Socket Grafting: When to Graft and What to Use (1 CEU)

The dental profession has seen significant advancements in the understanding of bone healing at the cellular and molecular level, and this has led to techniques that have expanded the scope of oral implantology. One such technique is socket grafting for predictable bone regeneration and successful implant placement.
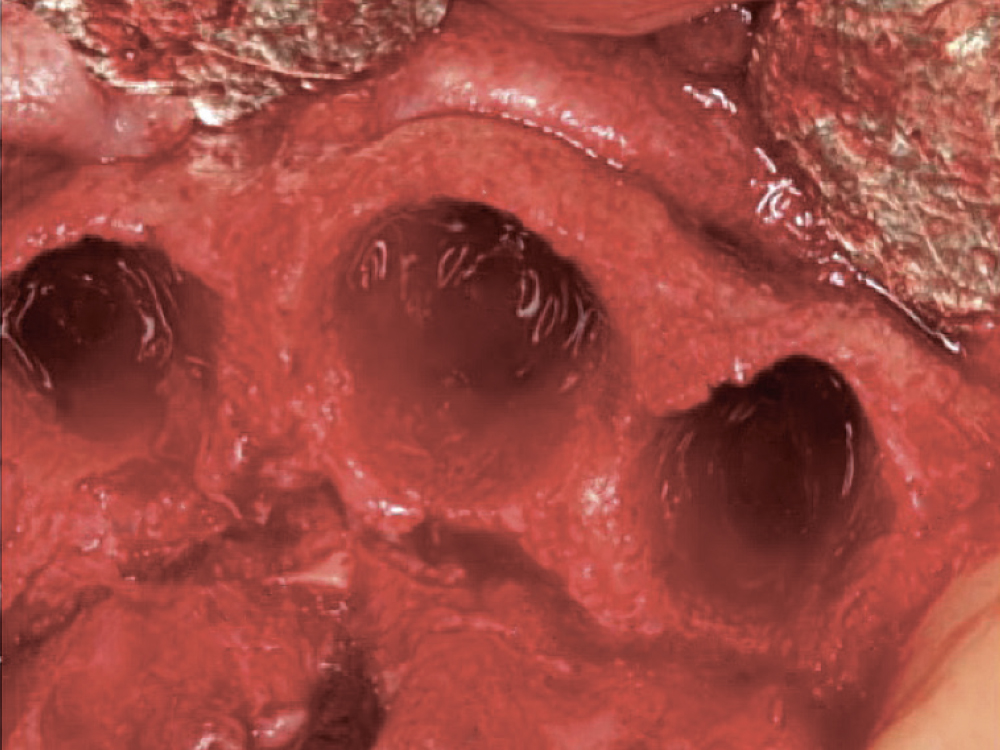
After a tooth extraction, clinicians have several options, including immediate implant placement, socket grafting or no socket grafting. If all socket walls are present and the surgical anatomy is ideal, immediate replacement is often the preferred method of treatment. However, if an implant will not be placed immediately, the clinician should evaluate and classify the extraction site based on the number of walls remaining.
A comprehensive explanation of grafting situations — including extraction site healing, along with indications and contraindications of socket grafting— has been provided in Chairside® magazine Vol. 14, Iss. 2. A step-by-step socket grafting protocol, including various techniques that are specific to the anatomy of the particular extraction socket — are explained in Chairside magazine Vol. 14, Iss. 3. Here, we will present simplified clinical recommendations for regenerative material selection. Using this guide will help practitioners in their clinical decision-making.
A tooth socket contains five walls: the mesial, distal, buccal, lingual and apical.1 The number of walls remaining after tooth extraction dictates whether the site should include bone grafting. Although there is no consensus with respect to a generalized and ideal type of bone grafting material and barrier membrane to use at all times, when grafting is recommended, the Newport Biologics™ line of regenerative materials (Glidewell Direct; Irvine, Calif.) helps dentists simplify the procedure, and Table 1 includes the types of materials recommended for each situation.
