Implant Restorations: Screw-Retained vs. Cemented
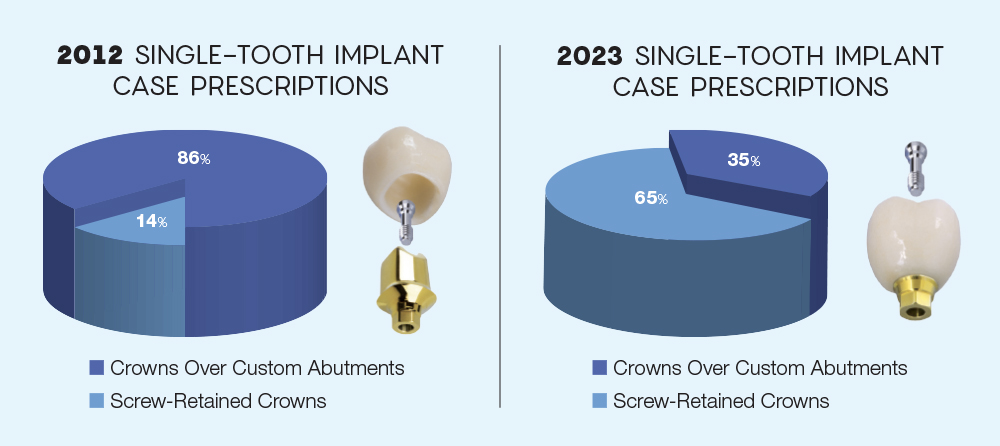
In recent years, there have been several reports and much discussion surrounding the role played by dental cements in the development of peri-implant mucositis and peri-implantitis.1,2,3 As a result, many dentists have changed their restorative procedures, resulting in a significant shift toward screw-retained restorations.
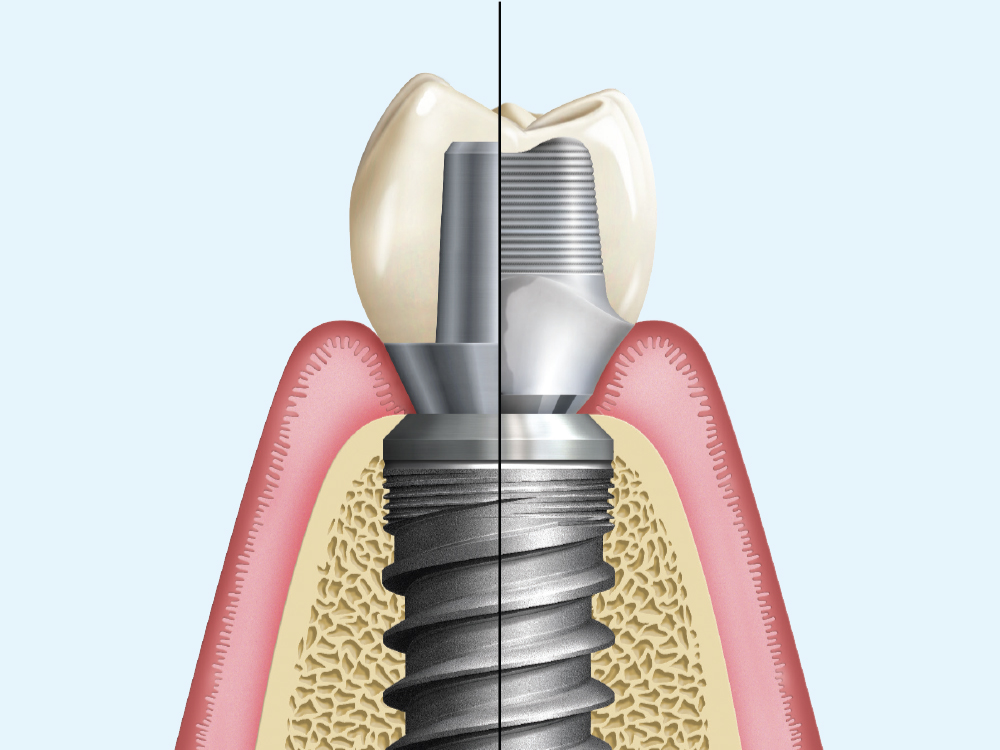
It is important to note that the cement itself is not the contributing factor toward peri-implant disease. More precisely, it is the excess cement that is allowed to remain around the restoration that acts as the nidus for soft tissue — and eventual hard tissue — disease. It should also be noted that in the early days of implant restoration, doctors routinely used stock abutments — universal abutments sold by implant manufacturers — that often placed restorative margins 5 mm or more below the soft-tissue crest. These deep margins made complete removal of excess cement virtually impossible, leading to the frequent occurrence of residual cement and subsequent tissue inflammation.
