5 Ways to Prevent Medicolegal Complications

The best way to handle legal problems in your practice is to take measures designed to prevent them. Based on my 30 years of dealing with the legal issues that often plague dental practitioners, I have developed these guidelines to follow that will help you avoid becoming ensnared in the legal system. Follow these five ways to prevent medicolegal complications from occurring in your practice.
1. DON’T IGNORE TREATMENT COMPLICATIONS
A less-than-ideal outcome doesn’t necessarily mean that you violated the standard of care. But failing to address complications or concerns during treatment can set you up for liability if a permanent injury results. Adopt a mindset that will objectively reflect your situation. Take a step back and think things through before jumping to the next phase. If you have the chance to fix the problem but don’t, you may be considered liable.
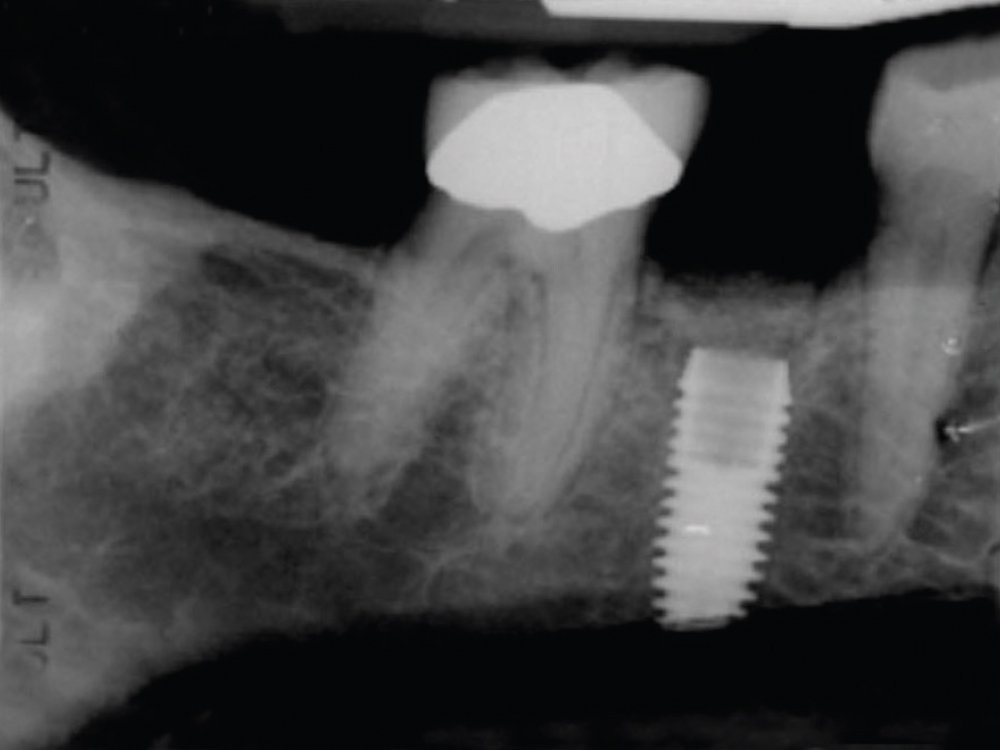
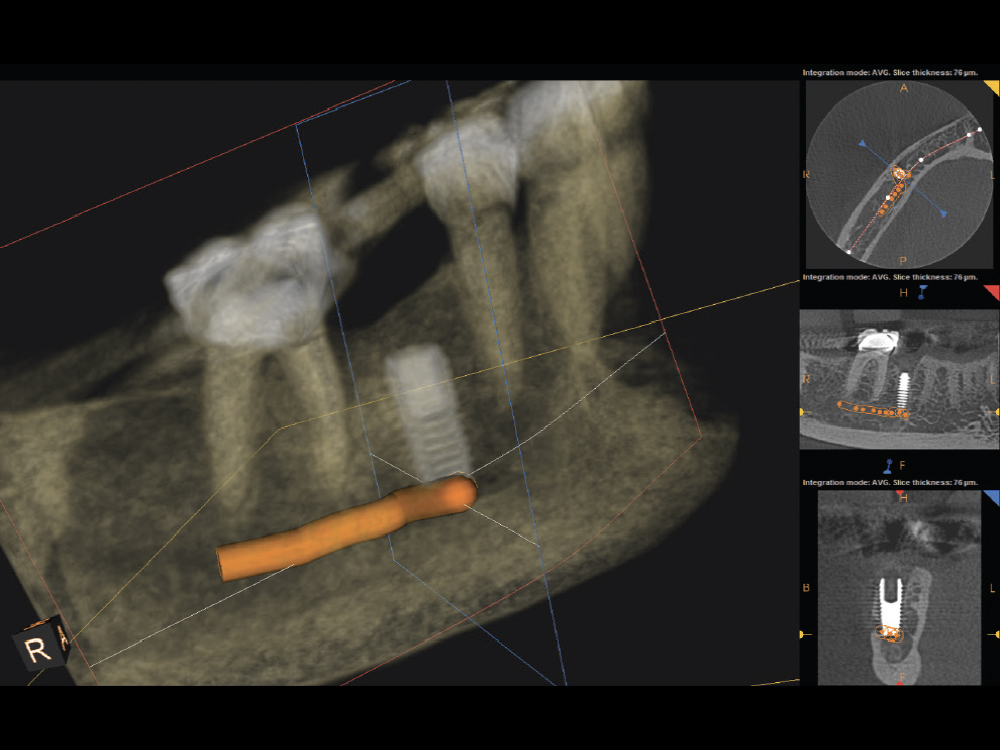
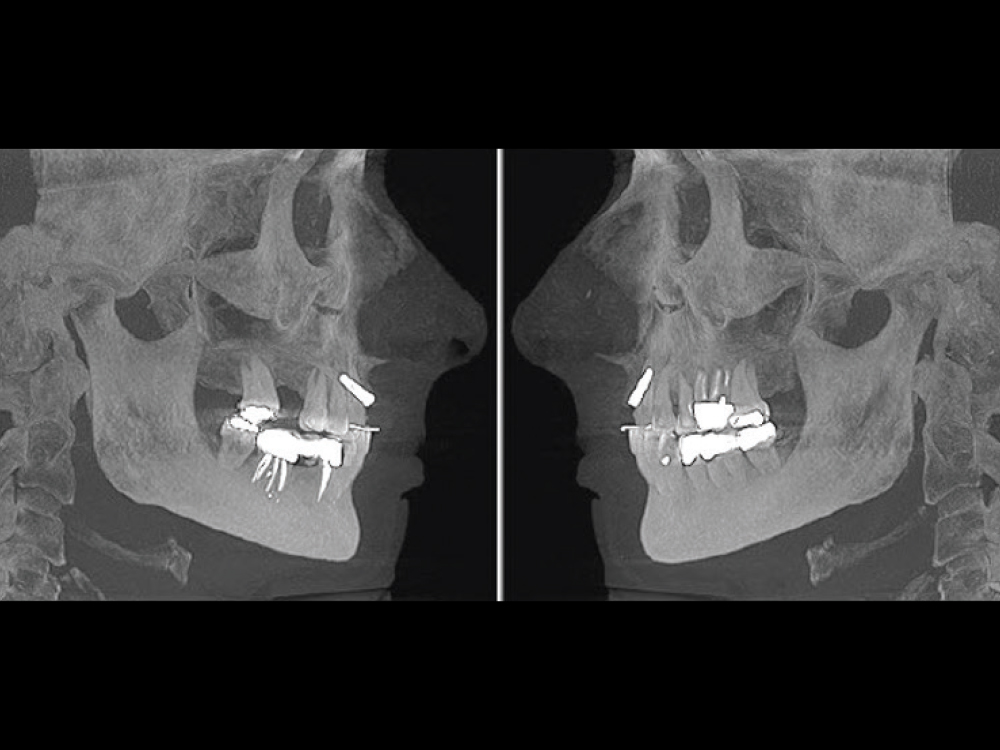
A doctor who places an implant in the mandible based only on a periapical radiograph runs the risk of injuring the inferior alveolar nerve. In this case, the patient returned a week later with paresthesia, and a CBCT scan showed that the implant invaded the inferior alveolar canal, most likely engaging the nerve. This could have been avoided had the doctor insisted on taking the necessary and appropriate scans before proceeding.