After a tooth extraction, clinicians have several options, including immediate implant placement, socket grafting or no socket grafting.
For example, most sockets can be bonegrafted with mineralized freeze-dried allograft, such as Newport Biologics Mineralized Cortico/Cancellous Allograft Blend. The amount of material typically required for various extraction sites are as follows: 0.5–1.0 cc for centrals and canines, 0.5 cc for laterals, 0.5–1.0 cc for bicuspids and 1.0–2.0 cc for molars.
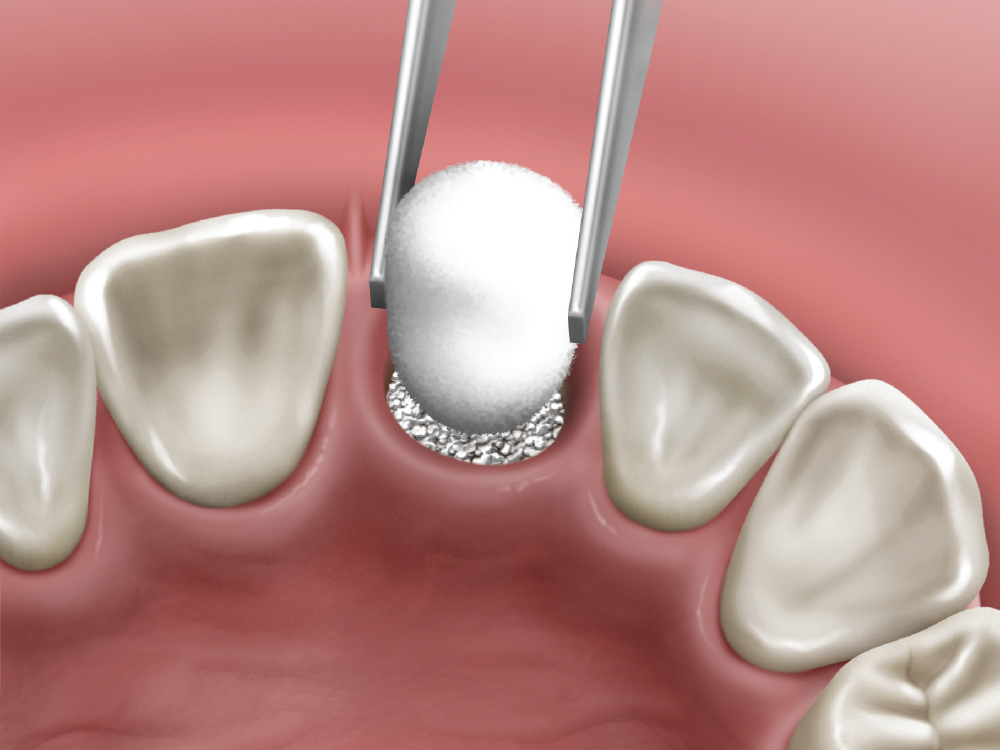
Because soft-tissue cells migrate at a faster rate than bone-forming cells, a biocompatible barrier membrane is recommended in conjunction with the socket graft procedure to prevent soft-tissue invasion. Newport Biologics Resorbable Collagen Membranes, available with two different resorption schedules of 3–4 months and 4–6 months, are advantageous as they are cost-effective, easy to use and naturally biodegradable. In general, the larger the socket or the more missing walls, the longer-acting the membrane should be for that site.
A biocompatible barrier membrane is recommended in conjunction with the socket graft procedure to prevent soft-tissue invasion.
