Supporting Long-Term Soft-Tissue Health: Choosing the Best Restorative Materials

CASE REPORT
The monolithic zirconia restorations available today are substantially more versatile and natural-looking than those released a decade ago. While the original monolithic zirconia formulations, including BruxZir® Full-Strength Zirconia, have rightfully developed a reputation for reliability in posterior restorations that require toughness, the advanced materials now on the market are ideal for anterior, esthetically demanding cases.
As these zirconia restorations become more widely used in the anterior, it is important to highlight an additional key benefit of the material — polished zirconia restorations have been found to elicit a better soft-tissue response than other ceramics.1 Not only do these new zirconia solutions offer strength and translucency, but they also allow for better interaction between the tissue and ceramic to ultimately produce a healthier-looking result.
In the case that follows, lab-fabricated BioTemps® Provisionals and BruxZir Esthetic Zirconia are used to create a complete restorative makeover.

Figure 1: Her pre-restorative condition included diastemata, prominent labial frenum attachment, enamel fluorosis, caries, a missing tooth at site #30 and a high smile line. A comprehensive treatment plan was developed for a full-mouth makeover, which included caries control, labial frenectomy, Invisalign® treatment (Align Technology, Inc.; Tempe, Ariz.) to move the teeth into a more favorable restorative position, implant placement at site #30, maxillary anterior gingivectomies, BioTemps Provisionals, and the delivery of BruxZir Esthetic crowns on teeth #2–15 and #18–30.


Figures 2a, 2b: After completion of her caries control, labial frenectomy and orthodontic treatment, digital impressions were taken and sent to the laboratory. BioTemps Provisionals, shown here on a 3D-printed model, were fabricated by the lab.

Figure 3: To ensure accurate placement of the BioTemps Provisionals, a thermoformed stent provided by the laboratory was utilized as a positioning guide.

Figure 4: This thermoformed stent has many uses, and in this case, I also utilized it as a reduction guide and a gingival-contouring guide. Knowing that the definitive restorative material would be BruxZir Esthetic, preparations were created with chamfer margins and room for 1.25 mm of material thickness, with transitional edges, angles, and corners rounded off. Then, using a Waterlase tissue laser (BIOLASE, Inc; Foothill Ranch, Calif.), I followed the contours of the stent to perform a gingivectomy.
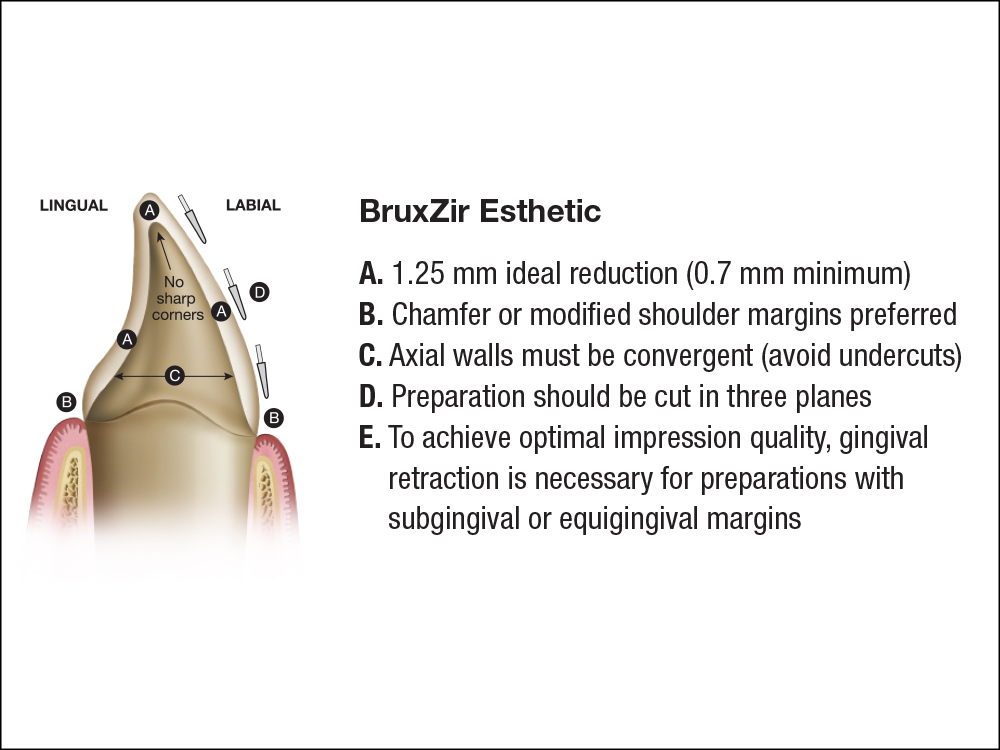
Figure 5: One issue dental technicians often experience is when tooth preparations do not meet the material-specific reduction requirements. This forces a choice between creating restorations with minimal material thickness and reduced strength, or requesting that the dentist reduce more after the restorations have been returned to the practice, which may compromise the fit. It is vital that clinicians are familiar with and follow the specific preparation requirements of the material they plan on utilizing.

Figure 6: Then, I used the stent to seat the BioTemps Provisionals to ensure the correct orientation.

Figure 7: Approximately one month later, after the soft tissue had healed, the patient returned for an impression appointment for the final restorations. In addition to taking impressions of the preparations, impressions were taken of the BioTemps in place to communicate minor adjustments back to the laboratory.

Figure 8: The definitive restorations were all single-unit crowns made from BruxZir Esthetic Zirconia. For this case I selected BruxZir Esthetic because it provides the desired strength, natural-looking translucency, and perhaps most importantly, a soft-tissue response that’s comparable to that of natural teeth.


Figures 9a, 9b: The treatment resulted in a transformative smile makeover for the patient. Upon completion of the treatment, she remarked: “Having a new smile has been rewarding in ways that I couldn’t have imagined. While I’ve always felt confident, my new smile is exciting and gives me opportunities to explore something new.”




Figures 10a–10d: From initial presentation (a), to post-Invisalign treatment (b), to provisionalization (c), to the final restorations (d), the treatment plan kept tissue health in mind to ensure a lifelike, transformative result.

CONCLUSION
While key factors in maintaining soft-tissue health over the long term include the patient’s adherence to a hygiene protocol and healthful habits, clinicians can position patients for soft-tissue success by choosing the right materials and techniques for both the provisional and definitive phases.
References
- ^ Tetè S, et al. Proliferation and adhesion capability of human gingival fibroblasts onto zirconia, lithium disilicate and feldspathic veneering ceramic in vitro. Dent Mater J. 2014;33(1):7-15