty V, Aghaloo TL. Dental implant failure rates and associated risk factors.