Buccal Roll Technique for Augmentation of Keratinized Tissue (1 CEU)
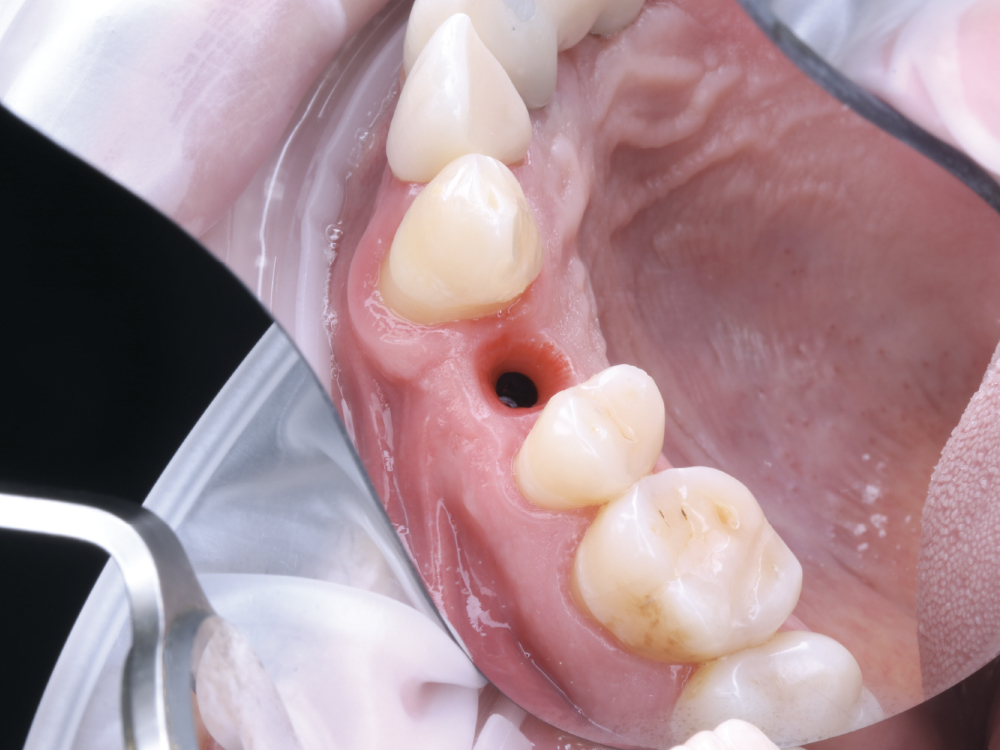
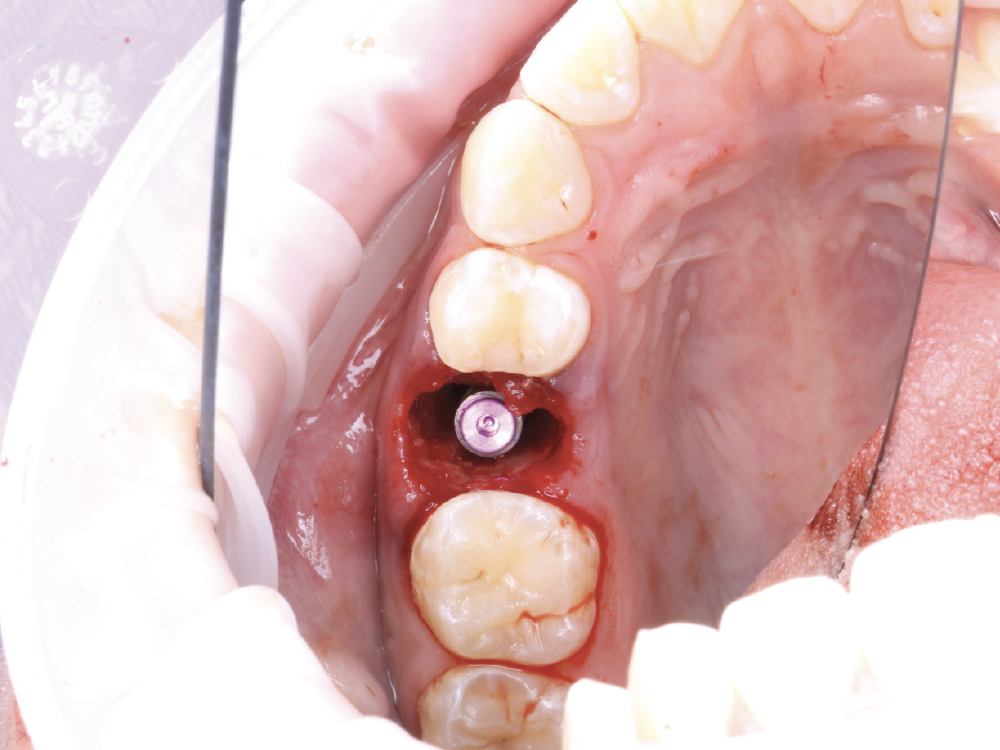
One of the most common questions asked by new implantologists is about when it is necessary to build keratinized tissue across the facial aspect of an implant. Generally, it’s recommended to have 3 mm of keratinized tissue occlusally (between the head of the implant and the top of the tissue), lingually, and buccally toward the mucogingival junction. This amount of tissue stability will ensure that the patient will not suffer loss of function around the implant site. If these conditions are not met after implant placement, surgical intervention is recommended.
