Full-Arch Immediate Loading Using a Multi-Level Surgical and Prosthetic Guide (1 CEU)

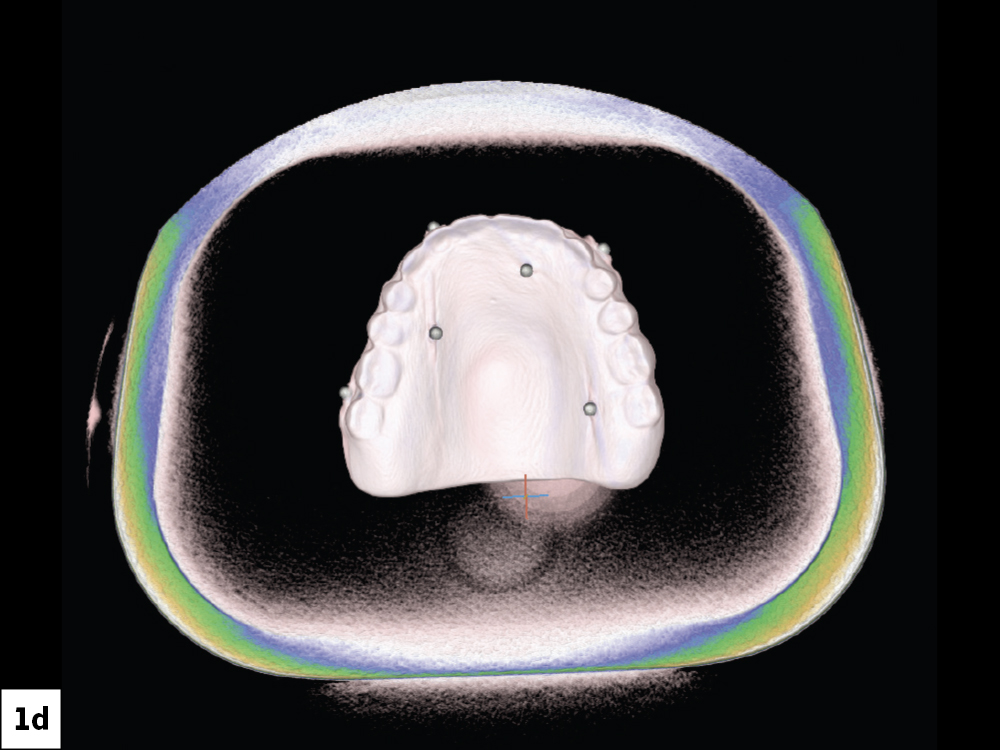
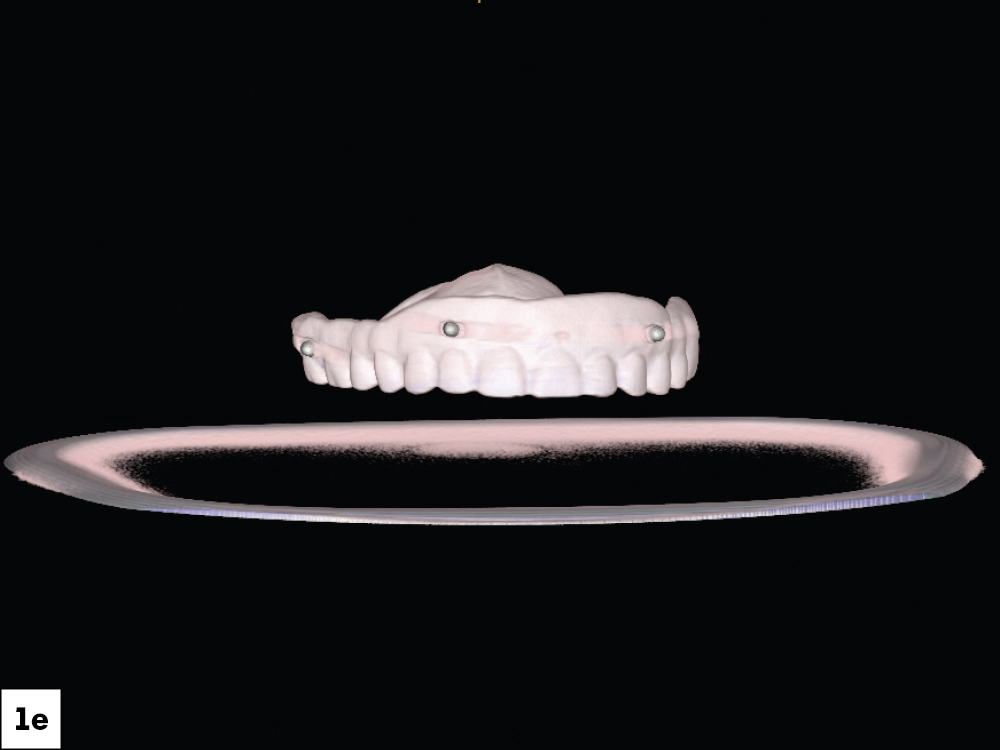
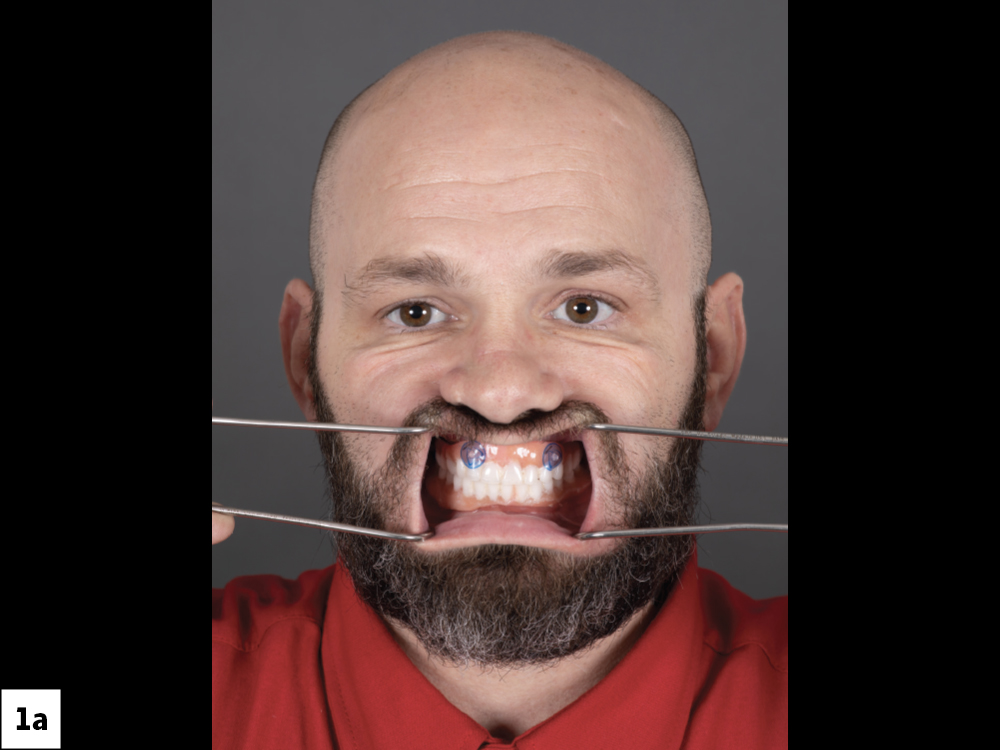
This patient presented wearing upper and lower complete dentures. While the removable dentures fit well, were easy to maintain, and provided acceptable esthetics, the patient sought a fixed prosthesis as a long-term solution.