The development of custom abutments — first by the wax-and-cast technique, and later with CAD/CAM — allowed the supragingival and equigingival placement of restorative margins. These more accessible restorative margins are more readily cleaned, which may well mitigate the risk associated with cemented restorations.4
So, if we put aside the issue of retained cement, what are the actual indications for screw-retained or cemented restorations? In my experience, the most significant indication for a screw-retained restoration is insufficient restorative space. In order to have a successful cement-retained crown, the abutment should have a minimum height of 4 mm above the margin with minimal taper. Allowing for the space needed for the restoration, there is a minimum required restorative space of 7 mm for a cemented restoration. A screw-retained restoration requires less restorative space because we are not relying on a bonded surface. It is possible to fabricate these restorations with restorative space as little as 4 mm.5
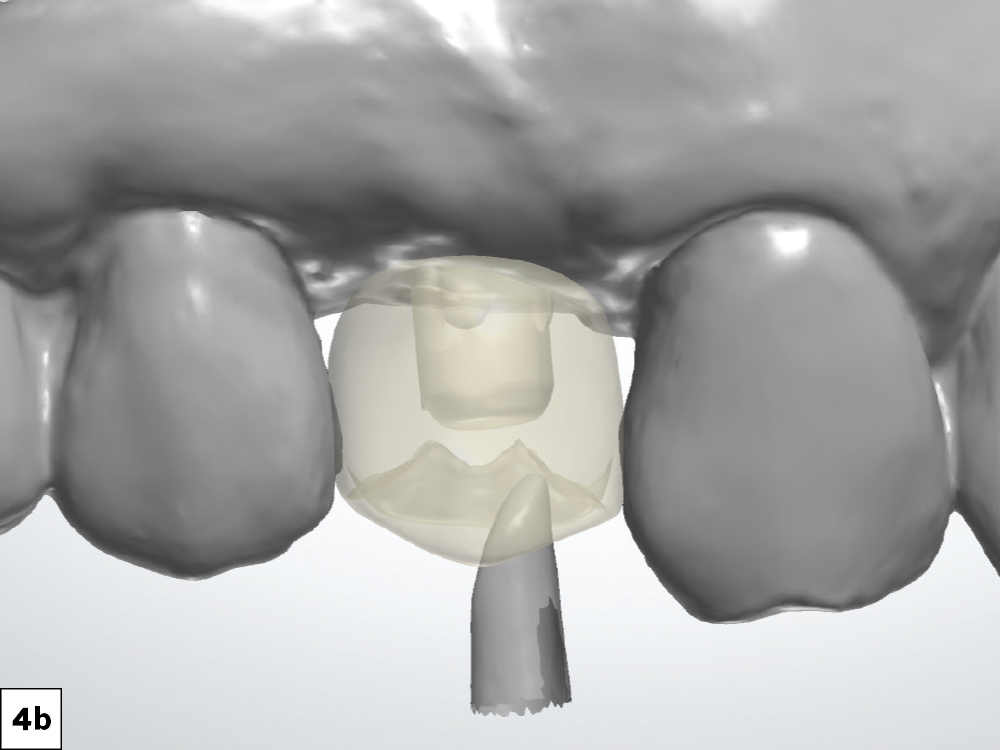
In contrast, the most significant indication for a cement-retained restoration is an implant position that would create a screw access opening through the facial surface of the crown. While we have become more adept at hiding this access opening with composite, there is little question that it can create an esthetic compromise that will make some patients uneasy.