2. COMMUNICATE WITH YOUR PATIENT
Honest communication is key. When a dental complication occurs, do not place blame on the patient or tell them that you’re uncertain how to proceed. Rather, you can reassure the patient by explaining that you would like the opportunity to do a bit of research and call one of your colleagues before proceeding. Inform the patient that you want to work with them to achieve a successful resolution together. Present your patient with something that moves the situation forward and demonstrates that you are actively working toward a better outcome for them. Do not ignore the patient.
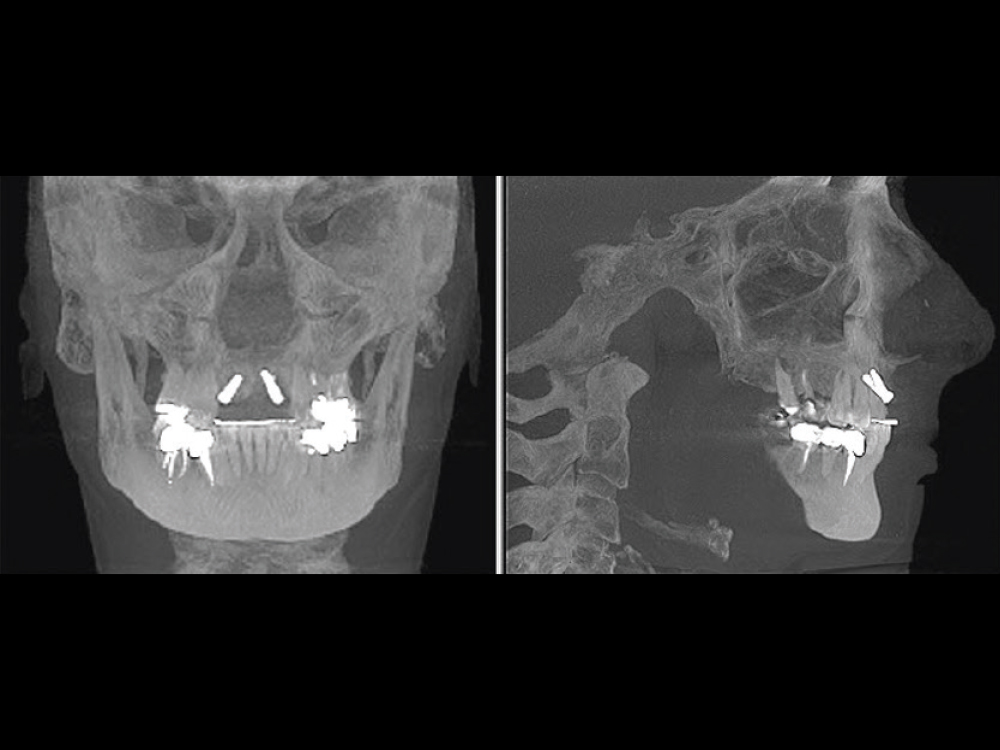

This patient received two implants for edentulous sites in the upper anterior. Instead of communicating to the patient that the implant platforms were exposed, the doctor sent the patient home without addressing the issue and was later sued for negligence. Litigation could have been easily avoided had the doctor advised the patient that the treatment plan had changed and that removal of the implants was now required.
Do not place blame on the patient or tell them that you’re uncertain how to proceed.
3. DON’T TAKE CASES YOU’RE UNCOMFORTABLE WITH
I’ve listened to numerous depositions with doctors who admit that they knew a case was going to be a problem from the start, and then went ahead with it regardless. It’s best not to get involved with a case if you’re unsure that your treatment can completely satisfy the patient. If you intuitively know from the beginning that a case isn’t what it appears to be, consider offering an alternative treatment plan or referring the patient to another doctor who may feel more comfortable taking it on. Difficult patients do not improve over time.