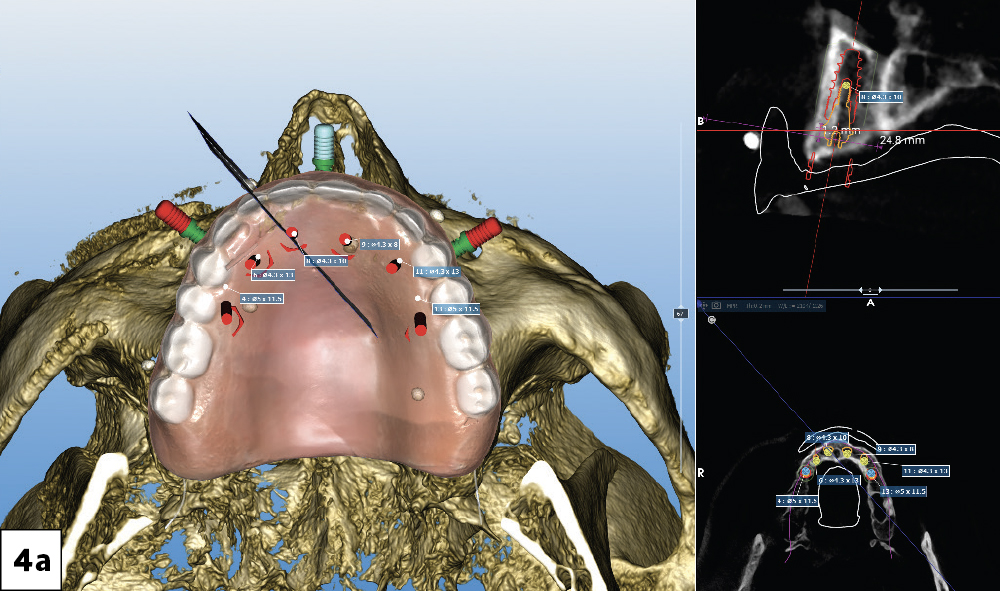
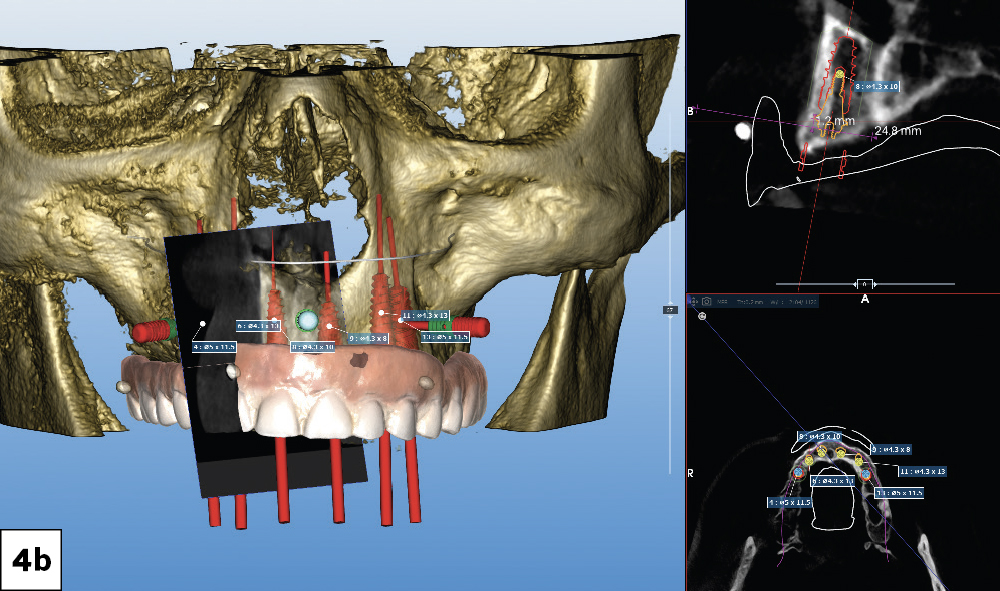
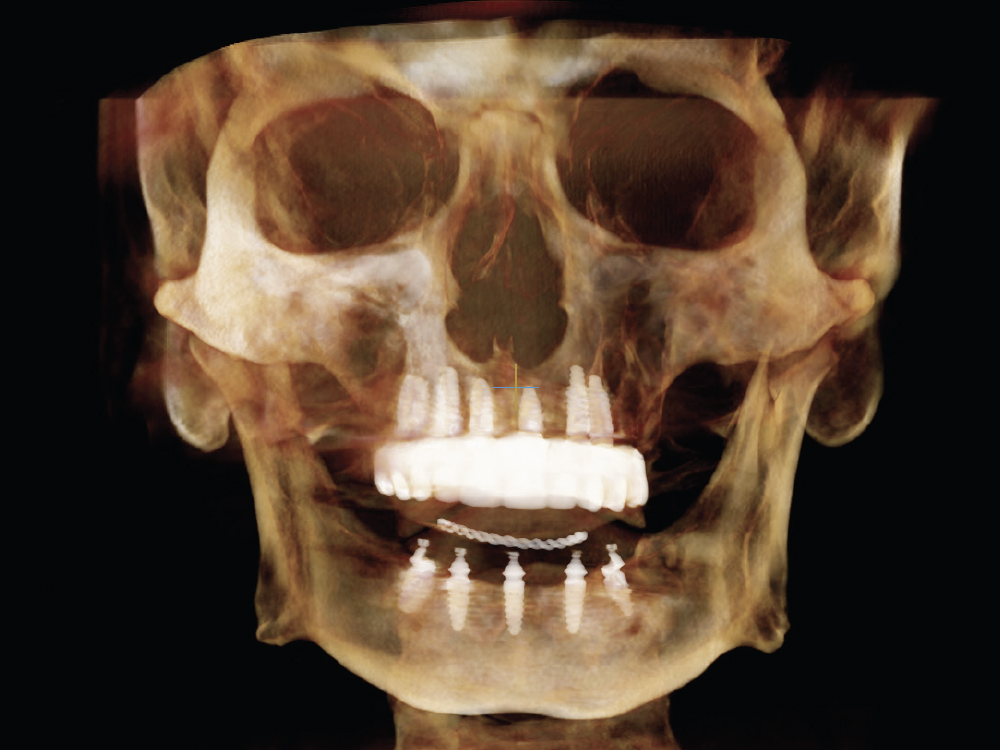
Prosthetically driven treatment planning requires careful collaboration from the lab, the restorative dentist and the surgeon. Based on our treatment goals for this case, we selected a multi-level surgical guide (Glidewell; Newport Beach, Calif.) for increased predictability and efficiency. In this case report, we will elaborate on the treatment of the maxillary arch utilizing a multi-level guided surgery protocol, from the treatment plan to the delivery of the provisional screw-retained implant prosthesis.
PREPARATION
LEARN MORE
The dual-scan protocol is essential to achieving a predictable outcome for your full-arch guided surgery cases. You can find it by visiting glidewell.com/dtp.
MULTI-LEVEL SURGICAL GUIDE
The multi-level surgical guide is a “stackable” approach to full-arch implant surgery and immediate loading that provides maximum efficiency and predictability with what has traditionally been a complex surgical and restorative procedure.
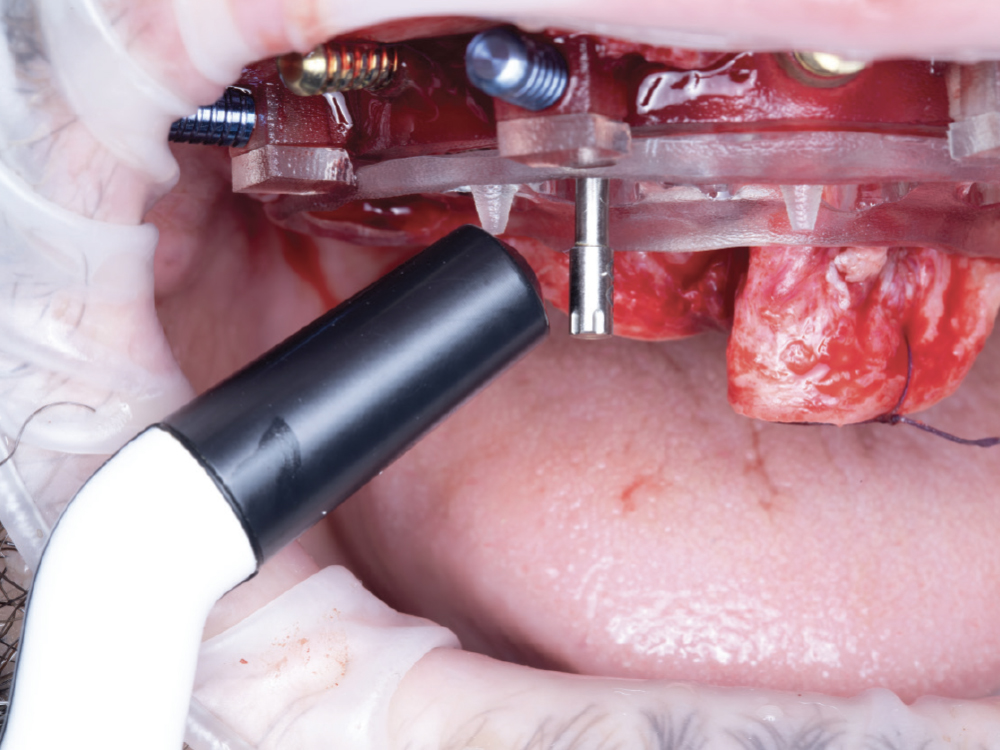
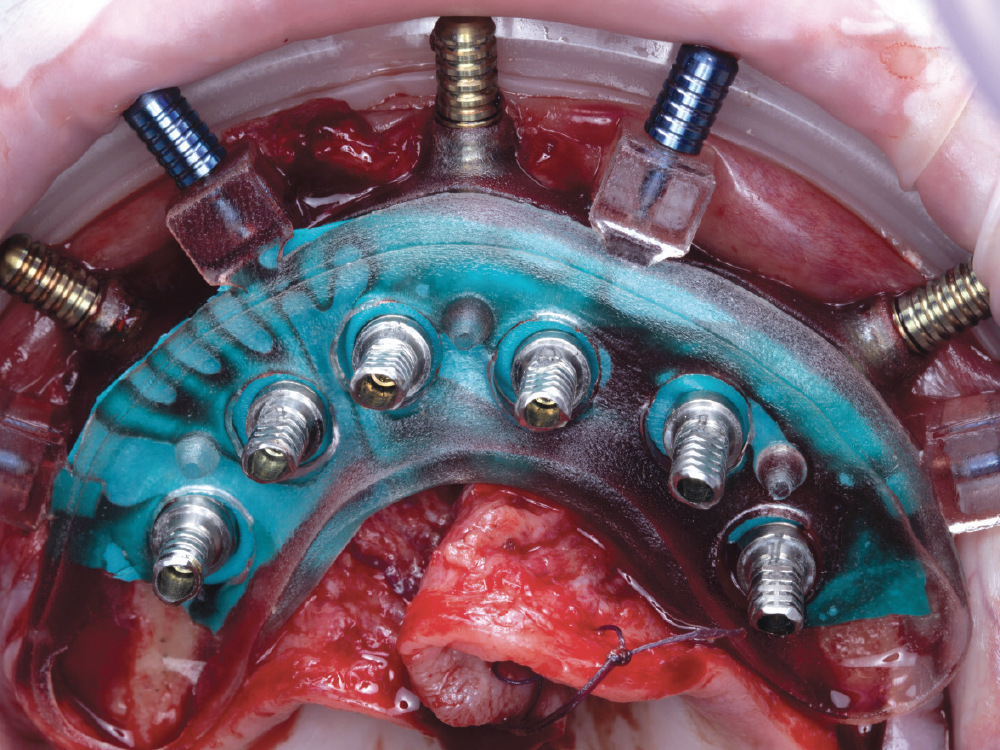
Implant Verification Prosthesis
The implant verification prosthesis (IVP) is connected to the titanium cylinders on the day of surgery and then kept by the restorative dentist. The IVP can be utilized when it is time to fabricate the definitive prosthesis.