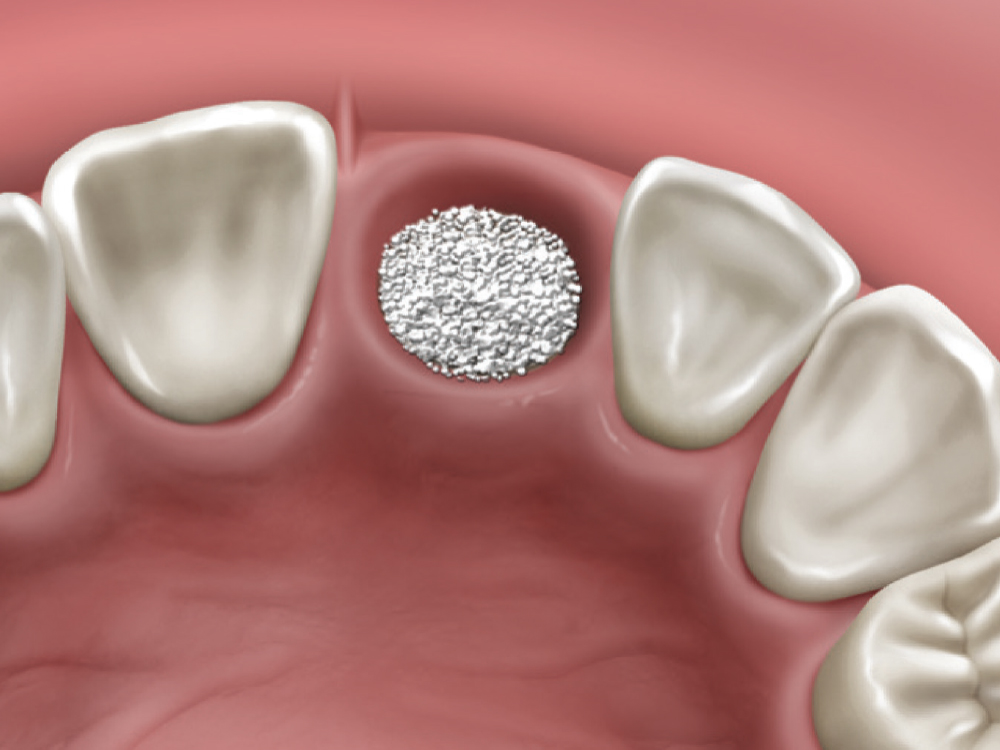
A faster-resorbing collagen, such as Newport Biologics Resorbable Collagen Plug, may be used over the socket when all walls of the extraction socket are intact (five-walled socket), but are insufficient in thickness (less than 1.5 mm).
AVERAGE BONE GRAFT VOLUME FOR EXTRACTION SOCKETS
Centrals, Canines: 0.5–1.0 cc
Laterals: 0.5 cc
Bicuspids: 0.5–1.0 cc
Molars: 1.0–2.0 cc
CONCLUSION
To increase the predictability of bone growth, clinicians must first identify the type of extraction socket and determine whether grafting is recommended.
When all five walls of the socket are present, but one or more walls are thin (less than 1.5 mm), socket grafting is indicated. When additional walls are missing, socket grafting is highly recommended. When indicated, regenerative materials, used along with the proper surgical protocol and techniques, help to maximize treatment success.
TABLE 1 — TO GRAFT OR NOT TO GRAFT: SOCKET GRAFTING MATERIALS BASED ON THE NUMBER OF WALLS
Five-Walled Defect — Thick Bony Plates Greater Than 1.5 mm
Optional
A five-walled extraction socket, where all the bony walls are present, is the most predictable to treat. If the walls are thick (greater than 1.5 mm) and have the interseptal bone remaining, then grafting of the socket is not necessarily required.
Five-Walled Defect — Thin Bony Plate(s) Less Than 1.5 mm
Recommended
With some five-walled extraction sockets, one or more of the bony walls may be considered thin (less than 1.5 mm). Because of the bony wall thinness, the predictability of maintaining the socket volume is reduced. This is most common in the maxillary anterior region, as the average thickness has been shown to be less than 1 mm.2 In these types of sites, grafting of the socket is recommended regardless of the anatomic location. Bone grafting allows for space maintenance and a more predictable regenerative process.
