Getting Paid for Sleep Therapy: Do You Need to Bill Medical Insurance?

Dentists treat sleep-related breathing disorders because of a strong desire to help patients prevent the negative health consequences associated with these conditions. The challenge, however, has been the complexity of obtaining reimbursement for these services. Dental insurance doesn’t cover sleep appliances — and billing medical insurance is difficult and expensive. It’s difficult because it pays dentists only after patients have received a definitive diagnosis of sleep apnea from their physician, and it’s expensive because working with a billing company reduces your profit margin.
Fortunately, dentists don’t need to accept medical insurance to become involved in treating sleep-related breathing disorders. If you have a desire to treat snoring and sleep apnea, the “win-win-win” billing method is a strategy that can ensure victory.
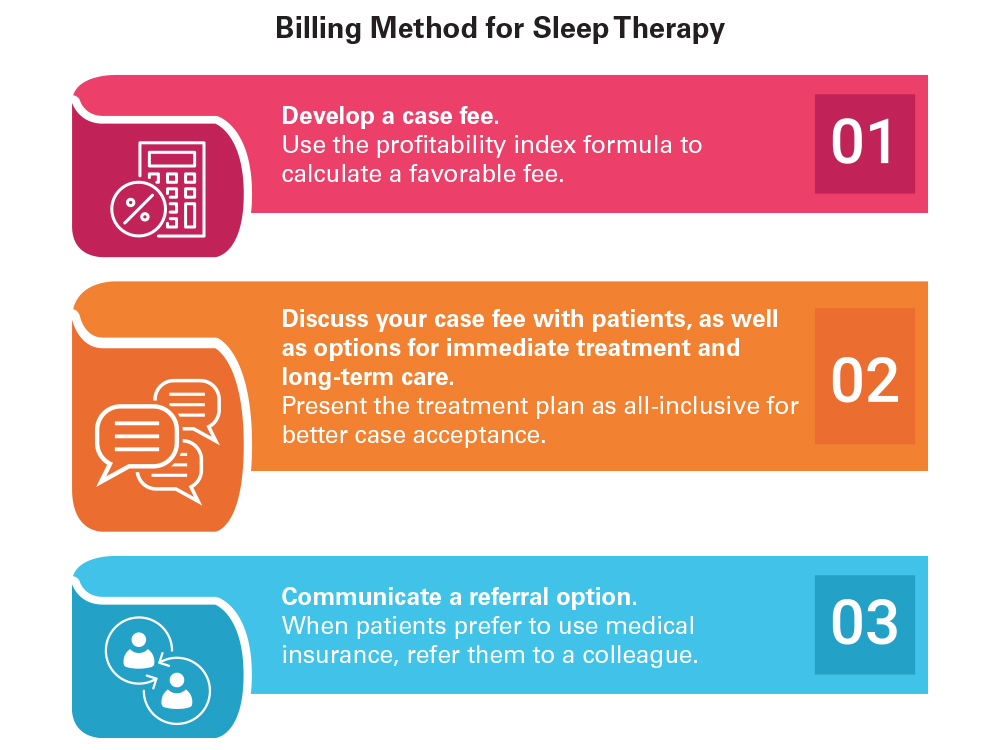
WIN-WIN-WIN BILLING METHOD
Step 1: Develop a case fee.
To determine your rate for providing oral appliance therapy, you must account for multiple factors, such as how much capacity you have (available chair time and staff), your skill and expertise, and the skill and expertise of your staff. Evaluation, treatment planning, fitting and follow-up will all take longer in the beginning. The fee will depend on appliance selection and the associated costs. Appliance choice will vary from patient to patient — there is no one-size-fits-all appliance. The fee will also depend on the ability for the office to use telemedicine appointments for follow-up, which reduces needed chair time and makes chair time more productive.
To determine your fee, do not use a formula such as “three to five times the cost of the lab bill.” This may work fine for many procedures, but not for sleep therapy, which is follow-up intensive and therefore chair-time intensive. This chair time is not typically related to physical adjustments of the appliance, but is rather the time required to discuss with patients how they are responding to therapy and what, if any, side effects they are experiencing. Time is also needed for decision-making by the dentist and staff regarding next steps. Handling follow-up via telemedicine can make these visits much more efficient.