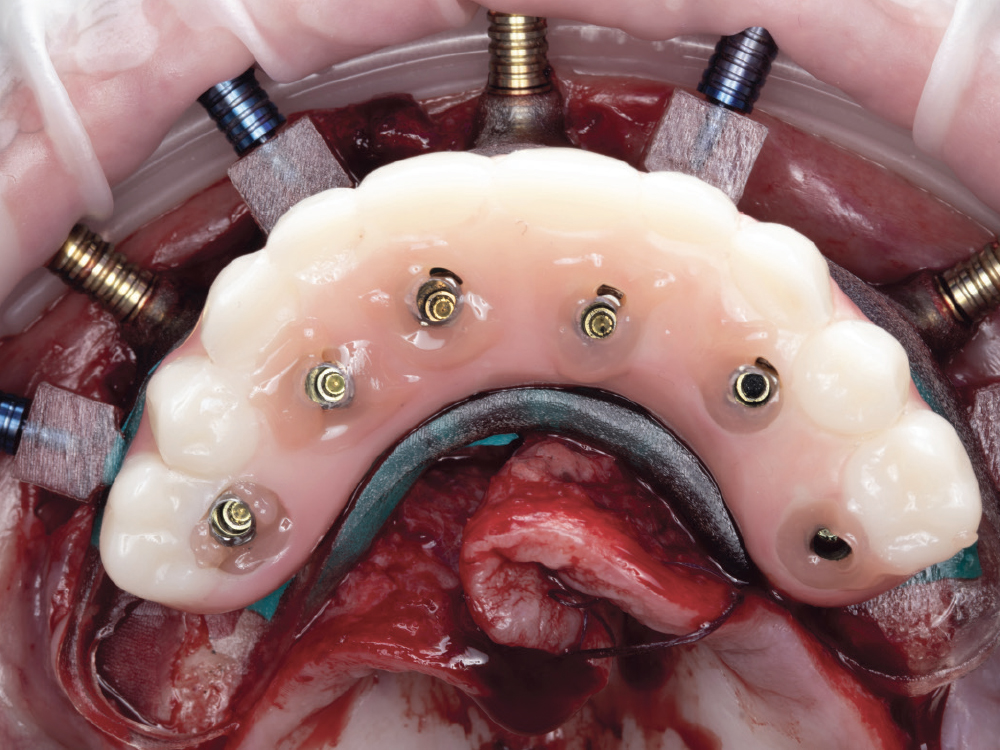
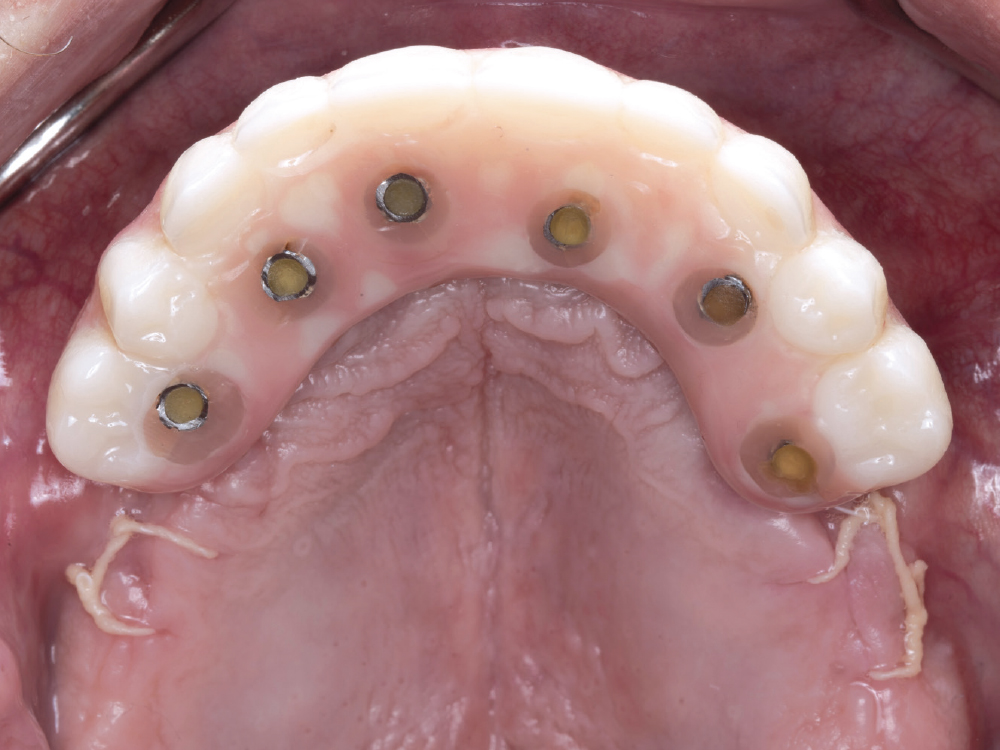
Immediate Fixed Screw-Retained Provisional Implant Prosthesis
The immediate provisional implant prosthesis is luted to the titanium cylinders on the day of surgery and delivered to the patient to wear until the implants are ready for fabrication of the definitive prosthesis.