Regenerative Materials
- Graft: Newport Biologics Mineralized Cortico/ Cancellous Allograft Blend hydrated with sterile saline (0.9% sodium chloride) or platelet-rich fibrin (PRF)
- Membrane: Newport Biologics Resorbable Collagen Plug cut in half and hydrated with 0.9% sodium chloride
Four-Walled Defect
Highly Recommended
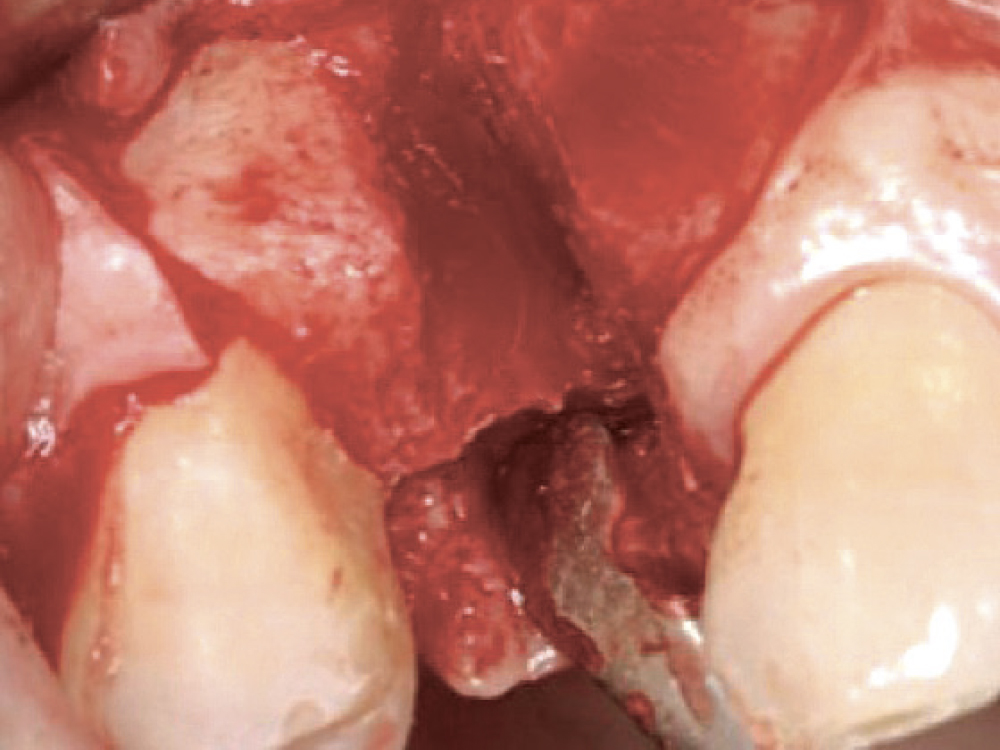
With a four-walled extraction socket, one wall is missing — typically the buccal or facial plate. When the buccal plate is missing and not treated properly, the absence of the wall prevents space maintenance, reduces host bone vascularization, allows for the migration of bone graft material, and increases the possibility of softtissue invasion. Therefore, it’s recommended to use a longer-acting membrane over the missing buccal plate. The membrane will maintain the space and prevent loss of bone material.