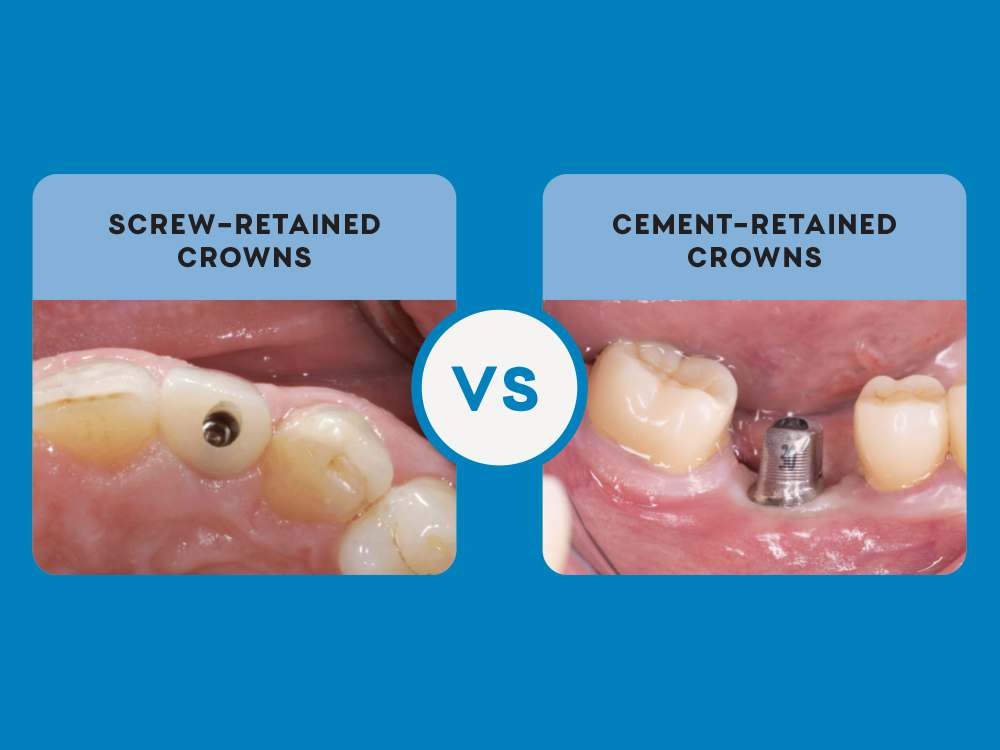
Both restorative options are associated with straightforward clinical and laboratory procedures. Let’s look at two cases that illustrate the predictability of these procedures.