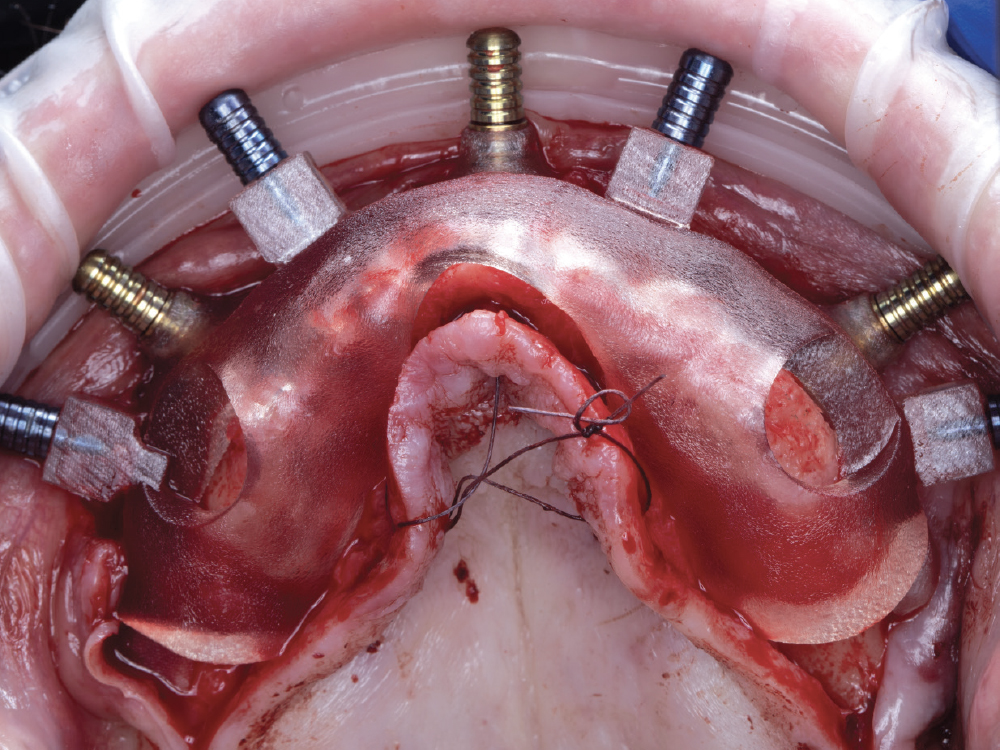
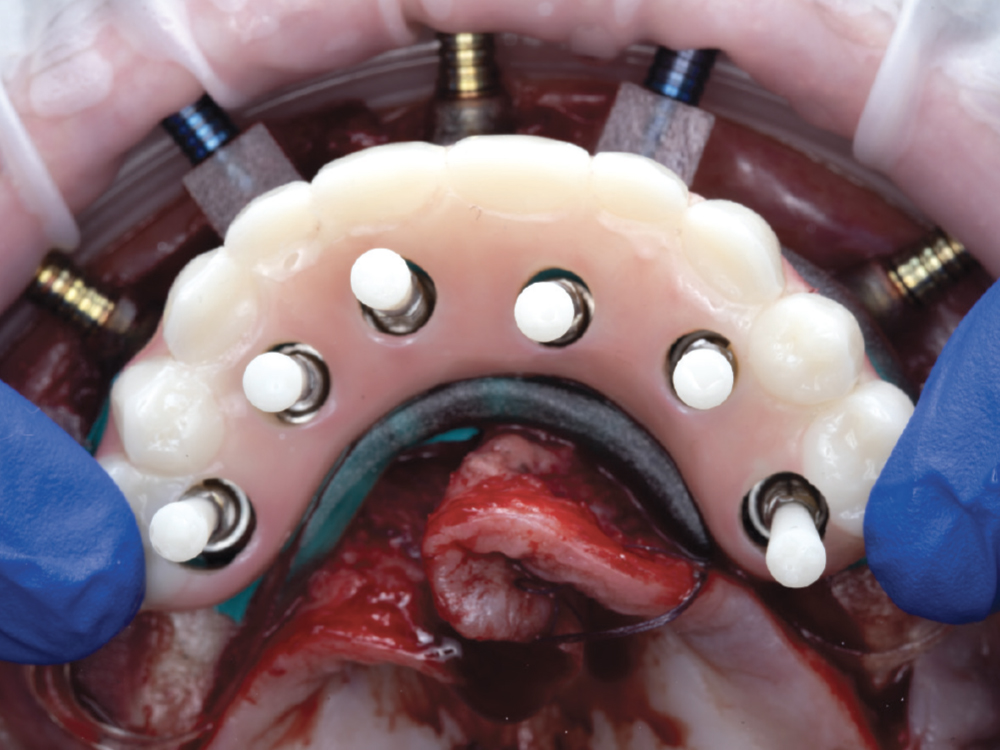
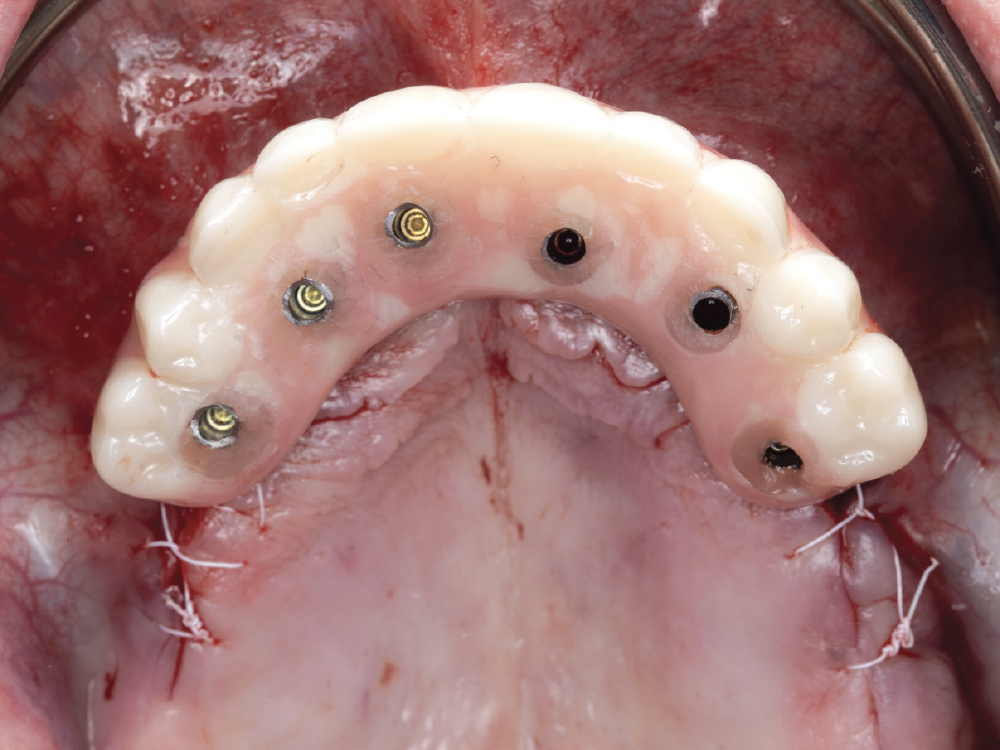
Temporary Cylinders
The temporary cylinders are connected to the multi-unit abutments and then luted to the immediate provisional implant prosthesis and implant verification prosthesis.
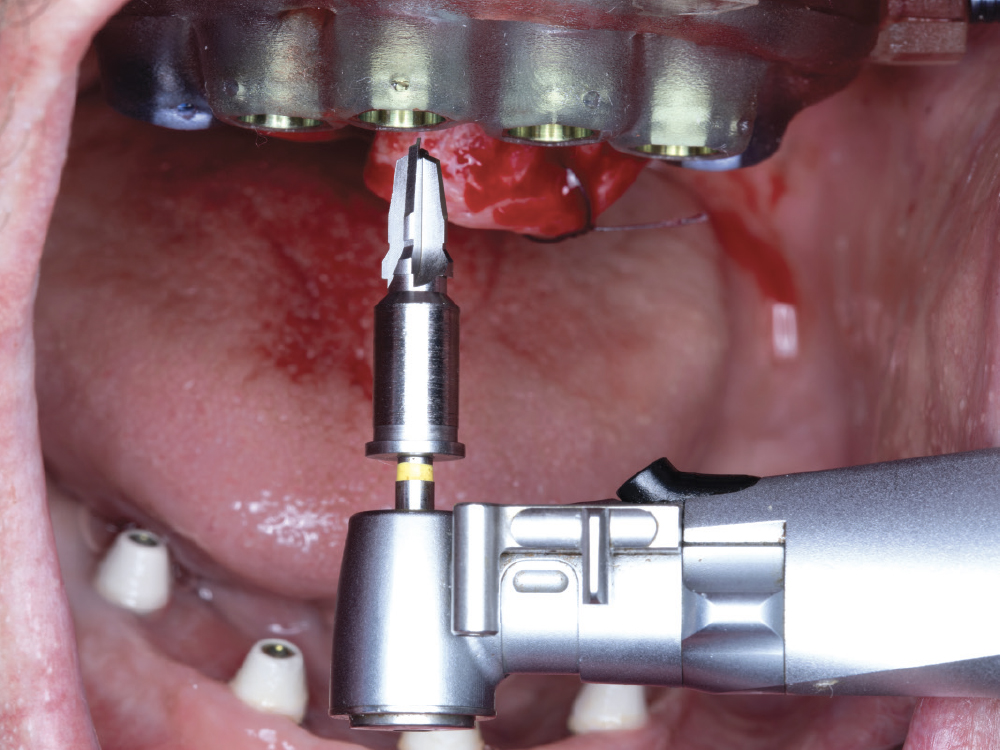
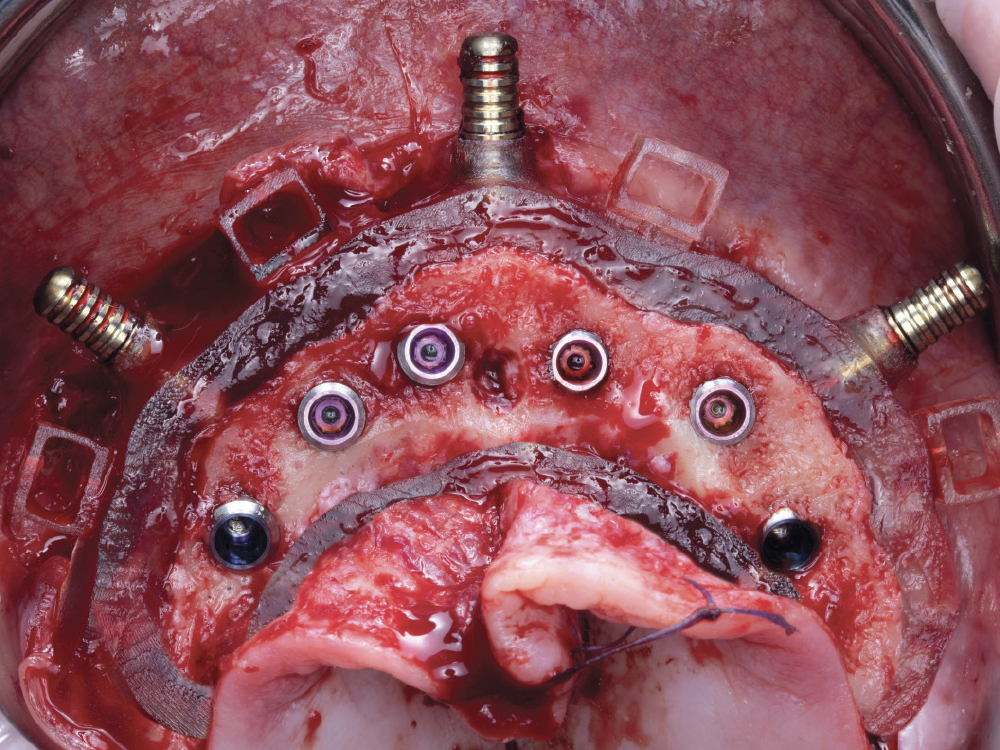
Multi-Unit Abutments
Available in straight or angled, 17 or 30 degrees, these abutments seat between the implants and the prosthesis. They allow for the correction of implant angulation to improve screw-access hole locations. They can assist in leveling the restorative platform for easier restoration design and soft-tissue maintenance.