Regenerative Materials
- Graft: Newport Biologics Mineralized Cortico/ Cancellous Allograft Blend hydrated with sterile saline (0.9% sodium chloride) or platelet-rich fibrin
- Membrane: A longer-acting collagen cross-linked membrane (e.g., Newport Biologics Resorbable Collagen Membrane, with a resorption rate of 3–4 or 4–6 months) trimmed in a modified V-shape
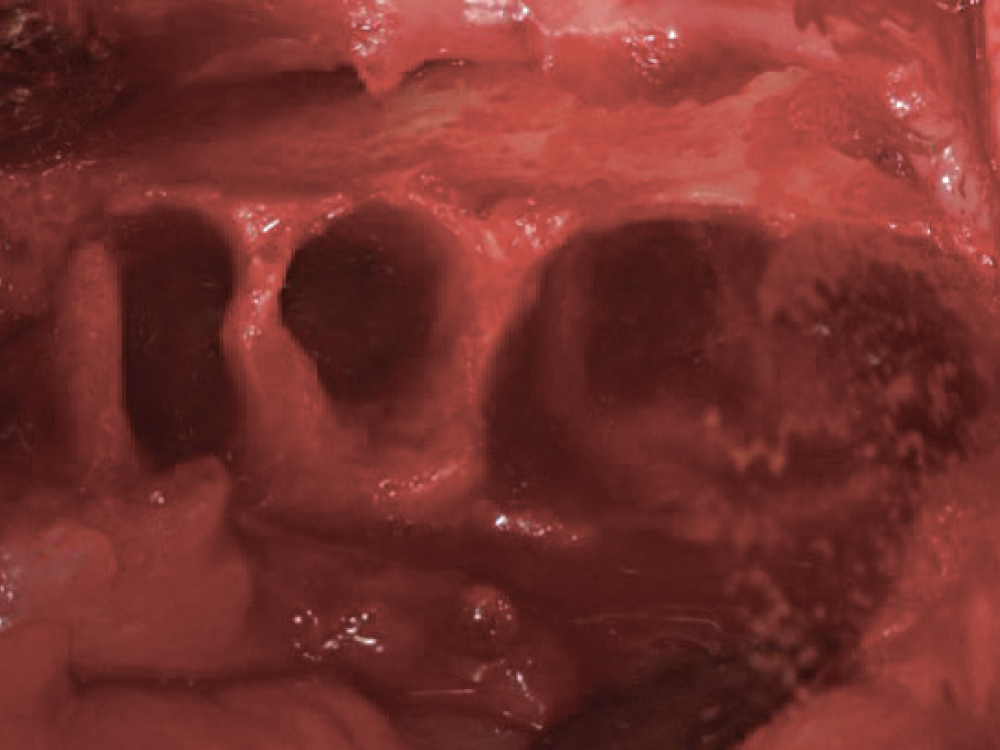
Three-, Two- or One-Walled Defects
Highly Recommended
When multiple socket walls of bone are missing, there is a greater need for the use of autogenous bone along with an allograft material. Although these types of defects are commonly grafted solely with allograft material to simplify the surgical procedure, a particulate graft alone can be very unpredictable. For most three-walled defects, a donor site is most often used to obtain autogenous bone — typically the mandible (i.e., ramus, symphysis) or maxilla (i.e., tuberosity). In some cases, a membrane tent screw may be indicated to increase space maintenance and predictability.
Two- and one-walled sockets are very rare and usually will require autogenous block grafting. In addition, biologic growth factors (platelet-rich fibrin, platelet-rich plasma, and bone morphogenic protein) are often used to increase the predictability and success of the bone graft. See Chairside magazine Vol. 15, Iss. 1, for more information about enhancing bone regeneration with the use of platelet concentrates.
Regenerative Materials
- Graft: Autogenous harvested bone as the first layer and particulate allograft (e.g., Newport Biologics Mineralized Cortico/Cancellous Allograft Blend) to fill in any voids and to maintain space
- Membrane: For most three-walled sockets, a long-acting membrane (e.g., Newport Biologics Resorbable Collagen Membrane 4–6) modified to encompass the missing socket walls; membrane tacks may be used to preventany micromovement of the membrane
Available CE Course
References
- ^Misch CE, Suzuki JB. Tooth extraction, socket grafting, and barrier membrane bone regeneration. In: Misch CE, editor. Contemporary Implant Dentistry, 3rd ed. St. Louis: Mosby; 2008. p. 870-904.
- ^Vera C, De Kok IJ, Reinhold D, Limpiphipatanakorn P, Yap AK, Tyndall D, Cooper LF. Evaluation of buccal alveolar bone dimension of maxillary anterior and premolar teeth: a cone beam computed tomography investigation. Int J Oral Maxillofac Implants. 2012 Nov-Dec;27(6):1514-9.