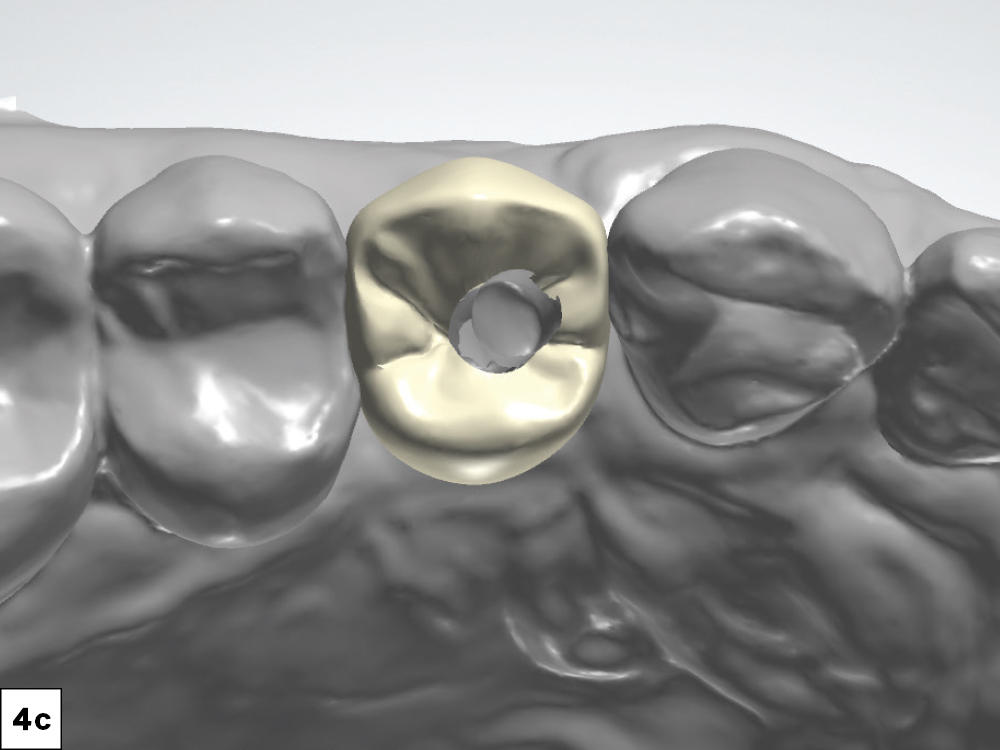
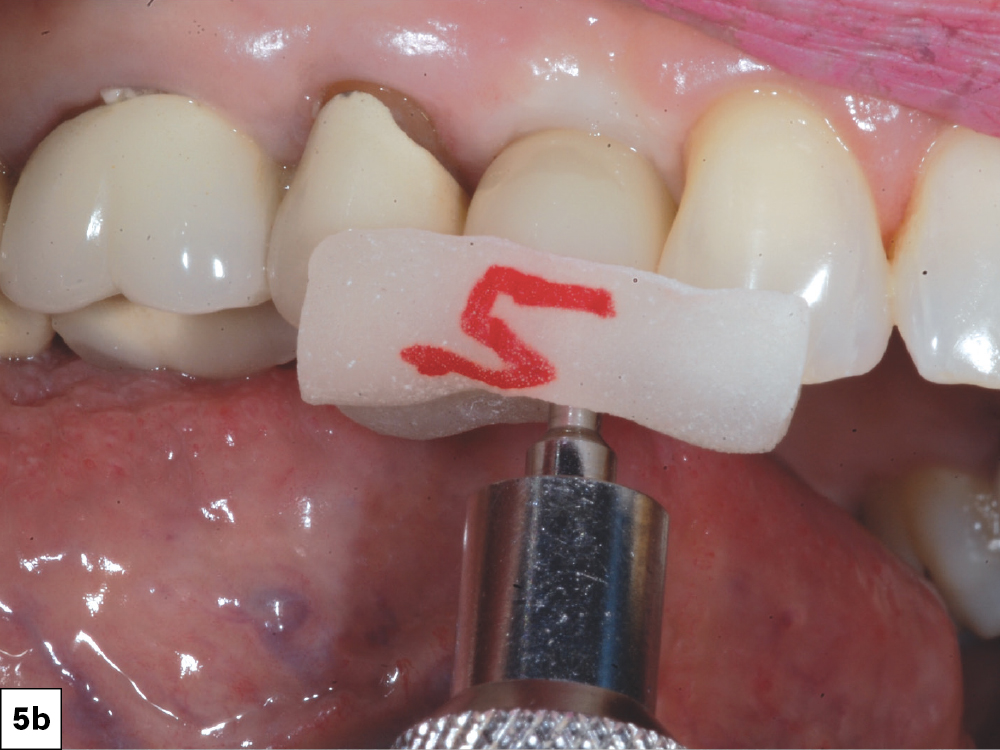
CASE 1: SCREW-RETAINED CROWN
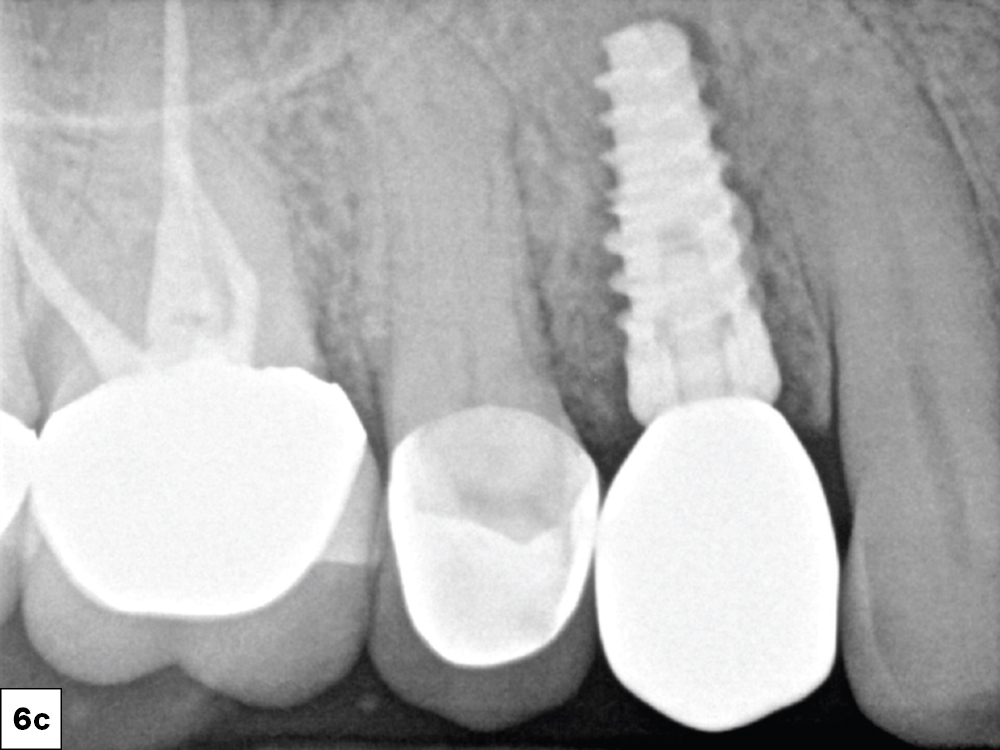
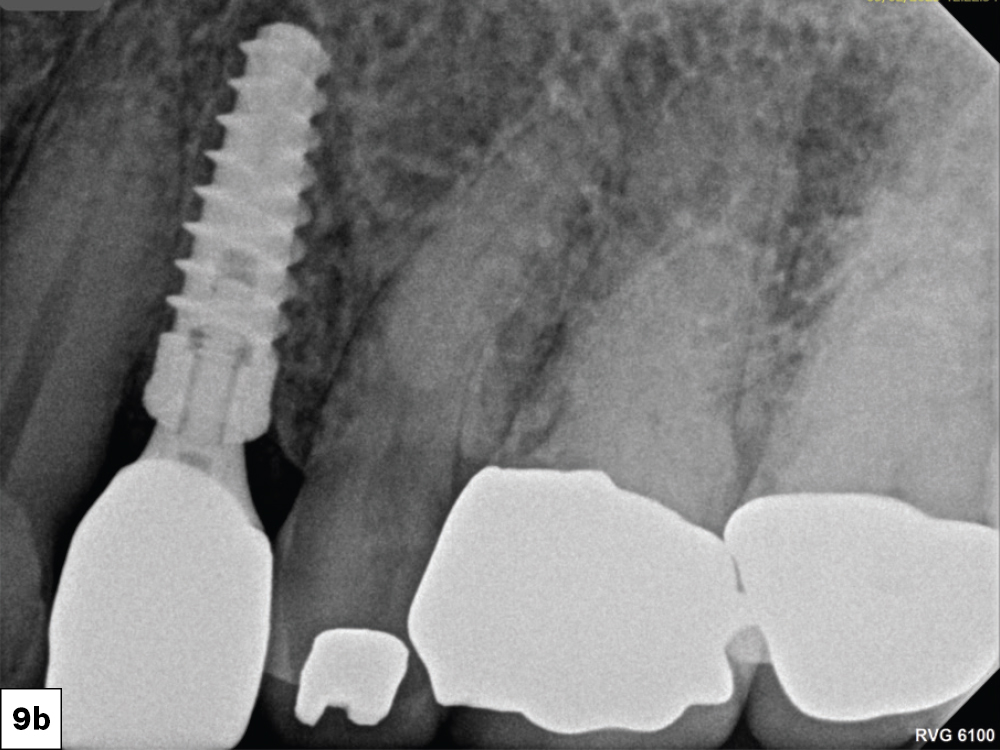
CASE 2: CUSTOM ABUTMENT AND CROWN
CONCLUSION
Both screw-retained and cemented crowns are viable restorative options for the single-tooth implant. The choice depends on specific factors such as restorative space, implant trajectory, as well as the preference of the clinician.