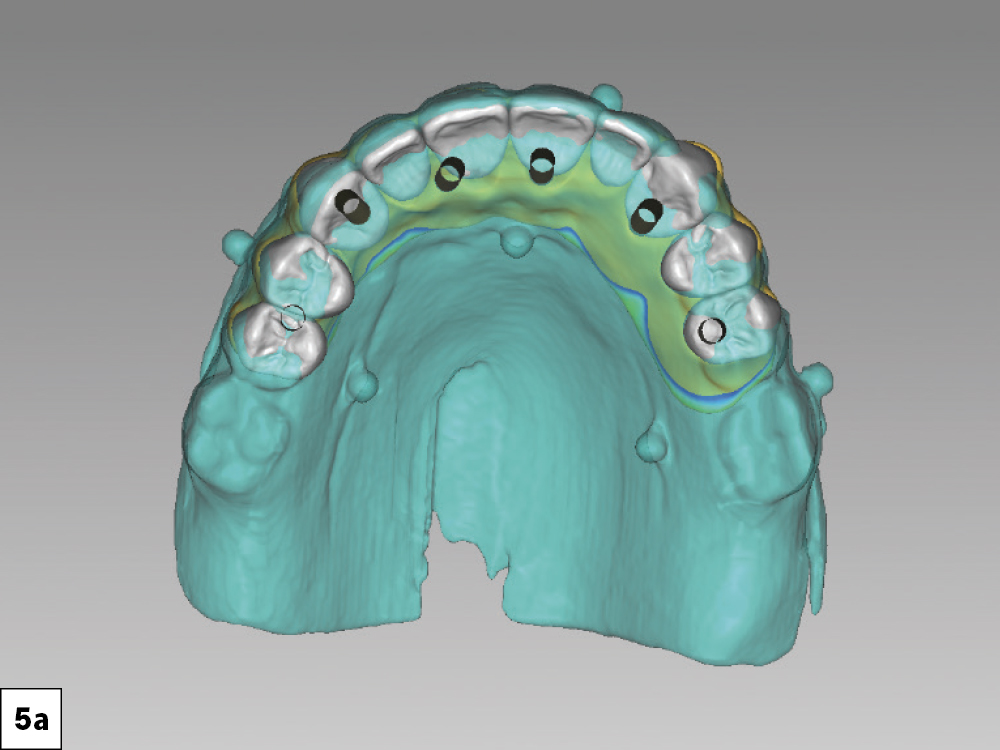
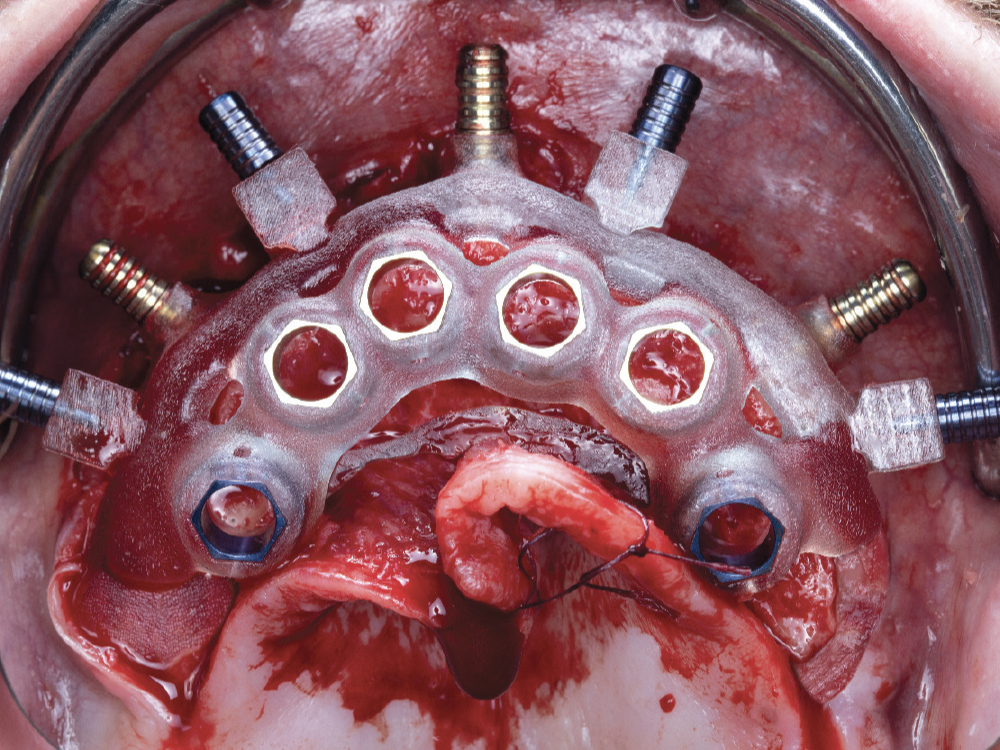
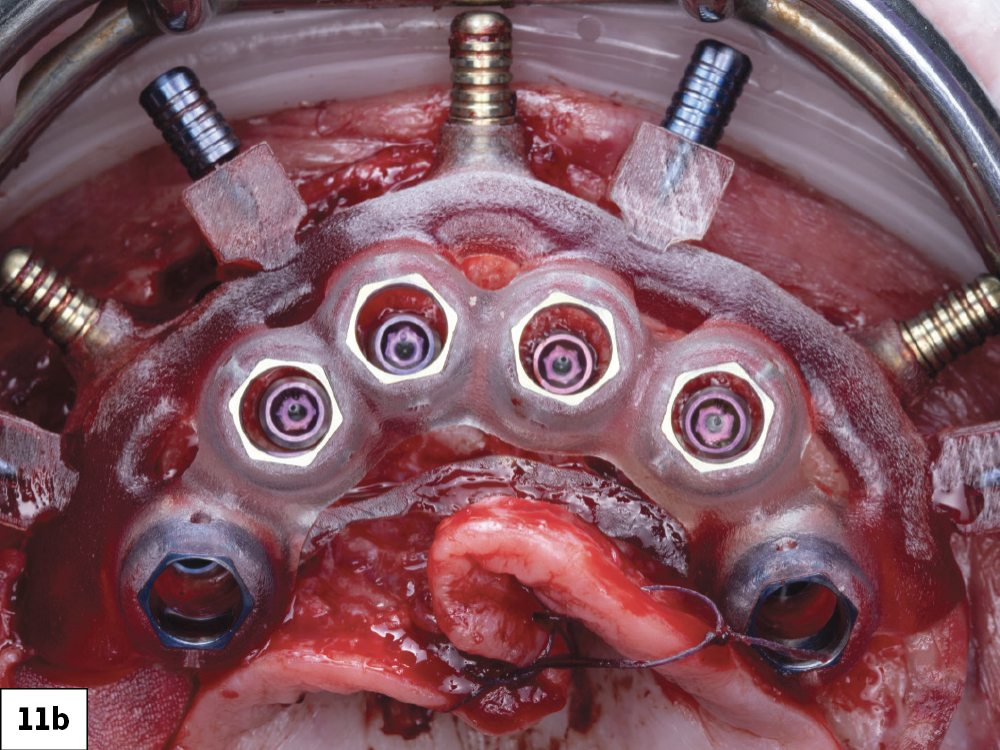
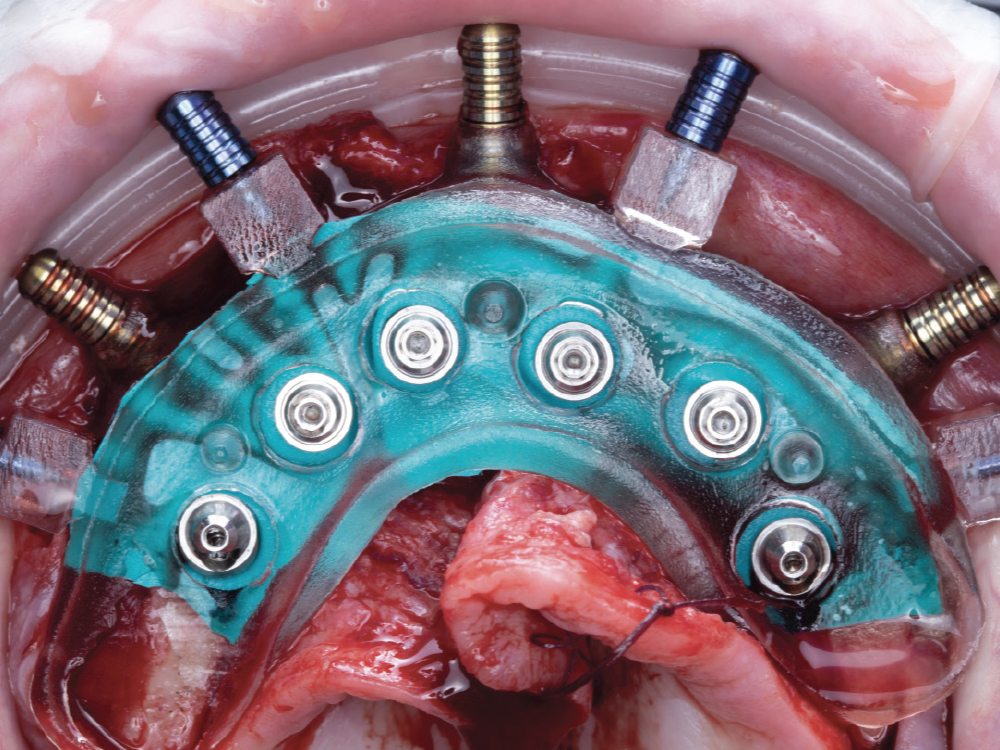
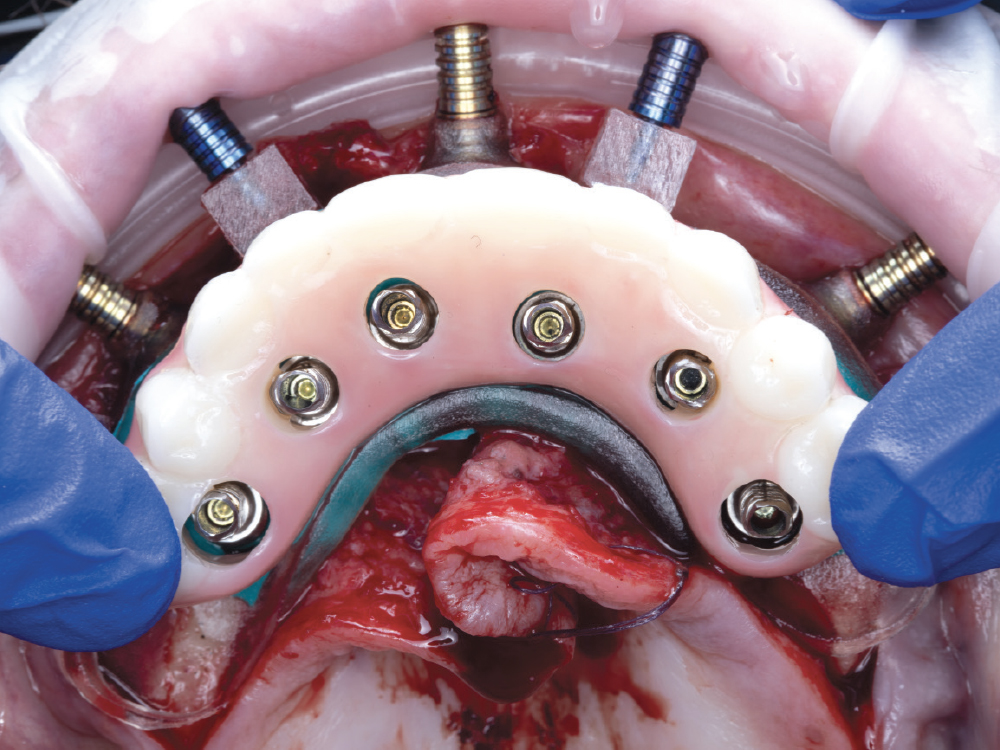
Prosthetic Delivery Guide
The prosthetic delivery guide has direction indicators for easy placement of multiunit abutments. The pegs on the delivery guide allow for the