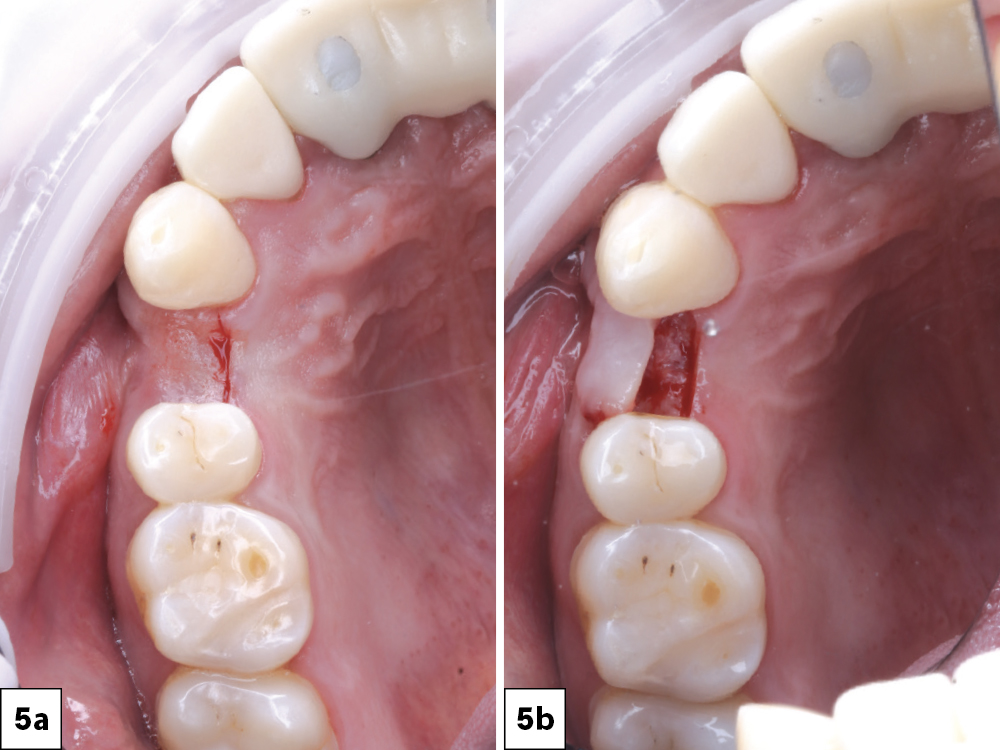
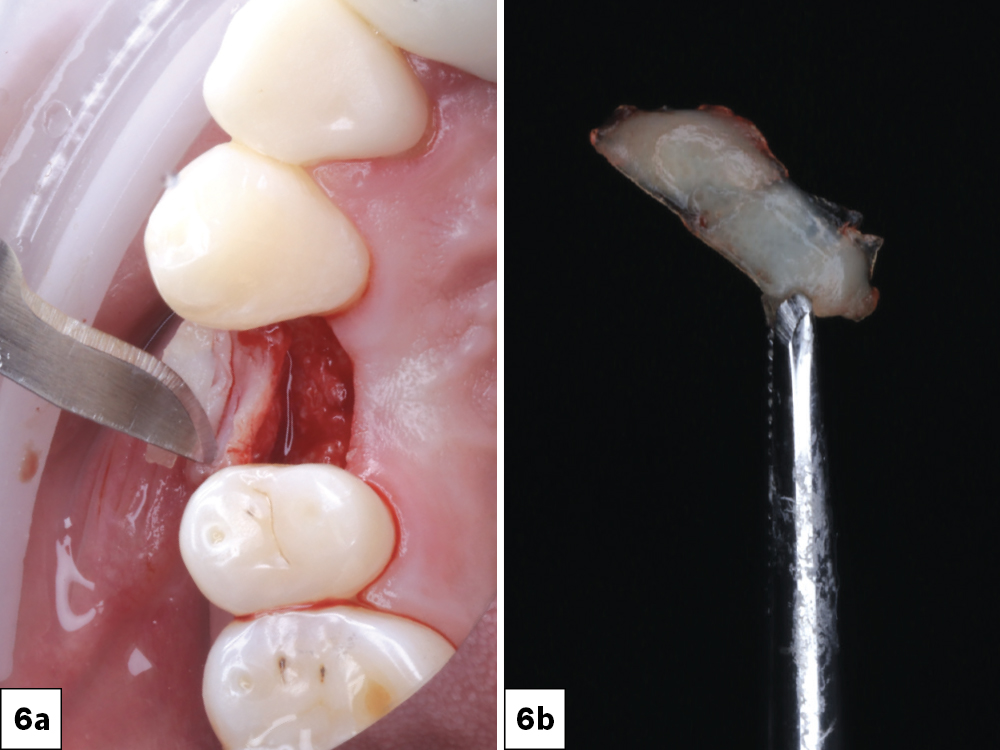
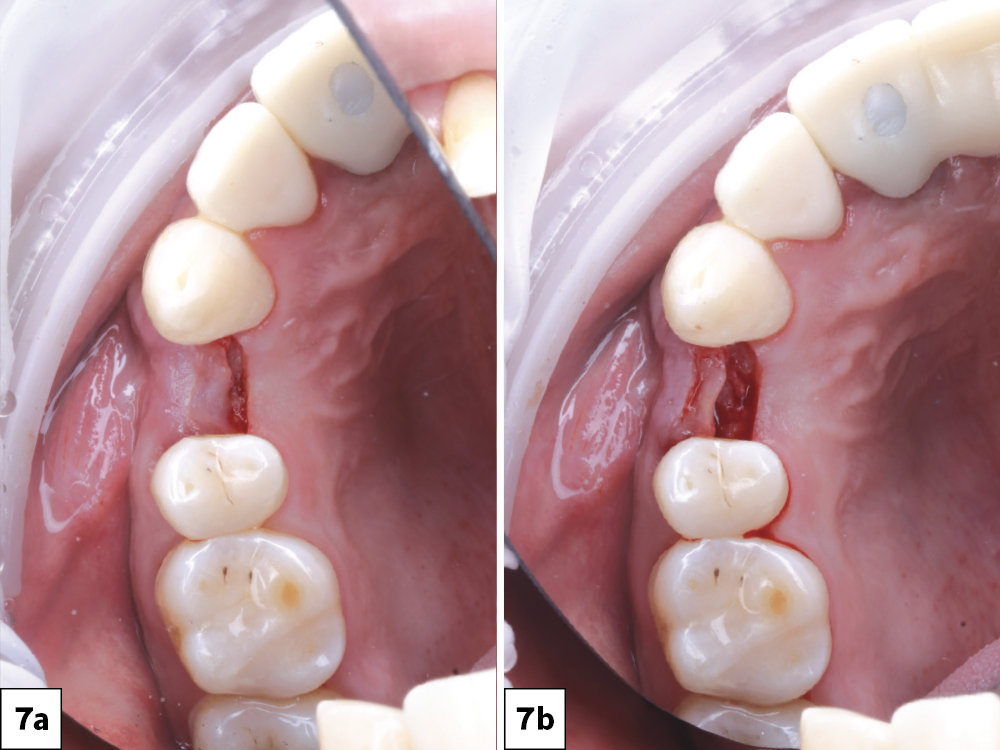
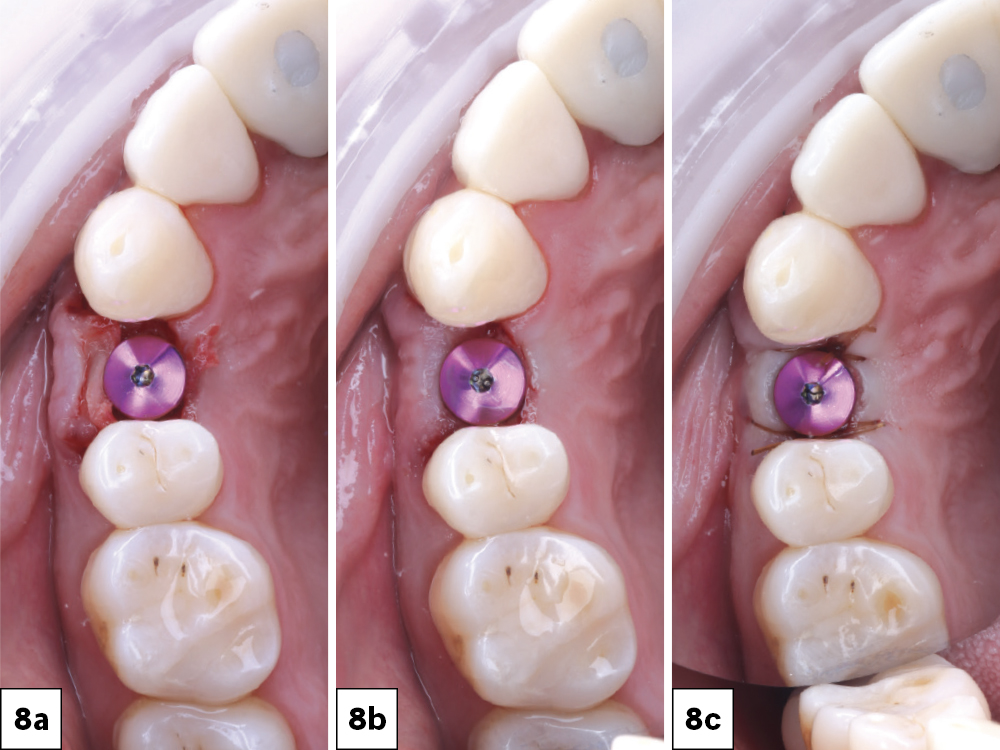
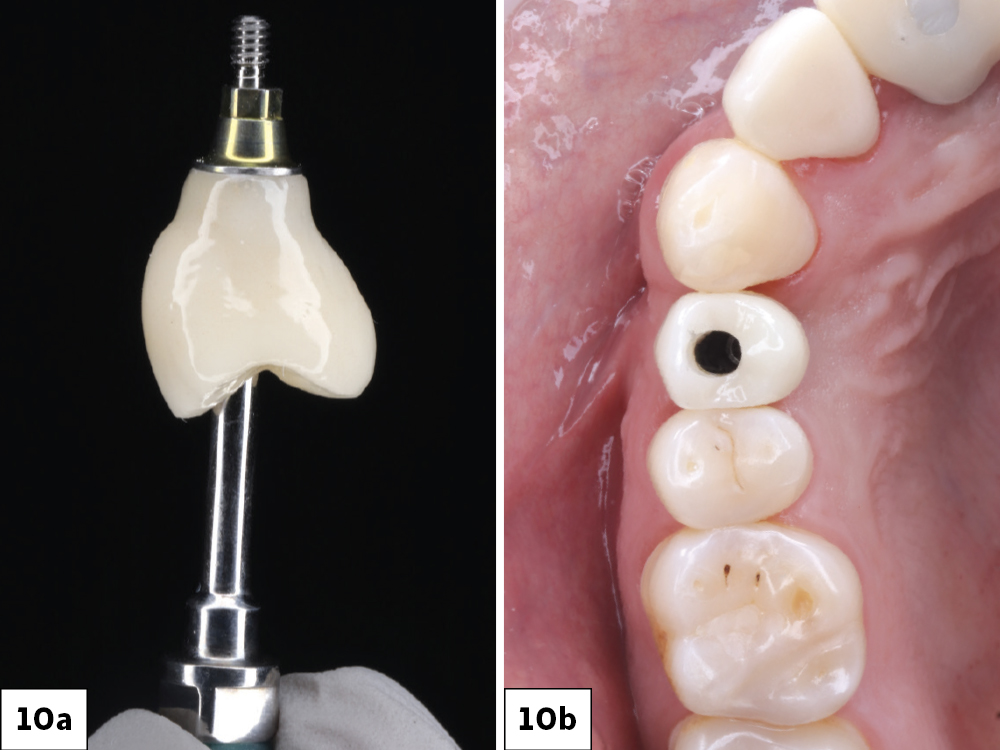
An effective way to build keratinized tissue on the facial is by using a modification of Abrams’ roll technique for localized alveolar ridge augmentation, or the buccal roll.1 This simple technique uses deepithelialized palatal tissue to fold underneath buccal mucosa and create the necessary amount of keratinized tissue for an ideal functional and esthetic outcome.2 This case study will demonstrate how to use this technique by analyzing a mandibular premolar that required an implant restoration.
CONCLUSION
Understanding how to perform the buccal roll technique to compensate for insufficient keratinized tissue is an important skill for doctors to have. Furthermore, being able to recognize the need for this procedure before delivery of the final crown will allow doctors to provide more efficient and cost-effective care.
Available CE Course
References
-
Scharf DR, Tarnow DP. Modified roll technique for localized alveolar ridge augmentation. Int J Periodontics Restorative Dent. 1992 Oct;12(5):415–25.
-
Saquib SA, Bhat MYS, Javali MA, Shamsuddin SV, Kader MA. Modified roll technique for soft tissue augmentation in prosthetic rehabilitation: a case report. Clin Pract. 2019 Mar 14;9(1):1110.