References
-
Raval NC, Wadhwani CP, Jain S, Darveau RP. The interaction of implant luting cements and oral bacteria linked to peri-implant disease: an in vitro analysis of planktonic and biofilm growth — a preliminary study. Clin Implant Dent Relat Res. 2015;17(6):1029-35.
-
Wadhwani C, Schonnenbaum TR, Audia F, Chung KH. In vitro study of the contamination remaining on used healing abutments after cleaning and sterilizing in dental practice. Clin Implant Dent Relat Res. 2016;18(6):1069-74.
-
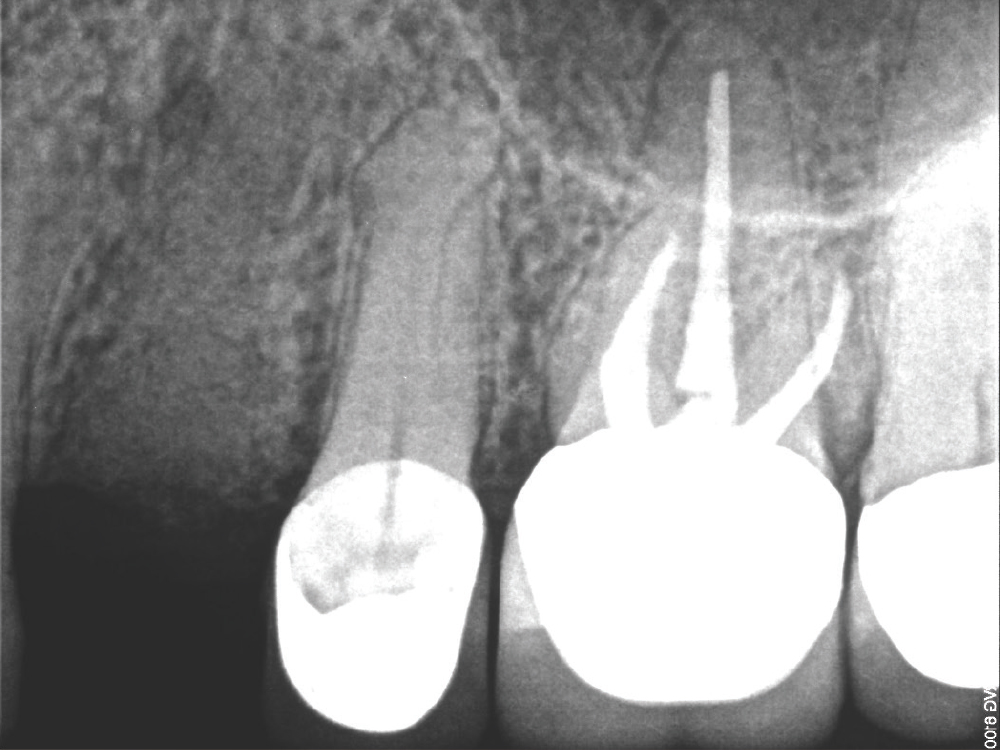
Wadhwani C, Rapoport D, La Rosa S, Hess T, Kretschmar S. Radiographic detection and characteristic patterns of residual excess cement associated with cement-retained implant restorations: a clinical report. J Prosthet Dent. 2012;107(3):151-7.
-
Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):1379-84.
-
Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695-706.