positioning of the immediate provisional prosthesis and the IVP.
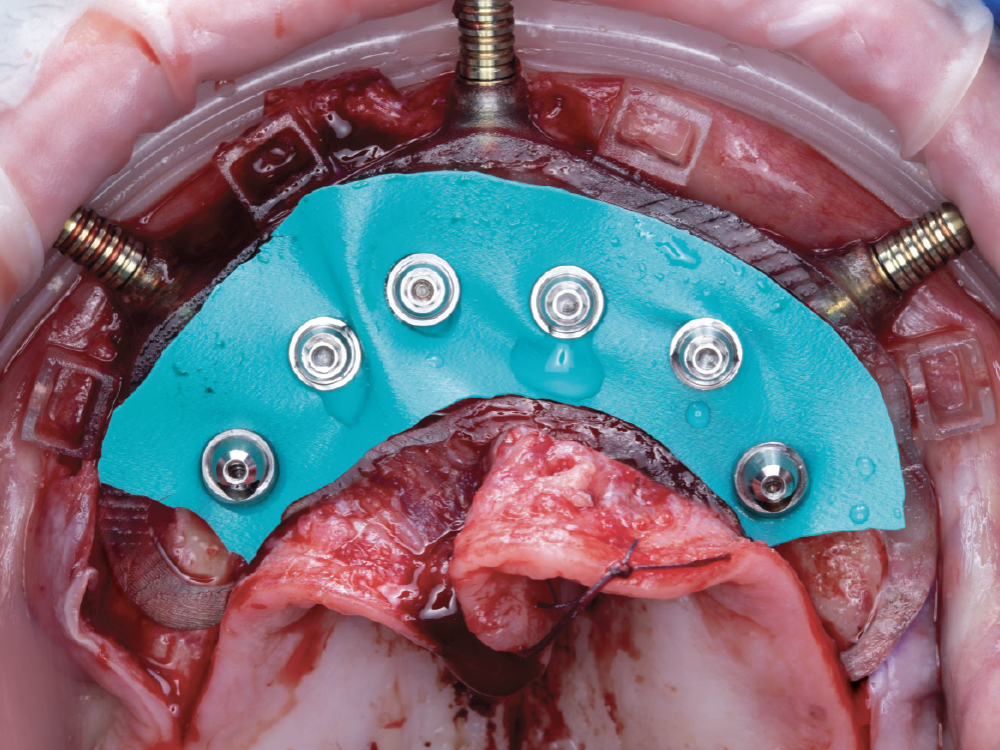
Custom Gasket for Relining Prostheses
The custom gasket is designed to fit snugly around each of the multi-unit abutments, laying underneath the prosthetic delivery guide. This gasket helps prevent the restorative pick-up material from contaminating the surgical site.