4. KEEP MEDICAL HISTORY CURRENT
Patients today are on more medications than ever before, making it important that you understand how their medical history can affect your treatment plan. Medical history forms will determine your path forward and often lead to a necessary medical clearance request from the patient’s primary care physician. When seeking medical clearance, tell the physician exactly what treatment you are planning to perform, including the anesthesia you’ll be administering to the patient. If the physician doesn’t respond to your request for medical clearance, tell the patient you can’t proceed. The physician’s failure to respond is not a green light for you to proceed. It’s important that this form as well as all medical history information stay current.
For more information on the importance of medical clearance, read Dr. Randolph Resnik’s articles “Medical Evaluation: Part 1 — Preoperative Evaluation of the Dental Implant Patient” in Chairside® magazine vol. 16, iss. 1, “Medical Evaluation: Part 2 — Systemic Disease and Oral Implants” in vol. 16, iss. 2, and “Medical Evaluation: Part 3 — The Influence of Systemic Medications.”
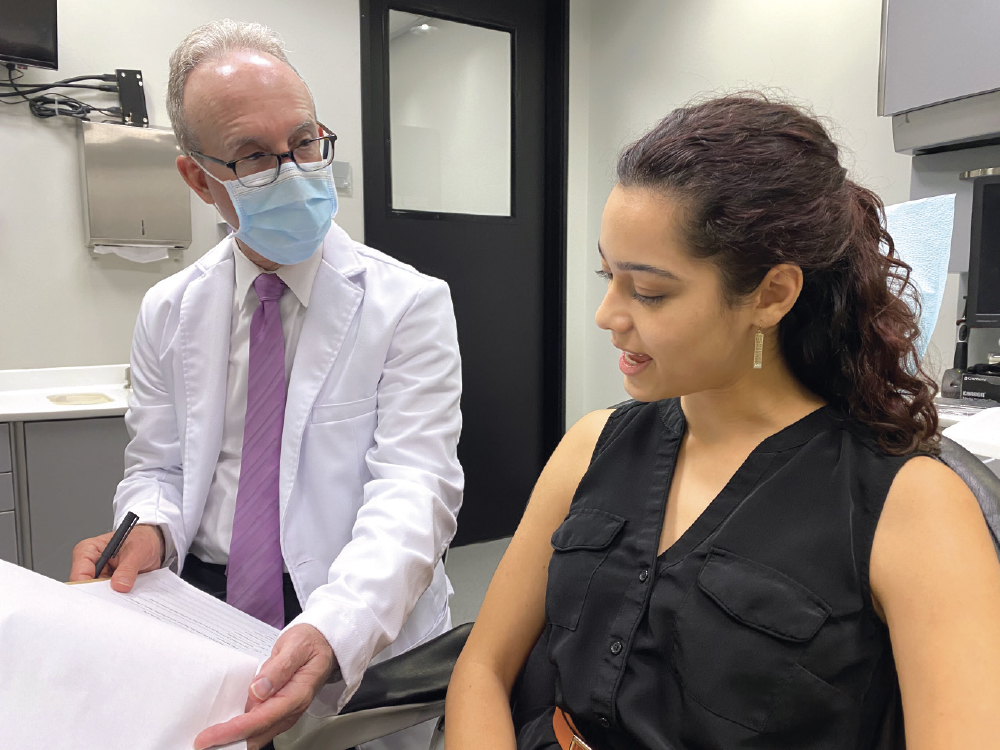
5. PROVIDE FACE-TO-FACE CONSENT AND GET SIGNATURES
I often see doctors who give their patients an informed consent document while the patient is already in the chair, prepared for surgery. Signed informed consent documents are vital in legal cases, but a specific discussion regarding the patient’s upcoming procedure is equally important. Give the patient the informed consent document as well as post-op instructions well in advance so they have the time to comprehend what they’re reading and ask questions. A chart entry should also be made when the documents are provided to the patient — for example, at the appointment prior to the surgical appointment. Sit down with them and ensure that they understand the treatment, including any potential complications. It is equally important to make a chart entry that states: “All risks, benefits and alternatives to the proposed treatment were discussed verbally with the patient, and the patient, having no questions, agreed to proceed.”
In over 30 years of practicing dental law, I’ve seen many legal cases that could have easily been prevented. Take the time to follow these five steps and work toward preventing medicolegal complications in your practice.