Treating patients for sleep-related breathing disorders involves developing a case fee that’s both affordable for patients and profitable for the clinician.
Gauging profitability
For most dentists, an all-inclusive fee in the $1,800 to $3,200 range would be appropriate. Some dentists may decide to charge less as they are starting out because they recognize that they are “paying for their education.” Dentists may use the profitability index formula to evaluate their profitability and create their case fee. See Table 1.
Table 1: Profitability Index Formula and Case Example Profitability index (PI) = Your case fee – Your lab bill / Number of patient visits for the case
Case Example: A dentist has a case fee of $1,800. The EMA® appliance at the cost of $217 is an excellent choice for this specific patient. Treatment goes smoothly, requiring only two follow-up visits after the initial fitting, for a total of three visits.
PI = ($1,800 – $217) / 3 = $528 per visit
In most states, dentists can delegate the fitting and follow-up adjustments to well-trained staff members, resulting in very little chair time for the dentist. In addition, many follow-up visits can be conducted using telemedicine, further reducing required chair time.
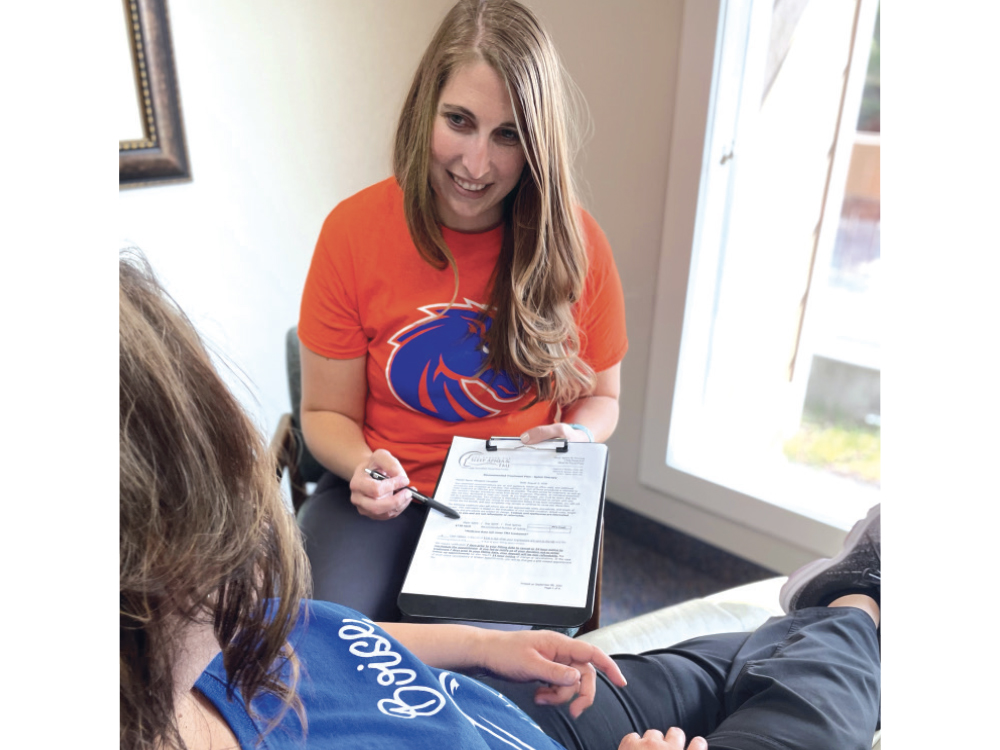
With dental sleep therapy, fitting and follow-up appointments can often be delegated to knowledgeable staff members, reducing chair time for dentists.
Step 2: Discuss your case fee with patients, as well as options for immediate treatment and long-term care.
Ensure that your patients completely understand what you can and can’t do for them. Explain that the case fee is all-inclusive, just like it would be with orthodontics — a useful example because most people know approximately how much braces cost in their area. As such, when your case fee is presented and it is less than orthodontics, patients will feel it’s appropriate, and they may not be surprised.
Provisional mandibular advancement device (PMAD) therapy provides an option for the patient to get started immediately and use the outcomes of therapy as part of the decision-making process for moving forward with further diagnosis and treatment, working in conjunction with their primary care physician.
In the PMAD model, the provisional aspect of therapy may be presented as a portion of the case fee. If long-term care is indicated, then the rest of the case fee would be charged. The following is an example situation:
- Case example — The dentist’s case fee is $1,800 for PMAD therapy. The patient receives the physician’s definitive diagnosis of sleep apnea. The dentist uses what was learned from provisional therapy (i.e., mandibular position, including vertical) to prescribe a new appliance. This treatment plan is an additional $1,000 and includes the necessary follow-up.
The EMA device and Silent Nite® Sleep Appliance, which are both available from Glidewell, are excellent choices for the PMAD model for the following reasons:
- Comfort — They are thin and comfortable for the patient to wear. Compliance is the key to success with oral appliance therapy. Starting with a custom appliance that is small and easy to use helps set the patient up for success.
- Adjustment style — The straps or connectors, and thus the mandibular position, are prescribed by the dentist. When only the straps appropriate to that stage of therapy are given to the patient, this eliminates the risk of the patient being lost to follow-up and adjusting their appliance farther and farther forward, which may lead to significant side effects.
- Long-term success — Both the Silent Nite and EMA appliances may also be used long term and are affordable enough that a patient could have several appliances (e.g., one for home and one for their travel bag). Additional cost savings are provided when two appliances are prescribed at the same time with the Glidewell Clinical Twinpak™.

The Silent Nite Sleep Appliance is an excellent choice for the PMAD model due to its comfort, connector adjustment style, and affordability. The Glidewell Clinical Twinpak enables two appliances to be prescribed at the same time at a special discounted price.
Step 3: Communicate a referral option.
Let patients know that if they receive their physician’s diagnosis of sleep apnea, a portion of the oral appliance therapy may be covered by their medical insurance — and if cost is most important, because you don’t work with medical insurance, you would be happy to refer them to a colleague who does.
Because of escalating deductibles, many patients would have to pay a significant amount out-of-pocket anyway, so they will be more likely to stay with their trusted family dentist. However, when cost is the determining factor, patients will appreciate your referral, which builds more trust that you are looking out for their well-being and financial situation.
EMPLOYING THE WINNING STRATEGY
For most dentists, medical billing is the main obstacle as they try to start helping patients with snoring and sleep apnea problems. The win-win-win billing method allows you to start without having to deal with extra hassles, and you can refer patients to dentists who are in-network if that is the patient’s desire. This method is a practice builder, as it allows patients to start provisional therapy immediately, connects you to primary care doctors who may become referral sources, and strengthens the relationship of trust between you and your patients. With this strategy, everyone wins, including patients. You and your team also win, as helping people sleep better — which improves overall health and quality of life — is one of the most rewarding things healthcare professionals can do.
EMA is a registered trademark of Frantz Design Inc.

With the win-win-win billing method, dentists can provide sleep therapy without having to deal with the extra hassles of medical insurance.