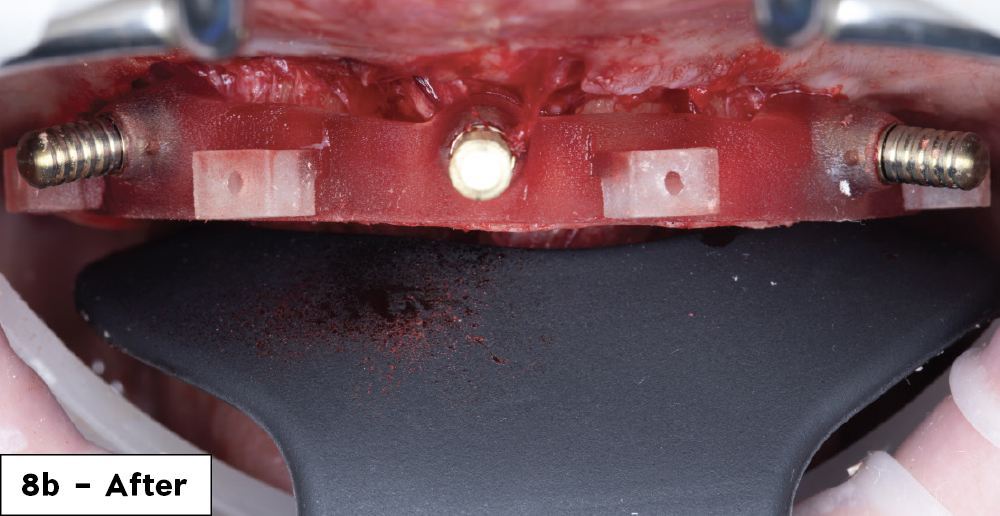
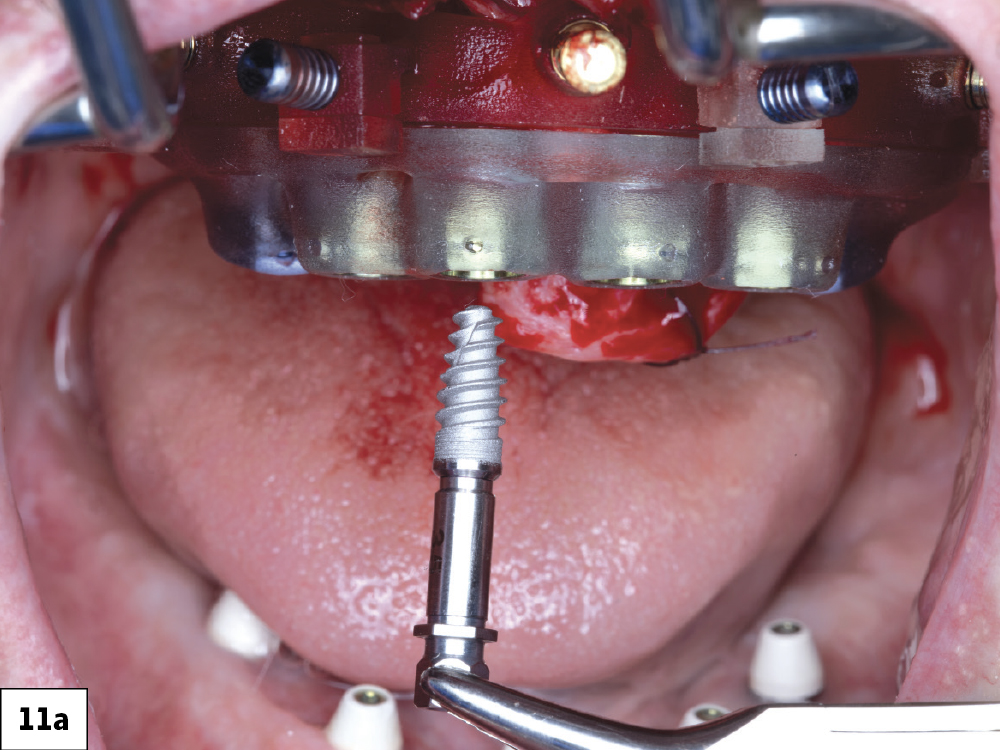
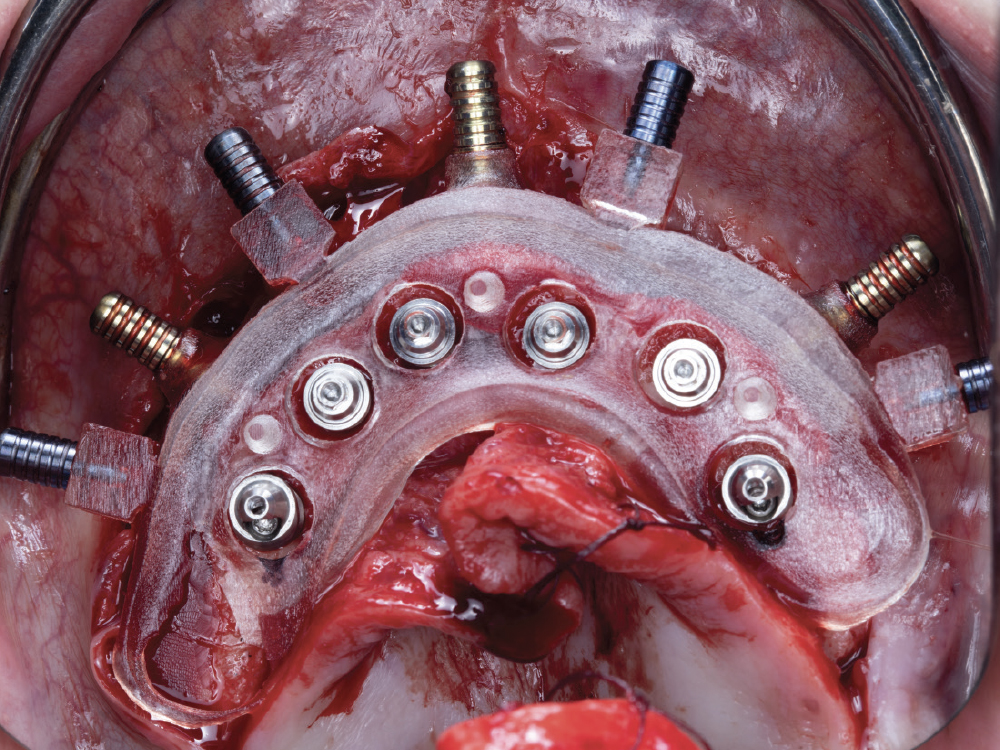
Osteotomy Guide
The osteotomy guide allows for the placement of the implants in the exact positions determined by the digital treatment plan. The guide is compatible with any implant system that utilizes a guided drill system.
Mounting Guide
The mounting guide allows for the placement of the foundation guide. Predesigned windows in the mounting guide allow for visualization of the underlying bone when securing the foundation guide in place.
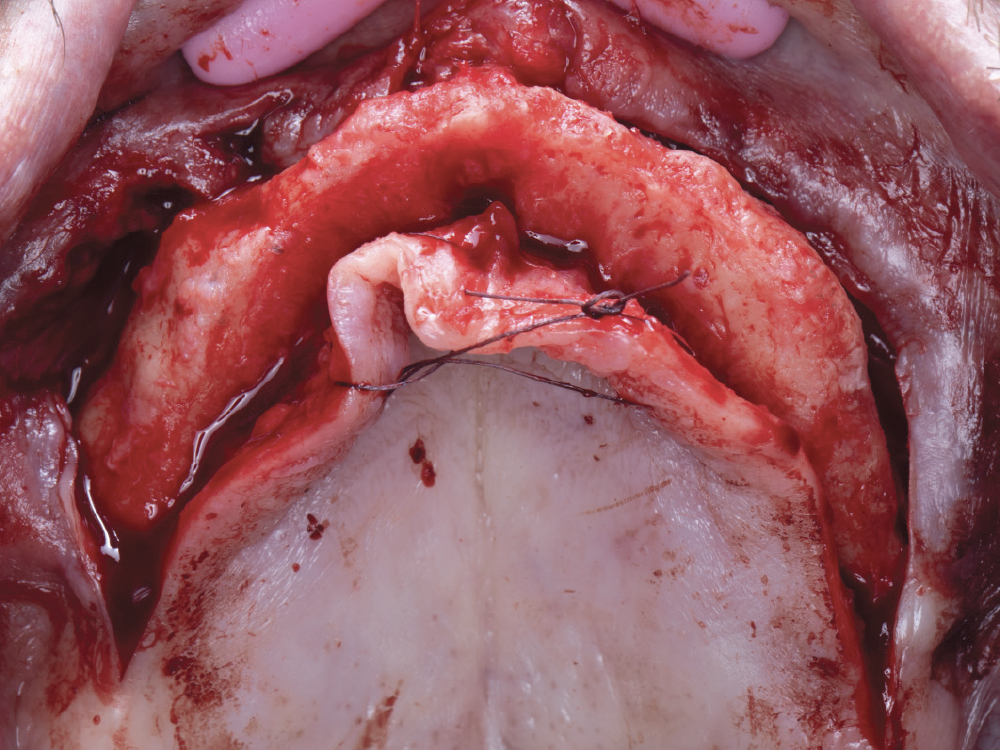
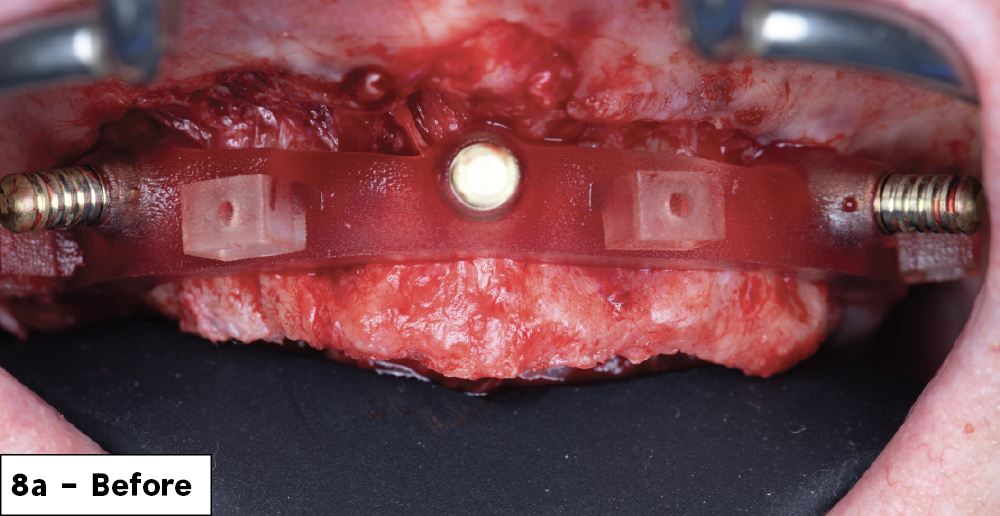
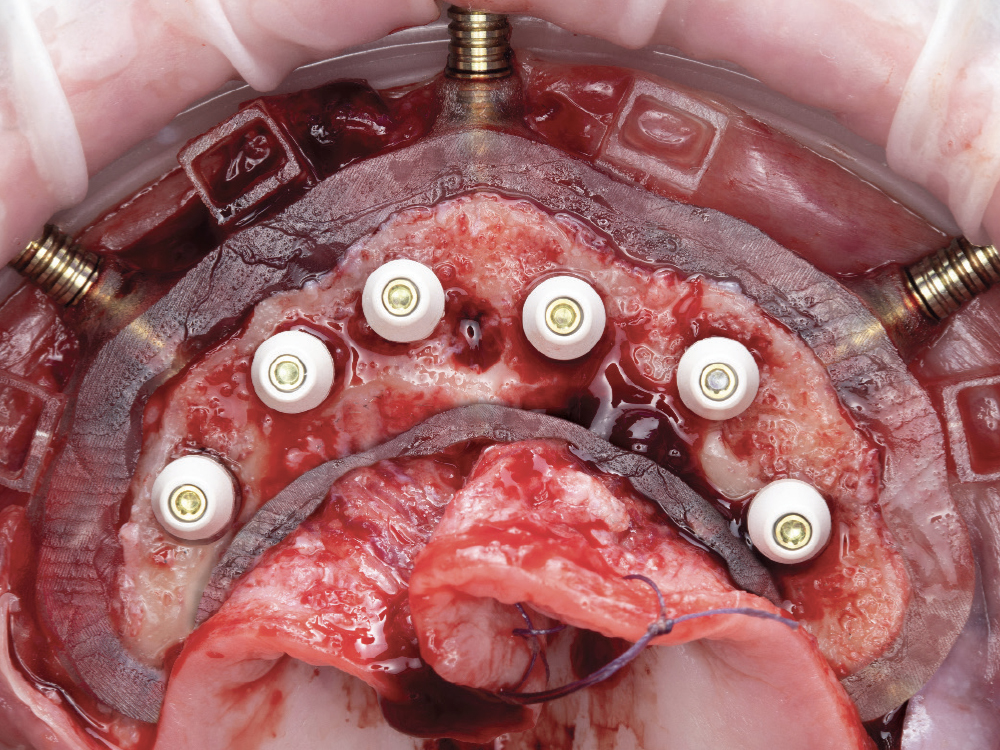
Foundation (Bone Reduction) Guide
This is the foundation for the surgery. It is delivered to the bone via a bone-supported mounting guide. It is the foundation upon which all the other guides will be seated. Once secured in place, the flat plane of the foundation guide is utilized to reduce the bone to the predetermined level.
Anchor Pins
A 1.5 mm diameter drill is utilized to create the osteotomies for the placement of anchor pins, which are then pushed into position to secure the foundation guide to the bone.
Interlocking Pins
These pins secure the multi-level components together. For ease of transition between the various multi-level componentry, the pins are manually placed and released. Floss holes are included on the handles for safety measures.
3D-Printed Segmented Bone Reduction Model
This model demonstrates the planned bone reduction.
3D-Printed Model
This model demonstrates the bony anatomy of the arch being treated and the post-bone reduction implant placement.
Note: Surgical guides are customized for individual patients
FOUNDATION GUIDE
The multi-level surgical guide is a “stackable” approach to full-arch implant surgery and immediate loading.
OSTEOTOMY GUIDE
NOTE: Based on the stability of the implant and our plan for prosthetic loading, we select one of the following component options:
- Cover screw (hand-tighten)
- Healing abutment (hand-tighten)
- Multi-unit abutments (implant manufacturer’s recommended torque value)
PROSTHETIC DELIVERY GUIDE
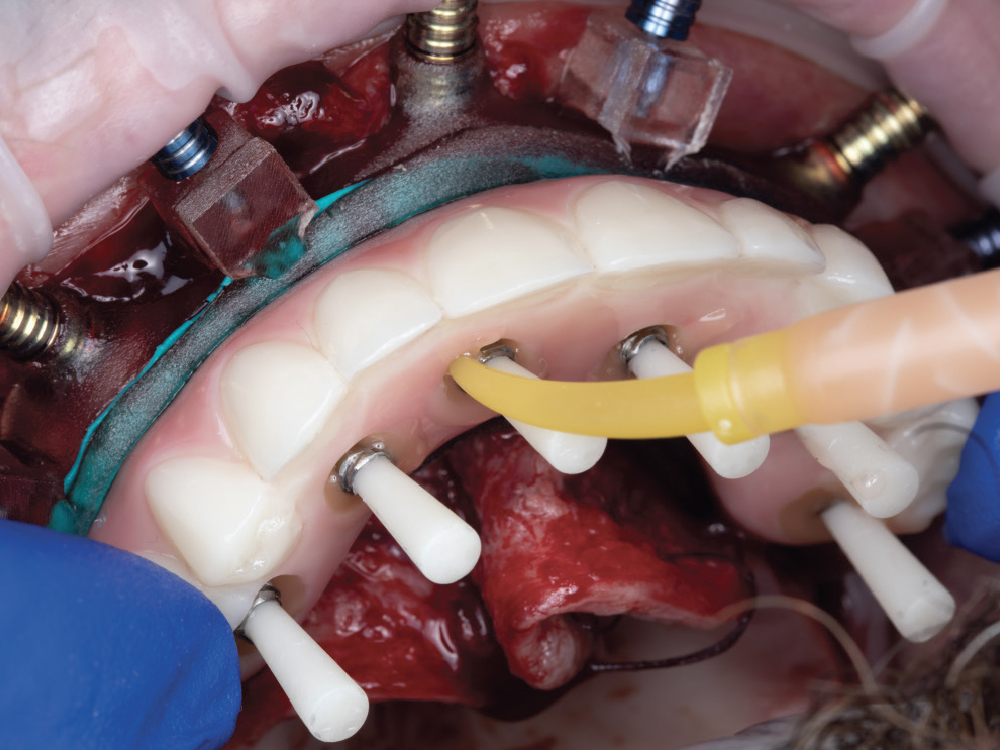
NOTE: Complete the conversion process by performing the following steps with the provisional implant prosthesis outside of the patient’s mouth:
- Cut cylinders if necessary
- Fill in voids with composite or pickup acrylic
- Adjust and polish the prosthesis
If an implant verification prosthesis was also provided for your case, repeat the above steps for it.
DELIVERY OF PROVISIONAL IMPLANT PROSTHESIS
CONCLUSION
Advanced procedures like the immediate loading of implants for a fixed full-arch restoration are becoming more predictable with advances in technology. Prosthetically driven guided implant placement allows for optimal restorative outcomes. The multi-level surgical guide will allow you to take your implant practice to the next level, aiding in both surgical and prosthetic predictability.